Remote monitoring of pregnant women: the Orenburg experience
Savinova T.L., Grudkin A.A., Ermolaeva I.V., Kundik T.A., Zingerman B.V., Abu Al Laban N.A., Borodin R.A., Yakovleva I.V., Kholin A.M., Shuvalova M.P., Sukhikh G.T.
Background: Patient-centered medical care is one of the most promising areas in the development of digital healthcare, including remote monitoring of pregnant women’s health, since it meets the demand for improved access and quality of medical services.
Objective: To analyze the experience of using a system of remote monitoring and control of pregnancy, including the possibility of monitoring high-risk pregnancies, to evaluate the use of remote monitoring of pregnant women’s health using a cloud-based digital platform and to assess the potential for its future implementation based on prospective follow-up in Orenburg.
Materials and methods: The remote monitoring system for pregnancy health is a cloud-based digital platform, web application, and symptom-based surveillance scripts. The qualitative study was based on prospective follow-up of 2,488 pregnant women and 489 women who gave birth. A total of 18,206 questions asked by pregnant women to their attending physicians and 4,013 notifications (‘alarms’) were studied. The notifications were generated using the parameters entered by pregnant women on the Medsenger.AI remote monitoring platform, provided by AyPat LLC, in collaboration with the Orenburg Clinical Perinatal Centre and seven antenatal clinics in Orenburg. The data cover the period from 17 October 2023 to 20 May 2024.
Results: The system for remote monitoring of pregnant women’s health has received high marks from users. Professionals who were introduced to the system appreciated its usefulness in existing routine work. The study demonstrated the importance, convenience and accessibility to the patients. The time spent by the physician on participating in remote monitoring was assessed. There was a high demand for remote monitoring among pregnant women: 81% of participants used the platform, 86% of those who used it indicated that it was useful and convenient. The participant feedback score was 4.82 (out of 5).
Conclusion: A comprehensive scenario for remote monitoring of pregnant women has demonstrated that both patients and physicians are receptive to its integration into routine practice. The proposed tool can be used in the management of pregnancy at the primary specialist health care level.
Authors’ contributions: Savinova T.L., Sukhikh G.T. – developing the study concept; Grudkin A.A. – developing the scenario, organizing the monitoring; Ermolaeva I.V. – developing and analyzing the use of the monitoring scenario, medical supervision of the monitoring project; Kundik T.A. – developing the monitoring scenario, guiding and supporting the doctors who conducted the monitoring; Zingerman B.V. – scientific supervision of the project, drafting the text of the article; Abu Al Laban N.A. – software development, user support; Borodin R.A. – software development, analysis of the received materials; Yakovleva I.V., Kholin A.M. – expert analysis of the results, editing the text of the article, literature selection; Shuvalova M.P. – expert analysis of the results, editing the text of the article.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: This study was a part of a project supported by the Foundation for Assistance to Small Innovative Enterprises in Science and Technology (832GRNTIS5/81931); it was carried out using the specialised platform Medsenger.AI (Certificate of State Registration of Computer Program No. 2019619421).
Patient Consent for Publication: Patients signed informed consent to join the remote monitoring program.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Savinova T.L., Grudkin A.A., Ermolaeva I.V., Kundik T.A., Zingerman B.V., Abu Al Laban N.A., Borodin R.A., Yakovleva I.V., Kholin A.M., Shuvalova M.P., Sukhikh G.T.
Remote monitoring of pregnant women: the Orenburg experience.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (11): 162-172 (in Russian)
https://dx.doi.org/10.18565/aig.2024.212
Keywords
The development of telemedicine technologies, including remote medical monitoring, is a priority for the strategic development of the healthcare system [1]. In accordance with the Order of the Ministry of Health of the Russian Federation dated November 30, 2017 No. 965n “On approval of the order of organization and provision of medical care with the use of telemedicine technologies” remote monitoring can be defined as the continuous observation of the patient’s health indicators by a healthcare provider through the analysis of the data recorded with the use of medical devices, the possibility of data processing and emergency response when there is a critical deviation of the patient’s health indicators from the limit values.
A federal pilot project [2, 3] on remote monitoring of patients with arterial hypertension and diabetes mellitus is conducted within the framework of the Order of the Government of the Russian Federation dated December 09, 2022 No. 2276; this study contributes to the study of monitoring of pregnant women.
The relevance of the use of remote monitoring systems by pregnant women is determined by the possibility of expanding access to medical services during the period of restrictions on physical visits to medical institutions (e.g., restrictions associated with COVID-19 virus), timely tracking of risk factors for complications, reducing the importance of the territorial factor, and the ability to form a positive experience of interaction with the health care system. Thus, the aim of this study was to evaluate the effectiveness and efficiency of remote monitoring of pregnant women’s health using a cloud-based digital platform, as well as the potential for its further implementation based on prospective follow-up of pregnant women in Orenburg.
Materials and methods
The study included records of 2,904 pregnant women registered in the system. The recruitment was conducted from October 2023 to May 2024 at the Orenburg Clinical Perinatal Center as part of the project entitled “We are always near”.
The Orenburg Clinical Perinatal Centre provides a full cycle of highly qualified medical care to women with gynecological diseases, pregnant women, women in labor, women who have given birth and newborns; the structure of the Orenburg Clinical Perinatal Centre includes a 24-hour hospital with 370 beds, a day care hospital, seven women’s clinics serving more than 230,000 women in Orenburg; about 6,000 births take place each year.
The study included the following stages: 1) development and coordination of the methodology and tools for remote monitoring by a working group consisting of obstetrician-gynecologists and IT specialists from IPat LLC who provided the Medsenger.AI remote monitoring platform (April–October 2023); 2) pilot testing of the developed methodology (October–December 2023); 3) implementation of the system from January 2024 in seven women’s clinics in Orenburg; 4) evaluation of the acceptance of the remote monitoring application.
The system employed 137 healthcare workers (70 obstetrician-gynecologists, 64 midwives, a psychologist, a social worker and a lawyer). The Orenburg Clinical Perinatal Center was provided with 30 blood pressure monitors and 3 cardiotocographic monitors.
The Medsenger.AI cloud-based platform provided the technological tool for remote monitoring of pregnant women’s condition by the attending physician. The patient flow management, the establishment of connections for monitoring and quality control of case management were among the basic administrative functions. Chat, file-sharing and video-calling capabilities were used by doctors; the formats were developed for mobile applications and in the web-version, a mechanism for connecting intelligent agents and specialized monitoring scenarios was developed.
There were some scenarios for groups of patients with the confirmed diagnosis or in a certain clinical situation, which included a set of automatic reminders and questionnaires for the patient, sent according to the schedule recommended by the doctor, based on the Order of providing medical care in obstetrics and gynecology and clinical recommendations.
The scenario of remote monitoring included the following steps: 1) weekly newsletters about the pregnant woman’s condition and fetal development with graphic images; 2) preparation memos and reminders to undergo medical examinations and procedures; 3) informational letters with materials about lifestyle, nutrition, preparation for childbirth, etc. (there are 82 letters in the developed scenario); 4) prescription patterns of medicines and reminders to take them (the scenario includes 13 patterns of the most frequent prescriptions, which can be supplemented by the doctor); 5) monitoring of indicators with reminders to take measurements: body weight, blood pressure, pulse should be taken once a week, body temperature should be taken once a day; 6) a questionnaire with a list of undesirable symptoms in pregnancy, the results of which are used to send a notification to the doctor and recommendations to the patient (e.g., calling an ambulance or a therapist at home); 7) questionnaire with symptoms of acute respiratory viral infection (ARVI), memo with recommendations; 8) possibility to connect an automatic blood pressure monitor that sends measurements directly to the medical record on the platform.
When the doctor was connected, he/she could choose an additional scenario: 1) to monitor gestational diabetes mellitus (GDM), which includes monitoring of the following indicators: fasting glucose – once a day, glucose after meals – three times a day, protein in urine – three times a month; when indicators are out of the reference range, a notification is sent to the physician requiring a response, a memo with information is sent to the patient; 2) to monitor arterial hypertension with the control of blood pressure and pulse three times a day; a questionnaire with threatening symptoms in arterial hypertension in pregnant women; a demanding notification is sent to the doctor (“alarm”), the patient is sent information about pre-eclampsia.
The developed scenario provided the possibility of connecting Russian specialized blood pressure monitor Hemodin-AKSMA with automatic data transfer and a system of remote cardiotocography (CTG) monitoring developed by the Russian BIPULS LLC, providing remote transfer of fetal CTG directly into the communication channel with the doctor on the Medsenger.AI platform.
The pregnant woman is enrolled in the remote monitoring program during a visit to the women’s clinic and after signing a consent form.
The quality was assessed by the patients using a questionnaire at the end of the monitoring, with scores on a 5-point scale; additionally, a one-time detailed survey of physicians and pregnant women about service and satisfaction was conducted.
Results
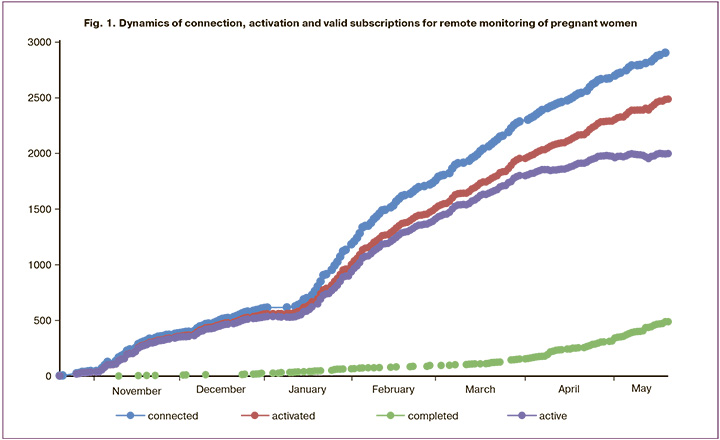
As a result, 80.8% of women successfully connected to remote monitoring, 416 women did not activate the monitoring connection, i.e. 13.5% of patients showed “passive refusal”. A total of 5.7% of women actively opposed to being connected to monitoring. There were the following reasons for refusal: language barrier - 2.6%, lack of computer literacy or smartphone - 2.2%, other - 0.9%. Thus, 2488 women who activated their monitoring channel were included in the study, 91.7% of pregnant women activated their monitoring channel almost immediately (mostly on the same day). The remaining 8.3% were connected when there was a need for remote communication with a physician (from 1 to 4 months). A total of 489 pregnant women have completed the monitoring process due to the end of the gestation period. The dynamics of connection, activation and termination of remote monitoring are shown in Figure 1.
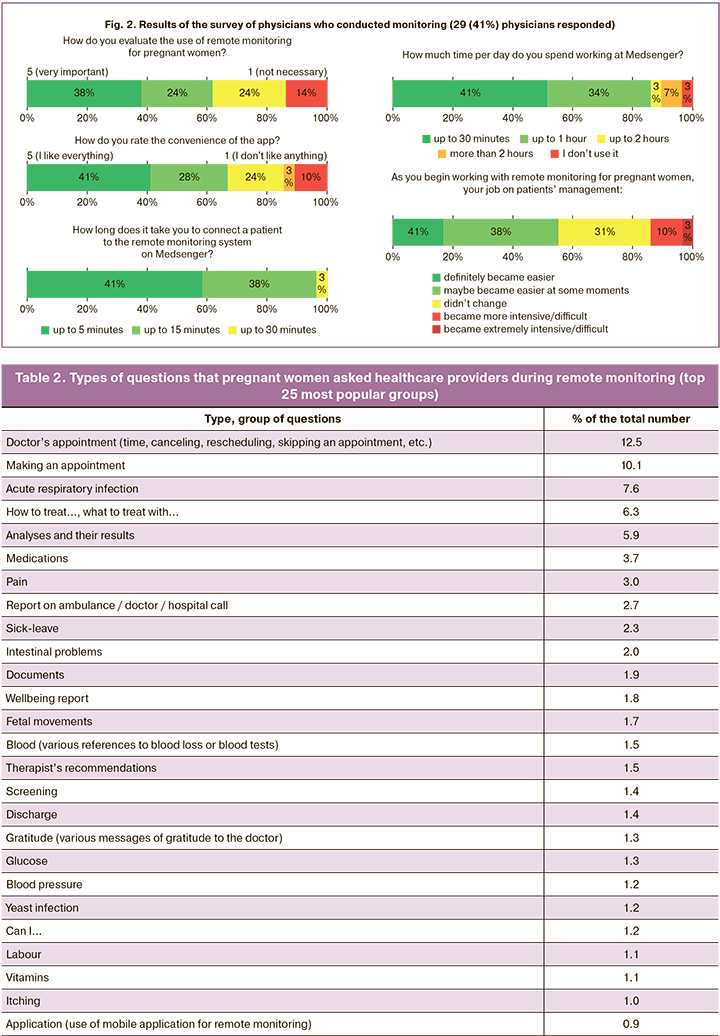
Physician’s workload. In this study, 71% of the remote monitoring participants were managed jointly by an obstetrician-gynecologist and midwife and 29% by the obstetrician-gynecologist alone. The number of patients per physician ranged from 5 to 104 (median 33, mean 42). A quarter of the doctors connected remotely managed 50 or more patients. An estimate of time costs is presented in Figure 2.
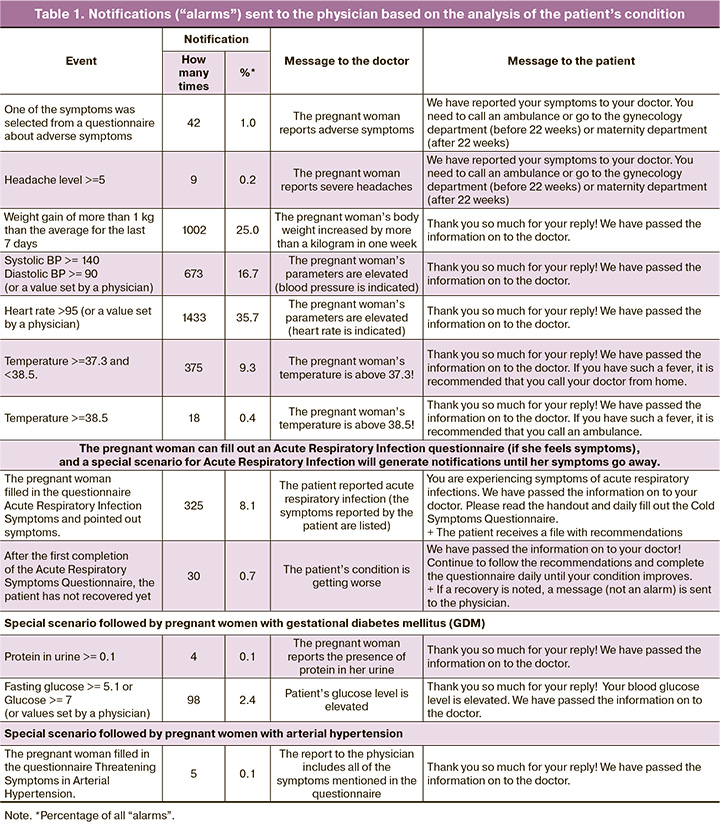
Questions from pregnant women and notifications from the system about their condition (“alarms”) form an additional workload for the physician during remote monitoring. A total of 4,013 “alarms” were received from the system during the analyzed period (Table 1); pregnant women asked 18,206 questions (Table 2); health workers (doctors and midwives) sent 22,352 messages (answers, recommendations, etc.) to pregnant women, which exceeds the total number of questions and “alarms” (22,219).
On average, there were 6.3 questions, 1.4 “alarms,” and 7.7 messages from healthcare providers per pregnant woman involved in monitoring. Given that pregnant women had different monitoring periods and durations, a more informative indicator is the average per “person-day” of monitoring: 0.080 questions, 0.017 alarms, and 0.099 responses from healthcare providers. The study found higher activity for patients who had already completed remote monitoring, with an average of 9.8 questions and 2.8 “alarms” and 11.1 messages from healthcare providers on average for each pregnant woman.
The number of questions posed to the physician demonstrated considerable variation. During the observation period, approximately half of the pregnant women did not inquire about any aspect of their care. However, three women asked more than 100 questions (116, 141, and 183). “Alarms” were generated for only 18% of pregnant women participating in monitoring. However, there were 45 patients (1.5%) who generated 20 or more “alarms” (maximum 104). This group of patients was the most active in asking questions to the physician, with an average of 27. The system also generated a notification to the patient for the “alarm” sent to the doctor. There were four pregnant women who had a large number of alarms generated (e.g., 76) but they did not ask the physician a single question, even though they had the opportunity to do so.
Midwife’s workload. The variation in the number of messages written by midwives is considerable (from 1 to 498). A total of 24 midwives actively participated in the study, providing responses to organizational queries such as appointment scheduling, test results, and the timing and order of examinations. These responses accounted for a minimum of 40% of the whole data set (Table 2).
Analysis of questions to the physician. Among the 18,206 questions posed to the doctor, the largest number related to organizational issues (appointments, tests, screenings, sick leave, and various paperwork). Less than 1% of questions were about the mobile application itself. About 2/3 of the questions asked were related to a wide range of issues connected with the health, condition and lifestyle of the pregnant woman.
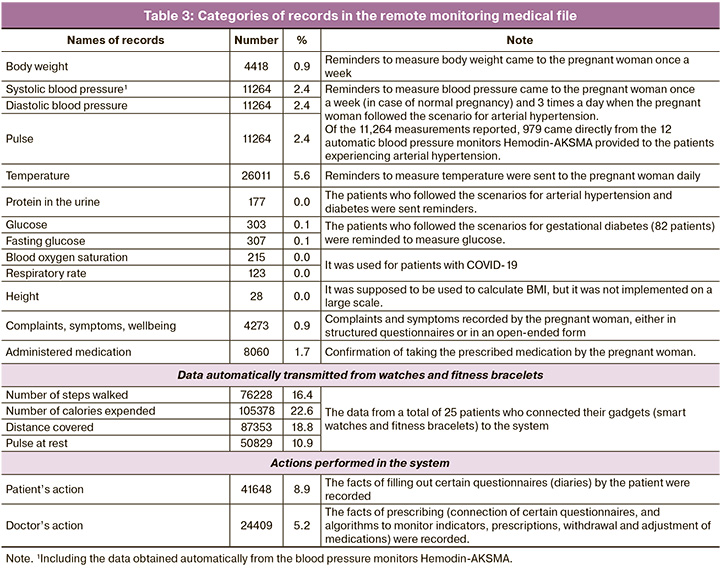
Exchange of information. Medical images including photos of medical documents were mainly exchanged: 800 images were sent by patients and 133 by healthcare providers. A total of 87 files and documents were sent by patients, while 39 were sent by healthcare providers. During the analyzed period, 465,795 records were entered into the medical records system.
Special scenarios in complicated pregnancies. The additional control scenario for arterial hypertension was used in cases of 132 patients, and the additional control scenario for GDM was applied in cases of 82 patients. The Anxiety Symptoms in Pregnancy questionnaire was completed 55 times, the Threatening Symptoms in Arterial Hypertension questionnaire was completed 5 times, and the Symptoms of Acute Respiratory Syndrome questionnaire was completed 365 times.
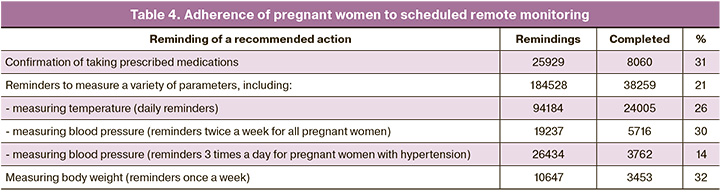
Patient adherence to remote monitoring. The patients followed about one-third of the incoming reminders; in situations where reminders came more frequently, such as for pregnant women with arterial hypertension, the compliance of the patients was lower (Table 4).
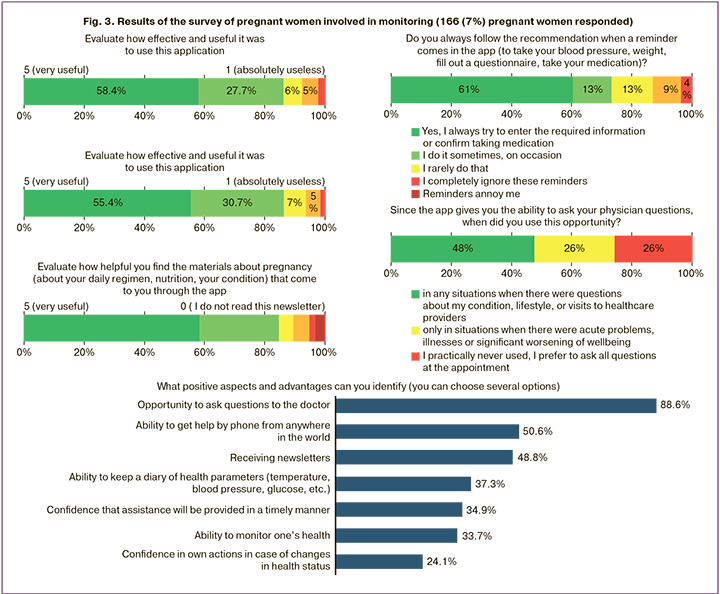
User assessment. The average rating score was 4.82. Of the respondents who completed the survey, 46 indicated a rating of “5”, with 20 providing additional comments that were also positive. One pregnant woman rated the item with a “4”, stating, “Everything is awesome”. One pregnant woman rated the item with a “3”, and two respondents rated it with a “2” (did not write any critical comments). The results of the patient survey are shown in Figure 3 and the physician survey are shown in Figure 2.
Discussion
The main findings of this study
Specialized monitoring scenarios help patients to accurately follow administrations and adhere to the doctor’s recommendations, involving the physician only in cases that require attention. The remote monitoring and support of pregnant women during a normal pregnancy is a significant and viable aspect of maternal care that is in high demand.
An important result of this study is the estimate of the average cost of physician’s attention during mass remote monitoring of pregnant women: each pregnant woman during mass monitoring required physician’s attention on average once every 10 days. A physician who is responsible for monitoring the health of 50 patients simultaneously must communicate with five of them on a daily basis. The workload is also shared between the doctor and the midwife. Thus, in the present study, midwives answered 19% of the questions, while the question classification shown in Table 3 demonstrates the potential for midwives to increase their responses to about 40% of the questions.
The time spent on monitoring was not measured, but the physicians provided subjective estimates in a survey (Fig. 2). A total of 51.7% of physicians spent up to 30 minutes per day on monitoring activities, and 35.7% of doctors spent up to an hour on these tasks. A more detailed analysis showed that physicians with 50 or more patients had this type of response. The introduction of remote monitoring was perceived as a significant improvement in the work of 17% of doctors, who indicated that it has “definitely” made their work easier; 38% of doctors reported that remote monitoring made their work “easier in some moments”.
Strengths and limitations
It is noteworthy that 2/3 of the records collected in the project’s local medical database came from fitness bracelets and smart watches that 25 pregnant women (less than 1%) independently connected to the remote monitoring platform. These gadgets are not medical devices and their use in healthcare practices is not regulated, but the results of the study demonstrate the interest of the patients and make health behavior relevant.
The market for remote monitoring devices with automatic data transmission is quite small. The practice of measurement is of greater importance than the act of automatic data transmission. The experience of this project demonstrates that the commitment to perform regular measurements is not influenced by the device the patient uses. Adherence is greatly improved by the use of the devices that automatically measure human parameters.
Comparison with existing studies
Attention to remote monitoring of pregnant women’s health is of interest to researchers in terms of clinical practice, timely decision making, compensating for the shortage of medical personnel, geographical characteristics and patient needs [6]. Research trends in this area are reflected in the present study. Remote monitoring is considered to be a safe, effective and less costly [7] in complicated pregnancies as a way to interact with the patient [8, 9], which helps to reduce the number of visits to the doctor [10]. A considerable amount of current research has focused on pregnant women with arterial hypertension, and these studies demonstrate the importance of the fastest possible response to the changing clinical picture and regular monitoring of blood pressure in the pregnant woman [11, 12]. In the present study, this was achieved through the introduction of an additional monitoring scenario. Furthermore, research has indicated that pregnant women have reported positive experiences, including emotional benefits when using digital platforms. Some studies have noted the importance of remote monitoring in the post pandemic period, emphasizing the importance of a personal visit to the physician [15]. The effectiveness and potential of this technology are demonstrated by monitoring systems which allow the involvement of a physician only when necessary [16].
Clinical interpretation of the study
The technology used for remote monitoring of pregnant women is currently a subject of active research and development, with ongoing data accumulation and analysis. It is important to note that remote monitoring, defined as regular measurement and entry into the system, including automatically transmitted indicators, is perceived as a disadvantage by patients. Only 30% of pregnant women expressed satisfaction with this possibility (Fig. 3). If the patient did not receive additional bonuses, she quickly discontinued participation [4]. There were the following bonuses in the conducted study: the opportunity to ask their physicians questions (appreciated by 88% of pregnant women); regular (2–3 times a week) obtaining useful informational materials (approved by more than 80% of pregnant women); convenient graphs and dynamic curves of indicators that can be viewed by both the patient and the attending physician; reaction to deviations in indicators and status, including notifications to the patient that a message to the physician has already been sent.
The most effective tool for remote monitoring of physiological parameters will be wearable devices. Patient adherence will remain inadequate without their use.
Information support for pregnant women becomes an important part of remote monitoring; it is included in the monitoring scenario, and it enhances the effectiveness of the monitoring process and improves its perception.
Conclusion
The demand for remote monitoring among pregnant women is evident; similarly, physicians view this technology as an effective and useful tool. Remote monitoring can be useful for all pregnant women, and special scenarios of profound monitoring can be used in case of pregnancy complications. The possibility of continuous remote communication with the attending physician is the most important part of remote monitoring of pregnant women. The absence of feedback in parameter monitoring results in the rejection of its use.
References
- Федеральный закон от 21 ноября 2011 г. № 323-ФЗ «Об основах охраны здоровья граждан в Российской Федерации» (ст. 36.2). [Federal Law of November 21, 2011 No. 323-FZ "On the Basics of Health Protection of Citizens in the Russian Federation" (Article 36.2). (in Russian)].
- Постановление Правительства Российской Федерации от 09.12.2022 № 2276 «Об установлении экспериментального правового режима в сфере цифровых инноваций и утверждении Программы экспериментального правового режима в сфере цифровых инноваций по направлению медицинской деятельности с применением технологий сбора и обработки сведений о состоянии здоровья и диагнозов граждан в отношении реализации инициативы социально-экономического развития Российской Федерации "Персональные медицинские помощники». [Decree of the Government of the Russian Federation of 09.12.2022 No. 2276 "On the establishment of an experimental legal regime in the field of digital innovations and approval of the Program of an experimental legal regime in the field of digital innovations in the field of medical activities using technologies for collecting and processing information about the state of health and diagnoses of citizens in relation to the implementation of the initiative socio-economic development of the Russian Federation" Personal medical assistants". (in Russian)].
- Постановление Правительства Российской Федерации от 28.12.2022 № 2469 «О реализации пилотного проекта по дистанционному наблюдению за состоянием здоровья пациента с использованием информационной системы (платформы) "Персональные медицинские помощники». [Decree of the Government of the Russian Federation of 28.12.2022 No. 2469 "On the implementation of a pilot project for remote monitoring of the patient's health using the Personal Medical Assistants information system (platform)".(in Russian)].
- Демкина А.Е., Ловцева В.А., Дубровина К.С., Асланова Т.М., Рогожкина Ю.А., Карпова И.А., Зингерман Б.В., Бородин Р.А., Исаева А.В., Коробейникова А.Н. Апробация самостоятельного дистанционного мониторинга у беременных группы риска. Врач и информационные технологии. 2023; 4: 66-78. [Demkina A.E., Lovtseva V.A., Dubrovina K.S., Aslanova T.M., Rogozhkina Yu.A., Karpova I.A., Zingerman B.V., Borodin R.A., Isaeva A.V., Korobeynikova A.N. Approbation of self-remote monitoring in high-risk pregnant women. Medical doctor and information technology. 2023; (4): 66-78. (in Russian)]. https://dx.doi.org/10.25881/18110193_2023_4_66.
- Есин И.В., Перецманас Е.О., Зингерман Б. В., Абу Аль Лабан Н.А., Хазбулатов А.Т., Бородин Р.А. Современные технологии телемедицинского мониторинга пациентов с заболеваниями позвоночника в условиях пандемии. Врач и информационные технологии. 2023; 1: 4: 4-15. [Esin I.V., Perethmanas Е.О., Zingerman B.V., Abu Al Laban N.A., Khazbulatov A.T., Borodin Р.А. Modern technologies of telemedical monitoring of patients with spinal diseases during pandemic. Medical doctor and information technology. 2023; 1: 4: 4-15. (in Russian)]. https://dx.doi.org/10.25881/18110193_2023_1_4.
- Таскина В.Ю., Демкина А.Е., Владзимирский А.В., Морозов С.П., Шкода А.С., Газашвили Т.М., Яковлева И.В., Шувалова М.П., Холин А.М. Дистанционное диспансерное наблюдение в акушерстве: состояние проблемы и перспективы. Акушерство и гинекология. 2021; 9: 12-20. [Taskina V.Yu., Demkina A.E., Vladzimirsky A.V., Morozov S.P., Shkoda A.S., Gazashvili T.M., Yakovleva I.V., Shuvalova M.P., Kholin A.M. Tele-follow-up in obstetrics: the problem state and prospects. Obstetrics and Gynecology. 2021; (9): 12-20(in Russian)]. https://dx.doi.org/10.18565/aig.2021.9.12-20.
- Xydopoulos G., Perry H., Sheehan E., Thilaganathan B., Fordham R., Khalil A. et al. Home blood-pressure monitoring in a hypertensive pregnant population: cost minimization study. Ultrasound Obstet. Gynecol. 2019; 53(4): 496-502. https://dx.doi.org/10.1002/uog.19041.
- Bekker M.N., Koster M.P.H., Keusters W.R., Ganzevoort W., de Haan-Jebbink J.M., Deurloo K.L. et al. Home telemonitoring versus hospital care in complicated pregnancies in the Netherlands: a randomised, controlled non-inferiority trial (HoTeL). Lancet Digit. Health. 2023; 5(3): e116-e124. https://dx.doi.org/10.1016/S2589-7500(22)00231-X.
- Zizzo A.R., Hvidman L., Salvig J.D., Holst L., Kyng M., Petersen O.B. Home management by remote self-monitoring in intermediate- and high-risk pregnancies: A retrospective study of 400 consecutive women. Acta Obstet. Gynecol. Scand. 2022; 101(1): 135-44. https://dx.doi.org/10.1111/aogs.14294.
- Marko K.I., Ganju N., Krapf J.M., Gaba N.D., Brown J.A., Benham J.J. et al. A Mobile Prenatal Care App to Reduce In-Person Visits: Prospective Cotrolled Trial. JMIR Mhealth Uhealth. 2019; 7(5): e10520. https://dx.doi.org/10.2196/10520.
- Холин А.М., Муминова К.Т., Балашов И.С., Ходжаева З.С., Боровиков П.И., Иванец Т.Ю., Гус А.И. Прогнозирование преэклампсии в первом триместре беременности: валидация алгоритмов скрининга на российской популяции. Акушерство и гинекология. 2017; 8: 74-84. [Kholin A.M., Muminova K.T., Balashov I.S., Khodzhaeva Z.S., Borovikov P.I.,Ivanets T.Yu., Gus A.I. First-trimester prediction of preeclampsia: Validation of screening algorithms in a Russian population. Obstetrics and Gynecology. 2017; (8): 74-84. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.8.74-84.
- Tucker K.L., Mort S., Yu L.M., Campbell H., Rivero-Arias O., Wilson H.M. et al.; BUMP Investigators. Effect of self-monitoring of blood pressure on diagnosis of hypertension during higher-risk pregnancy: The BUMP 1 randomized clinical trial. JAMA. 2022; 327(17): 1656-65. https://dx.doi.org/10.1001/jama.2022.4712.
- van den Heuvel J.F.M., Teunis C.J., Franx A., Crombag N.M.T.H., Bekker M.N. Home-based telemonitoring versus hospital admission in high risk pregnancies: a qualitative study on women’s experiences. BMC Pregnancy Childbirth. 2020; 20: 77. https://dx.doi.org/10.1186/s12884-020-2779-4.
- van den Heuvel J.F.M., Lely A.T., Huisman J.J., Trappenburg J.C.A., Franx A., Bekker M.N. SAFE@HOME: Digital health platform facilitating a new care path for women at increased risk of preeclampsia - A case-control study. Pregnancy Hypertens. 2020; 22: 30-6. https://dx.doi.org/10.1016/j.preghy.2020.07.006.
- Collins E., Keedle H., Jackson M., Lequertier B., Schmied V., Boyle J. et al. Telehealth use in maternity care during a pandemic: A lot of bad, some good and possibility. Women Birth. 2024; 37(2): 419-27. https://dx.doi.org/10.1016/j.wombi.2023.12.008.
- Robles Cuevas M.A., López Martínez I., López Domínguez E., Hernández Velázquez Y., Domínguez Isidro S., Flores Frías L.M. et al. Telemonitoring system oriented towards high-risk pregnant women. Healthcare (Basel). 2022; 10(12): 2484. https://dx.doi.org/10.3390/healthcare10122484.
Received 22.08.2024
Accepted 18.11.2024
About the Authors
Tatiana L. Savinova, Vice-Governor, Deputy Chairman, Government of the Orenburg Region for Social Policy – Minister of Health of the Orenburg Region,+7(3532)78-61-38, 78-63-84
Andrey A. Grudkin, Head, Orenburg Clinical Perinatal Center, 460051, Russia, Orenburg, Gagarin Ave., 23, +7(3532)49-91-00, gob41@mail.orb.ru
Irina V. Ermolaeva, Chief Physician, Orenburg Regional Hospital No. 3, 460040, Russia, Orenburg, Gagarin Ave., 19А, +7(903)360-38-02, i-ermolaeva@mail.ru
Tatiana A. Kundik, Head of the Department of Organization of Medical Care for Children and Maternity Services of the Ministry of Health of the Orenburg Region,
Orenburg, Russia, office04@mail.orb.ru
Boris V. Zingerman, Scientific Supervisor, “AyPat” Ltd, 115533, Russia, Moscow, Andropov Ave., 22, +7(499)519-00-78, boriszing@gmail.com,
https://orcid.org/0000-0002-1855-1834
Nadia A. Abu Al Laban, Senior Programmer, “AyPat” Ltd, 115533, Russia, Moscow, Andropov Ave., 22, +7(499)519-00-78, naabulaban@gmail.com
Rostislav A. Borodin, Technical Director, “AyPat” Ltd, 115533, Russia, Moscow, Andropov Ave., 22, +7(499)519-00-78, borodin@medsenger.ru
Irina V. Yakovleva, PhD (Sociology), Associate Professor, School of Public Administration, Lomonosov Moscow State University; Expert, Department of Telemedicine,
V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4,
+7(495)438-25-38, yakovleva@spa.msu.ru, https://orcid.org/0000-0002-1332-6419
Alexey M. Kholin, PhD, Head of the Department of Telemedicine, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,
Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, +7(495)438-25-38, a_kholin@oparina4.ru, https://orcid.org/0000-0002-4068-9805
Marina P. Shuvalova, PhD, Associate Professor, Deputy Director – Head of the Department of Regional Cooperation and Integration, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, +7(495)438-25-38, m_shuvalova@oparina4.ru, https://orcid.org/0000-0002-6361-9383
Gennady T. Sukhikh, Academician of the RAS, Dr. Med. Sci., Professor, Director, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, g_sukhikh@oparina4.ru, https://orcid.org/0000-0002-7712-1260
Corresponding author: Alexey M. Kholin, a_kholin@oparina4.ru