Fluorescence hysteroresectoscopy in the clarifying diagnosis of early endometrial cancer
Objective. To acquaint practitioners with a fluorescence hysteroresectoscopy technique in improving the diagnosis of atypical hyperplasia and early endometrial cancer.Pronin S.M., Matsneva I.A., Maltsagov M.R.
Material and methods. The paper describes the fluorescence hysteroresectoscopy technique performed at the Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia.
Results. Fluorescence hysteroresectoscopy makes it possible to identify the topography of neoplasia and the selectivity of photosensitizer (5-ALA) accumulation in tumor tissue and to perform a targeted biopsy from the maximum fluorescence foci for histological verification.
Conclusion. The introduction of fluorescence hysteroresectoscopy in clinical practice will be able to assess the possibility and success of organ-sparing treatment (hormone therapy) in reproductive-aged women, to monitor the endometrial status, and to timely diagnose a recurrence during or after hormone therapy in patients with early endometrial cancer.
Keywords
Among the lesions of the organs of the female reproductive system, cancer of the uterine corpus is stably the second most common cancer (7.1%), while breast cancer ranks first. According to cancer statistics, endometrial cancer in reproductive-aged women is detected in 5.2% of cases [1, 2]. Due to the extremely rare detection of the disease in young people, the lack of clinical and oncological symptoms allows the outpatient physicians not to take into account and not to consider the patient’s visit to a gynecologist as the reason for the detailed examination aimed at identifying or excluding a possible malignant process. As a rule, early forms of cancer are detected mainly by chance. At the same time, the diagnostics of early stage tumors are already developed and are not complicated, but, unfortunately, demonstrate low sensitivity and accuracy.
Modern Diagnostic Methods
Modern diagnostics of malignant tumors still remain the most important direction in oncology. The chance of cancer cure increases sharply when the oncological disease is detected at the very initial phases of its development.
The diagnostic stage for determining treatment tactics in initial endometrial cancer is a crucial point, allowing the clinician to choose the most optimal treatment option, which may imply both the possibility of dynamic observation and the choice of hormone therapy [3–5] or active surgical tactics [6].
Modern visualization methods (grayscale ultrasound and color Doppler mapping, magnetic resonance imaging, hysteroscopy with separate diagnostic curettage of the uterus) have already revolutionized the diagnostics of endometrial cancer. As a rule, all methods are applied in a complex, the sequence of their application depends on the information content of the previous one [7].
Endoscopic research method takes the leading place in the diagnosis of endometrial cancer. Hysteroscopy allows us not only to determine the presence, localization and prevalence of the tumor process, but also to perform targeted biopsy from a pathologically modified epithelium, as well as to assess the quality of separate therapeutic and diagnostic curettage and the necessity to perform it. Unfortunately, at present, a considerable part of the hysteroscopic and histological studies of the endometrial scraping samples leads to erroneous conclusions. The histological examination of the endometrium samples is the final and decisive diagnostic method, allowing us to determine the nature of morphostructural changes. However, the absence of histological verification does not exclude the presence of neoplasia. The information content of primary curettage in the early forms of the disease, especially in women of reproductive age, is only 78.6% [8].
Fluorescent Diagnosis
In recent years, fluorescence diagnostics (FD) have been recognized as one of the new high-tech methods that have shown their promise in detecting cancer.
To carry out FD we use 5-aminolevulinic acid (5-ALA) drug, its trade name is Alasens (manufactured by Scientific Centre NIOPIC, Moscow). In the laboratory of modifiers, sterile 3% solution of Alasens is prepared. Two hours before FD, 10 ml of 5-ALA is instilled into the uterine cavity. Exposure is 120 minutes (the optimal time interval to determine the high fluorescent contrast between the tumor and the surrounding tissue). In the operating room, under intravenous anesthesia, fluorescent hysteroscopy is performed using a xenon light source (XENON Video Cold Light Fountain) and the Karl Storz video D-light system; the latter provides electronic regulation of the image in white light, 5-ALA-induced fluorescence mode РРIX when excited by blue light (wavelength 380–440nm).
The use of FD is necessary to identify the primary focus or the persistent malignant transformation in the organ tissues. The technique makes it possible to visualize microscopic tumor foci (up to 1 mm) on the seemingly unchanged mucosa, specify their topography, the true areas of the lesion; this visualization is due to the selective accumulation of the previously injected photosensitizer - aminolevulinic acid in the foci. Subsequently, fluorescence (own and induced) is seen on the screen of the video system when exposed to laser radiation in the ultraviolet spectrum [9–10].
5-ALA is not a fluorescent compound, its excessive introduction into the organ tissues leads to the accumulation of its precursor, protoporphyrin-9 (PP-IX), which is able to fluoresce in the red region of the spectrum. The result of its induction in the affected cells is the identification of foci of endometrial cancer by specific fluorescence of PP-IX. The sensitivity and specificity of the method in the initial diagnosis is 99% and 97% [9].
The National Medical Research Centre for Obstetrics, Gynecology and Perinatology in Moscow has been successfully performing organ preservation treatment of early-stage endometrial cancer in young women using individual hormone therapy with subsequent preservation of fertility. The high risk of the disease recurrence after the hormonal treatment (18–37%) requires its timely detection [11].
Fluorescent Hysteroscopy
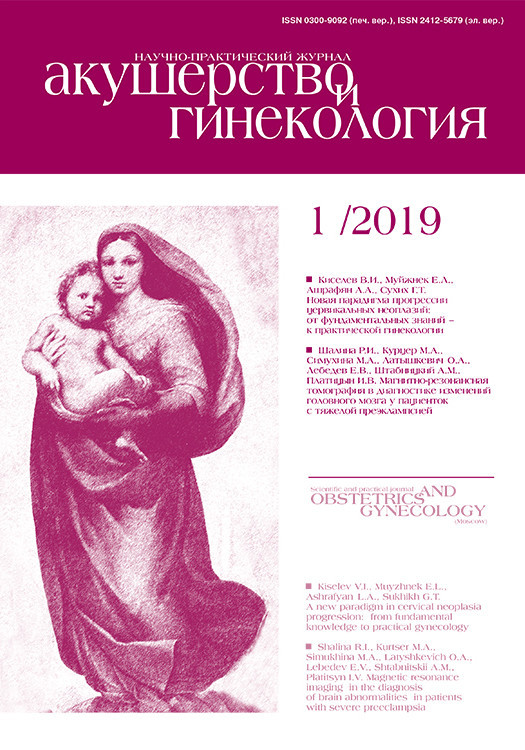
The endoscopic picture of atypical hyperplasia and initial endometrial cancer in natural «white» light is almost indistinguishable (Fig. 1), especially in young women when the lesion is limited. It is extremely difficult to determine the minimal focus among the actively functioning endometrium. To improve the detection of endometrial oncopathology, it is advisable to combine hysteroscopy with FD.
 The successful combination of FD and selective resectoscopy makes it possible to diagnose incurable disease in the process of systemic hormonal therapy and to verify the recurrence of the disease at the early stages in young patients upon completion of the treatment. The method of fluorescent hysteroscopy increases the sensitivity and specificity of biopsy and help visualize the microfoci of endometrial tumor pathology.
The successful combination of FD and selective resectoscopy makes it possible to diagnose incurable disease in the process of systemic hormonal therapy and to verify the recurrence of the disease at the early stages in young patients upon completion of the treatment. The method of fluorescent hysteroscopy increases the sensitivity and specificity of biopsy and help visualize the microfoci of endometrial tumor pathology.
It is necessary to keep in mind the “false glow” phenomenon resulting from the accumulation of the photosensitizer in the decidually modified uterine mucosa, due to pronounced drug pathomorphosis and hormone therapy, which can be confused by the doctor. The sensitivity of this fluorescence method during the treatment is 100%, the specificity is 67% [9].
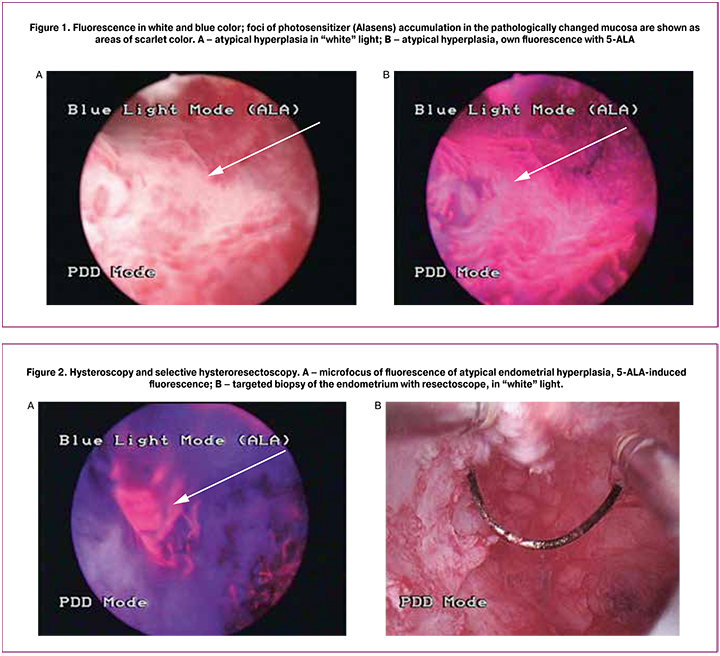
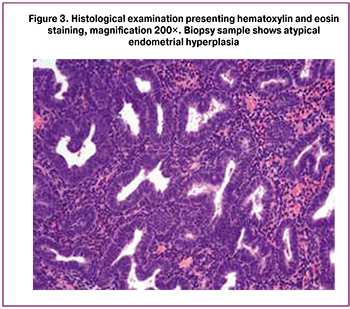
The combination of Alasens FD with selective hysteroresectoscopy (Fig. 2) might minimize the number of false-positive biopsy results; it is also possible to estimate the affected areas of the uterine mucosa and perform targeted biopsy (Fig. 3).
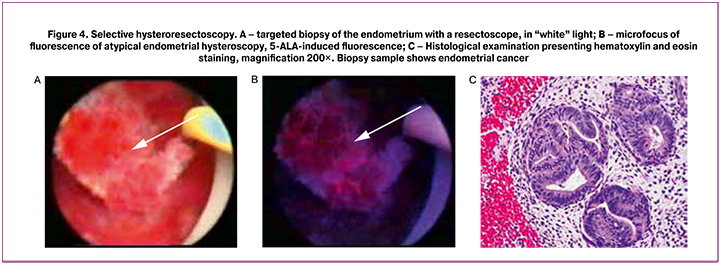
The revealed correlation of the FD results with the data of histological examination determines the FD specificity. Biopsy should be performed using a loop electrode with resectoscope to obtain sufficient material for histological examination, since the material obtained with endoscopic “forceps” is usually not informative for histological examination due to its small size (1.5–2 mm) (Fig. 4).
Conclusions
The introduction of the technique into clinical practice allows:
- assessment of the possibility and success of organ-sparing treatment (hormone therapy) in curing early-stage endometrial cancer in women of reproductive age;
- monitoring the state of the endometrium in patients with early-stage endometrial cancer during and after performing individual hormone therapy;
- identification of the incurable disease or early recurrence of the disease.
References
- Каприн А.Д., Старинский В.В., Петрова Г.В., ред. Злокачественные новообразования в России в 2016 году (заболеваемость и смертность). М.: МНИОИ им. П.А. Герцена - филиал ФГБУ «НМИЦ радиологии» Минздрава России; 2018. [Kaprin A.D., Starinsky V.V., Petrova G.V., ed. Malignant neoplasms in Russia in 2016 (morbidity and mortality). M.: Moscow them. P.A. Herzen - a branch of the Federal Research Center for Radiology Research Center of the Ministry of Health of Russia; 2018. (in Russian)]
- Edometrial Cancer Treatment (PDQ). National Cancer Institute. 23 April 2014. Archived from the original on 3 September 2014. Retrieved 3 September 2014.
- Gunderson C.C., Fader A.N., Carson K.A., Bristow R.E. Oncologic and reproductive outcomes with progestin therapy in women with endometrial hyperplasia and grade 1 adenocarcinoma: a systematic review. Gynecol. Oncol. 2012; 125(2): 477-82.
- Gonthier C., Walker F., Luton D., Yazbeck C., Madelenat P., Koskas M. Impact of obesity on the results of fertility-sparing management for atypical hyperplasia and grade 1 endometrial cancer. Gynecol. Oncol. 2014; 133(1): 33-7.
- Pal N., Broaddus R.R., Urbauer D.L., Balakrishnan N., Milbourne A., Schmeler K.M. et al. Treatment of low-risk endometrial cancer and complex atypical hyperplasia with the levonorgestrel-releasing intrauterine device. Obstet. Gynecol. 2018; 131(1): 109-16.
- Loiacono R.M., Trojano G., Del Gaudio N., Kardhashi A., Deliso M.A., Falco G. et al. Hysteroscopy as a valid tool for endometrial pathology in patients with postmenopausal bleeding or asymptomatic patients with a thickened endometrium: hysteroscopic and histological results. Gynecol. Obstet. Invest. 2015; 79(3): 210-6.
- PRACTICE BULLETIN clinical management guidelines for obstetrician-gynecologists. Number 149, April 2015.
- Ашрафян Л.А., Киселев В.И. Опухоли репродуктивных органов (этиология и патогенез). М.: Издательство Дмитрейд График Групп; 2007. [Ashrafyan L.A., Kiselev V.I. Tumors of the reproductive organs (etiology and pathogenesis). M .: Publishing Dmitreyd Grafik Group; 2007. (in Russian)]
- Серова Л.Г. Флуоресцентная диагностика у больных с предопухолевой и опухолевой патологией эндометрия: автореф. дисс. … канд. мед. наук. М.; 2012. [Serova L.G. Fluorescent diagnostics in patients with pretumor and tumor endometrial pathology: author. diss. ... Cand. honey. sciences. M .; 2012. (in Russian)]
- Чиссов В.И., Филоненко Е.В., ред. Флюоресцентная диагностика и фотодинамическая терапия в клинической онкологии. Монография. М.: Триумф; 2012. [Chissov V.I., Filonenko E.V., ed. Fluorescent diagnostics and photodynamic therapy in clinical oncology. Monograph. M .: Triumph; 2012. (in Russian)]
- Новикова О.В., Новикова Е.Г., Лозовая Ю.А., Чулкова О.В., Пронин С.М. Самостоятельная гормонотерапия как альтернатива хирургическому лечению предрака и начального рака эндометрия у пациенток репродуктивного возраста. Онкогинекология. 2015; 3: 25-33. [Novikova O.V., Novikova E.G., Lozovaya Yu.A., Chulkova O.V., Pronin S.M. Self hormone therapy as an alternative to surgical treatment of precancer and initial endometrial cancer in patients of reproductive age. Oncogynecology. 2015; 3: 25-33. (in Russian)]
Received 20.03.2018
Accepted 20.04.2018
About the Authors
Pronin, Stanislav M., PhD, oncologist, obstetrician-gynecologist, senior Researcher of Department of Innovative Oncology and Gynecology,National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Health of Russia.
117997, Russia, Moscow, Ac. Oparina str. 4. Tel.: +79161463483. Psm_doc@mail.ru
Matsneva, Irina A., student of the 6th year medical faculty, I.M. Sechenov First Moscow State Medical University (Sechenov University), Ministry of Health of Russia.
119435, Russia, Moscow, Bolshaya Pirogovskaya str. 2, p. 4. Tel.: +79153345980. E-mail: via.white.doc@gmail.com
Maltsagov, Muslim R., clinical resident of 1th year of National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. Tel.: +79267513040. E-mail: terekman94@gmail.com
For citations: Pronin S.M., Matsneva I.A., Maltsagov M.R. Fluorescence hysteroresectoscopy in the clarifying diagnosis of early endometrial cancer. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (1): 104-8. (in Russian)
http://dx.doi.org/10.18565/aig.2019.1.104-108