Pregnancy after in vitro fertilization: obstetric and perinatal risks
Igitova M.B., Kazanina A.B., Cherkasova T.M., Yavorskaya S.D., Dmitrienko K.V., Dolgova N.S.
Relevance: The incidence of infertile marriages in Russia is steadily increasing, as is the rate of pregnancies after assisted reproductive technologies (ART). However, obstetric and perinatal outcomes of patients undergoing ART have not been fully studied.
Objective: To evaluate the incidence and structure of obstetric and perinatal complications in pregnant women following in vitro fertilization (IVF).
Materials and methods: Obstetric and perinatal outcomes were retrospectively analyzed in 96 patients with singleton pregnancies resulting from IVF (study group) and in 96 patients with spontaneous pregnancy (control group), who were matched by age, parity, and other characteristics.
Results: The incidence of major pregnancy complications in the control group was not significantly different from that in the study group. However, the study group had a significantly higher incidence of anemia (54/96 (56.3%) vs. 24/96 (25.0%); p<0.001) and gestational diabetes mellitus (26/96 (27.1%) vs. 11/96 (11.5%); p=0.01), as well as uteroplacental blood flow abnormalities in the third trimester of pregnancy and before delivery (40/96 (41.7%) vs. 25/96 (26.0%); p=0.03). The majority of patients in the study group underwent cesarean section (71/96 (74.0%) vs. 25/96 (26.0%), respectively; p<0.001). In study group planned surgeries were more common than emergency surgeries (60/71 (84.5%) vs. 9/25 (36.0%), respectively; p<0.001). Opposite dynamics were observed in the control group. Newborns from mothers in the study group were eight times more likely to have septal heart defects (15/96 (15.6%) versus 2/96 (2.1%); p>0.05) and were six times more likely to have transient hypoglycemia (19/96 (19.8%) vs. 3/96 (3.1%); p>0.05). They were also 2 times more likely to require a second stage of nursing (7/96 (7.3%) vs. 3/96 (3.1%); p>0.05).
Conclusion: The identified features of the course of pregnancy and the condition of newborns in patients who became pregnant as a result of IVF indicate that pregnancy in this group of patients should be managed by highly qualified obstetrician-gynecologists. When planning childbirth, it is necessary to assess the risks and choose the optimal method of delivery and a maternity facility where there is a possibility of early neonatal diagnosis of congenital malformations and provision of prolonged postnatal care to newborns.
Authors' contributions: Igitova M.B. – conception and design of the study, editing of the manuscript; Kazanina A.B. – material collection and processing, statistical analysis; Cherkasova T.M. – material collection and processing; Yavorskaya S.D., Dmitrienko K.V. – drafting of the manuscript, literature review; Dolgova N.S. - drafting of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Altay State Medical University.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Igitova M.B., Kazanina A.B., Cherkasova T.M., Yavorskaya S.D., Dmitrienko K.V.,
Dolgova N.S. Pregnancy after in vitro fertilization: obstetric and perinatal risks.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (7): 58-64 (in Russian)
https://dx.doi.org/10.18565/aig.2024.94
Keywords
According to current statistics, the prevalence of infertility in marriages in the Russian Federation is up to 20% [1]. In Altai Krai, the prevalence is 15% and 19.3% in urban and rural populations, respectively [2]. Moreover, its prevalence is steadily increasing [1, 3]. Assisted reproductive technologies (ART) have become a popular method of treating infertility in the 21st century [1, 3]. This is evidenced by the annual increase in the number of reproductive centers and ART protocols [4]. However, despite more than 40 years of history in medical practice, ART still raises concerns regarding the risks to both the mother and fetus, which remain topics of scientific research and debate.
Some researchers believe that obstetric and perinatal risks depend primarily on the age and initial physical health of expectant parents [5]. On the other hand, other experts claim that pregnancy after ART is an independent risk factor for adverse maternal and perinatal outcomes [5, 6]. We conducted our study because of conflicting data on obstetric and perinatal complications, and neonatal risks in pregnant women following different ART techniques.
This study aimed to evaluate the incidence and structure of obstetric and perinatal complications in pregnant women of the Altai Krai, whose pregnancies resulted from in vitro fertilization (IVF).
Materials and methods
A retrospective analysis of the course of pregnancy and childbirth was initially performed in 127 patients whose pregnancies resulted from ART from 2020 to 2022. In 115/127 (90.6) pregnancies occurred after the standard IVF procedure, in 9/127 (7.1%) after cryopreserved transfer, and in 3/127 (2.4%) after intracytoplasmic sperm injection (ICSI). Pregnancy with one fetus occurred in 96/127 (75.6%) patients, and multiple pregnancies (twins) occurred in 31/127 (24.4%) patients. Considering that the most common ART method in Altai Krai is IVF, in the second stage, a retrospective comparative analysis of the course of pregnancy, childbirth, and perinatal outcomes was performed in 96 patients with a singleton pregnancy resulting from IVF (study group) and 96 patients with a spontaneous singleton pregnancy (control group).
This study was conducted at the Altai Center for Maternal and Child Health (Barnaul), which is the clinical affiliation of the Department of Obstetrics and Gynecology, Altay State Medical University (Chief Physician – Smirnov K.V., PhD).
Inclusion criteria were singleton pregnancy resulting from IVF and informed consent from patients for the use and publication of their personal data.
The exclusion criteria were multiple pregnancies, pregnancy after ICSI or cryopreserved transfer.
During the study, an analysis was carried out on the data presented in the main medical documentation (delivery notes and developmental histories of newborns and individual records of pregnant and postpartum women), including an assessment of the full set of general clinical data and the results of laboratory and functional research methods carried out in accordance with current regulatory documents [7].
Statistical analysis
Statistical analysis was performed using Statistica 11.0 and Microsoft Excel 2010. The distribution of continuous variables was tested for normality using the Shapiro–Wilk test. Continuous variables are presented as median (Me) with interquartile range (Q1; Q3); frequencies and percentages were reported for categorical variables. The Mann–Whitney U test was used to compare continuous variables between the groups. The Pearson's χ2 test was used to compare categorical variables. Yates' correction was used when the expected frequencies were >5 or Fisher's two-tailed exact test (when expected frequencies were ≤5). The critical level of statistical significance for the differences (p) was defined as p<0.05 [8].
The study was reviewed and approved by the Research Ethics Committee of Altay State Medical University.
Results and discussion
Pregnant and postpartum women in the study groups were comparable in terms of age, parity, and other matching characteristics (Table 1). The median age was 34 years in the study group [(Q1; Q3)=(32; 36)] and 33 years in the control group [(Q1; Q3)=(31; 33)] (p=0.221). Most patients in the study group, 71/96 (74.0%), had secondary infertility. Peritoneal factor was the main cause of infertility and the need for ART. The median duration of infertility was four years [(Q1; Q3)=(2; 6)].
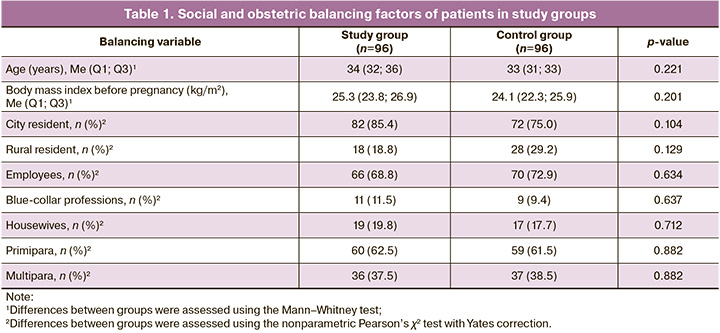
The frequency and structure of somatic pathology in patients of the study groups did not differ significantly, including chronic arterial hypertension (11/96 (11.5%) and 6/96 (6.3%); p=0.310), chronic diseases of the urinary system (16/96 (16.7%) and 14/96 (14.6%); p=0.099), varicose veins of the lower extremities (17/96 (17.7%) and 9/96 (9.4%); p=0.140), pathology of the thyroid gland, and subclinical hypothyroidism (20/96 (20.8%) and 10/96 (10.4%); p=0.074). It is believed that the presence of an increased body mass index in patients undergoing ART protocols not only reduces their effectiveness but also increases the risk of developing hypertension during pregnancy compared with patients with spontaneous pregnancy [3, 9]. The number of patients who were obese before pregnancy was almost identical between the study groups (16/96 (16.7%) and 15/96 (15.6%); p=1.000).
However, there are conflicting data in the scientific literature regarding the incidence of obstetric complications in pregnant women after ART. Lang M. et al. (2023) reported a 2-fold increase in the incidence of gestational hypertension and pre-eclampsia in pregnant women after ART compared to pregnant women with spontaneous pregnancy [10]. Wei D. et al. (2019) found an increased risk of gestational complications associated with arterial hypertension only after the use of cryopreserved transfer [6]. A study conducted by researchers from Turkey (2021), which included an analysis of the course of pregnancy in 10,929 patients, showed that the frequency of cholestasis during pregnancy in pregnant women after IVF was several times higher than that in the group of patients with spontaneous pregnancy [11]. Several authors have reported a higher incidence of preterm delivery and low birth weight in patients after ART [12].
We found no significant differences between the study groups in the incidence of arterial hypertension (6/96 (6.3%) and 7/96 (7.3%); p=1.000) and preeclampsia (late, moderate) (3/96 (3.1%) and 5/96 (5.2%); p>0.05), in terms of the incidence of pregnancy complications, such as isthmic cervical insufficiency requiring cerclage (12/96 (12.5%) and 7/96 (7.3%); p=0.334) and preterm delivery (8/96 (8.3%) and 7/96 (7.3%); p=1.000). According to Cavoretto P. et al. (2018), the risk of preterm birth is twice as high in patients who become pregnant after ART as in women who become pregnant spontaneously, including up to 34 weeks [13, 14]. At the same time, in our study, pregnant women after IVF (study group) had two times more gestational complications, such as anemia (54/96 (56.3%) vs. 24/96 (25.0%); p<0.001) and gestational diabetes mellitus (26/96 (27.1%) vs. 11/96 (11.5%); p=0.011).
The use of ART is considered an independent factor in the development of placental abnormalities and dysfunction [15]. As early as 2006, Romundstad L.B. reported a threefold increased risk of placenta accreta in patients whose pregnancy occurred as a result of ART [16], which was later confirmed by other researchers [17, 18]. Johnson K.M. et al (2020) reported that in patients using ART, ischemic disease of the placenta occurs 4 times more often in preterm and 1.7 times more often in term pregnancies [19]. The same data were obtained when the oocyte donation protocols were used [20].
In the present study, there were no cases of abnormal placentation in the group of pregnant women after IVF, but markers of placental dysfunction, such as uteroplacental blood flow disturbance according to Doppler measurements at the end of the third trimester and before delivery, were recorded 1.6 times more frequently than in the control group (40/96 (41.7%) and 25/96 (26.0%), respectively; p=0.033).
Pregnancy resulting from ART is not an indication for cesarean delivery. Previous studies have shown that the relative risk of cesarean delivery in primiparas over 35 years of age with a singleton pregnancy is 1.44–2.27 [5]. However, the cesarean section rate in pregnant women receiving infertility treatment with ART is quite high worldwide [21], which was also the case in our study. The high rate of cesarean sections in patients after IVF is due to the sum of the relative indications. Cesarean section is usually performed routinely (84.5%) in the interest of the fetus because of increased fear of adverse outcomes by both pregnant women and medical staff. Patients in the study group underwent cesarean delivery 2.8 times more often than those in the control group (71/96 (74.0%) and 25/96 (26.0%), respectively; p<0.001). In the group of patients who underwent operative delivery, planned operations predominated in the study group (60/71 (84.5%) and 9/25 (36.0%), respectively; p<0.001), whereas emergency operations were more frequent in the control group (11/71 (15.5%) and 16/25 (64.0%), respectively; p<0.001). The most common indication for emergency cesarean delivery in both groups was intrapartum fetal distress.
According to global statistics, perinatal outcomes in newborns of mothers whose pregnancies resulted from ART have a higher incidence of complications than those in the general population. For example, in an analysis of 425,732 singleton pregnancies, of which 10,235 were the result of ART, antenatal fetal death and stillbirth were significantly more common in women receiving ART [22, 23], as was the incidence of neonatal asphyxia and perinatal mortality [24, 25]. Ombelet W. et al. found a greater frequency of low birth weight for gestational age in women after ART [26], which indirectly indicates the presence of placental dysfunction during pregnancy.
In the present study, despite the higher incidence of placental dysfunction, anemia, and gestational diabetes mellitus in pregnant women after ART, the incidence of low-birth-weight newborns or, conversely, large fetuses in the study groups did not differ significantly and corresponded to the general population data. However, septal heart defects in newborns from mothers in the study group were detected eight times more often than in the control group (Table 2). Our results are consistent with those of the studies by Parizot E. et al. (2019) [27] and other researchers [28], who showed that during pregnancy achieved with the help of ART, the incidence of congenital malformations of the fetus, including heart defects, is higher than that in the general population of pregnant and postpartum women. According to Sung et al. (2021), women with a history of repeated implantation failure should be considered a high-risk group for congenital malformations in the fetus [29].
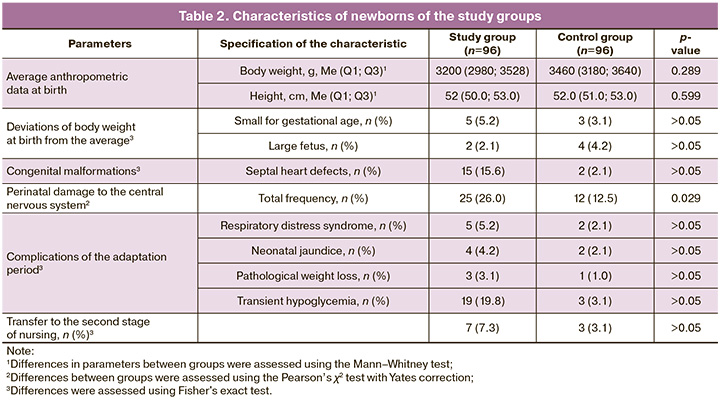
Perinatal central nervous system damage was observed 2 times more frequently in neonates born to mothers in the study group than in neonates born to mothers in the control group. In addition, perinatal central nervous system damage was classified as severe (p>0.05) in 3/96 (3.1%) infants born vaginally to mothers in the study group. In addition, despite the absence of significant differences in the frequency of most pathological conditions during the neonatal adaptation period, transient hypoglycemia was recorded six times more frequently in neonates of mothers in the study group than in those of the control group, which is directly proportional to the frequency of gestational diabetes in pregnant women after IVF.
Due to various complications of the adaptation period, newborns from mothers in the study group were transferred to the second stage of nursing twice as often as newborns from mothers in the control group.
Conclusion
The study results revealed that patients with singleton pregnancies resulting from IVF are at an increased risk of developing anemia, gestational diabetes mellitus, and placental dysfunction. This dysfunction is characterized by disturbances in uteroplacental blood flow, as indicated by Doppler measurements throughout gestation and before delivery. Additionally, newborns of these patients are susceptible to septal heart defects and transient hypoglycemia. These findings suggest the importance of close clinical observation by a highly skilled obstetrician-gynecologist for pregnant women after ART (IVF), who should collaborate with specialists from various fields, such as therapists, endocrinologists, and hematologists. Furthermore, delivery should be planned at a tertiary care center, as this allows for a targeted and comprehensive approach to address delivery methods, early detection of congenital malformations that may have been missed during pregnancy, and the provision of advanced neonatal care in the postnatal period.
References
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Женское бесплодие. 2021. 81с. [Ministry of Health of the Russian Federation. Clinical guidelines. Female infertility. 2021. 81p.(in Russian)].
- Гурьева В.А. Распространенность и причины женского бесплодия в сельской и городской местности. В кн.: Академическая наука - проблемы и достижения. Материалы III международной научно-практической конференции. Том 1. 2014: 38. [Gur’eva V.A. Prevalence and causes of female infertility in rural and urban areas. In: Academic science - problems and achievements. Materials of the III International scientific and practical conference. Vol. 1. 2014: 38. (in Russian)].
- Жук Т.В., Яворская С.Д., Востриков В.В. Предикторы неудач программы ЭКО у пациенток с бесплодием и профицитом массы тела. Бюллетень медицинской науки. 2017; 3(7): 58-9. [Zhuk T.V., Yavorskaya S.D., Vostrikov V.V. IVF program failure predictors in patients with infertility and underweight. Bulletin of Medical Science. 2017; 3(7): 58-9.(in Russian)].
- Фазлыева Э.А., Галиева Г.А., Измайлова Р.А. Анализ рынка вспомогательных репродуктивных технологий в Российской Федерации и Республике Башкортостан. Менеджер здравоохранения. 2022; 3: 10-6. [Fazlyeva E.A., Galieva G.A., Izmailova R.A. Market analysis of assisted reproductive technologies in the Russian Federation and in the Republic of Bashkortostan. Manager Zdravoohranenia. 2022; (3): 10-6. (in Russian)]. https://dx.doi.org/10.21045/1811-0185-2022-3-10-16.
- Яковлева О.В., Глухова Т.Н., Рогожина И.Е. Основные принципы ведения беременности после вспомогательных репродуктивных технологий. Медицинский вестник Северного Кавказа. 2020; 15(1): 140-5. [Yakovleva O.V., Glukhova T.N., Rogozhina I.E. Basic principles for the management of pregnancy after assisted reproductive technologies. Medical News of North Caucasus. 2020; 15(1): 140-5. (in Russian)]. https://dx.doi.org/10.14300/mnnc.2020.15035.
- Wei D., Liu J.Y., Sun Y., Shi Y., Zhang B., Liu J.Q. et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019; 393(10178): 1310-8. https://dx.doi.org/10.1016/S0140-6736(18)32843-5.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Нормальная беременность. 2023. [Ministry of Health of the Russian Federation. Clinical guidelines. Normal pregnancy. 2023.(in Russian)].
- Медик В.А., Толмачев М.С. Математическая статистика в медицине. 2-е изд. Том 1. М.: Издательство Юрайт; 2024. 472с. [Medik V.A., Tolmachev M.S. Mathematical statistics in medicine. 2nd ed. Vol. 1. Moscow: Yurait Publishing House; 2024. 472p. (in Russian)].
- American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice; Committee on Genetics; U.S. Food and Drug Administration. Committee Opinion No 671: perinatal risks associated with assisted reproductive technology. Obstet. Gynecol. 2016; 128(3): e61-e68. https://dx.doi.org/10.1097/AOG.0000000000001643.
- Lang M., Zhou M., Lei R., Li W. Comparison of pregnancy outcomes between IVF-ET pregnancies and spontaneous pregnancies in women of advanced maternal age. J. Matern. Fetal Neonatal Med. 2023. 36(1): 2183761. https://dx.doi.org/10.1080/14767058.2023.2183761.
- Alemdaroğlu S., Yılmaz Baran Ş., Durdağ G.D., Yuksel Şimşek S., Yetkinel S., Alkaş Yağınç D. et al. Intrahepatic cholestasis of pregnancy: are in vitro fertilization pregnancies at risk? J. Matern. Fetal Neonatal Med. 2021; 34(15): 2548-53. https://dx.doi.org/10.1080/14767058.2020.1765331.
- Ageheim M., Skalkidou A., Bergman E., Iliadis S., Lampa E., Lindström L.et al. Fetal growth after fresh and frozen embryo transfer and natural conception: a population-based register study. BJOG. 2024; 131(9): 1229-37.https://dx.doi.org/10.1111/1471-0528.17786.
- Cavoretto P., Candiani M., Giorgione V., Inversetti A., Abu-Saba M.M.,Tiberio F. et al. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: meta-analysis of cohort studies. Ultrasound Obstet. Gynecol. 2018; 51(1): 43-53. https://dx.doi.org/10.1002/uog.18930.
- Cavoretto P.I., Giorgione V., Sotiriadis A., Viganò P., Papaleo E., Galdini A. et al. IVF/ICSI treatment and the risk of iatrogenic preterm birth in singleton pregnancies: systematic review and meta-analysis of cohort studies. J. Matern. Fetal Neonatal Med. 2022; 35(10): 1987-96. https://dx.doi.org/10.1080/14767058.2020.1771690.
- Vermey B.G., Buchanan A., Chambers G.M., Kolibianakis E.M., Bosdou J., Chapman M.G. et al. Are singleton pregnancies after assisted reproduction technology (ART) associated with a higher risk of placental anomalies compared with non-ART singleton pregnancies? A systematic review and meta-analysis. BJOG. 2019; 126(2): 209-18. https://dx.doi.org/10.1111/1471-0528.15227.
- Romundstad L.B., Romundstad P.R., Sunde A., von Düring V., Skjaerven R., Vatten L.J. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum. Reprod. 2006; 21(9): 2353-8. https://dx.doi.org/10.1093/humrep/del153.
- Heshmatnia F., Jafari M., Bozorgian L., Yadollahi P., Khalajinia Z., Azizi M. Is there a relationship between assisted reproductive technology and maternal outcomes? A systematic review of cohort studies. Int. J. Reprod. Biomed. 2023; 21(11): 861-80. https://dx.doi.org/10.18502/ijrm.v21i11.14651.
- Liu C.N., Yu F.B., Xu Y.Z., Li J.S., Guan Z.H., Sun M.N. et al. Prevalence and risk factors of severe postpartum hemorrhage: a retrospective cohort study. BMC Pregnancy Childbirth. 2021; 21(1): 332. https://dx.doi.org/10.1186/s12884-021-03818-1.
- Johnson K.M., Hacker M.R., Thornton K., Young B.C., Modest A.M. Association between in vitro fertilization and ischemic placental disease by gestational age. Fertil. Steril. 2020; 114(3): 579-86. https://dx.doi.org/10.1016/j.fertnstert.2020.04.029.
- Modest A.M., Johnson K.M., Karumanchi S.A., Resetkova N., Young B.C., Fox M.P. et al. Risk of ischemic placental disease is increased following in vitro fertilization with oocyte donation: a retrospective cohort study. J. Assist. Reprod. Genet. 2019; 36(9): 1917-26. https://dx.doi.org/10.1007/s10815-019-01545-3.
- Richmond E., Ray J.G., Pudwell J., Djerboua M., Gaudet L., Walker M. et al. Caesarean birth in women with infertility: population-based cohort study. BJOG. 2022; 129(6): 908-16. https://dx.doi.org/10.1111/1471-0528.17019.
- Bay B., Boie S., Kesmodel U.S. Risk of stillbirth in low-risk singleton term pregnancies following fertility treatment: a national cohort study. BJOG. 2019; 126(2): 253-60. https://dx.doi.org/10.1111/1471-0528.15509.
- Sarmon K.G., Eliasen T., Knudsen U.B., Bay B. Assisted reproductive technologies and the risk of stillbirth in singleton pregnancies: a systematic review and meta-analysis. Fertil. Steril. 2021; 116(3): 784-92. https://dx.doi.org/10.1016/j.fertnstert.2021.04.007.
- Chughtai A.A., Wang A.Y., Hilder L., Li Z., Lui K., Farquhar C. et al. Gestational age-specific perinatal mortality rates for assisted reproductive technology (ART) and other births. Hum. Reprod. 2018; 33(2): 320-7. https://dx.doi.org/10.1093/humrep/dex340.
- Sabban H., Zakhari A., Patenaude V., Tulandi T., Abenhaim H.A. Obstetrical and perinatal morbidity and mortality among in-vitro fertilization pregnancies: a population-based study. Arch. Gynecol. Obstet. 2017; 296(1): 107-13. https://dx.doi.org/10.1007/s00404-017-4379-8.
- Ombelet W., Van Blerkom J. , Bruckers L., Dhont N., Nargund G., Campo R. Promising perinatal outcome after using a simplified low-cost IVF culture system specifically designed for resource-poor countries. J. Clin. Med. 2023; 12(6): 2264. https://dx.doi.org/10.3390/jcm12062264.
- Parizot E., Dard R., Janel N., Vialard F. Down syndrome and infertility: what support should we provide? J. Assist. Reprod. Genet. 2019; 36(6): 1063-7. https://dx.doi.org/10.1007/s10815-019-01457-2.
- Wen S.W., Miao Q., Taljaard M., Lougheed J., Gaudet L., Davies M. et al. Associations of assisted reproductive technology and twin pregnancy with risk of congenital heart defects. JAMA Pediatr. 2020; 174(5): 446-54.https://dx.doi.org/10.1001/jamapediatrics.2019.6096.
- Sung N., Khan S.A., Yiu M.E., Jubiz G., Salazar M.D., Skariah A. et al. Reproductive outcomes of women with recurrent pregnancy losses and repeated implantation failures are significantly improved with immunomodulatory treatment. J. Reprod. Immunol. 2021; 148: 103369. https://dx.doi.org/10.1016/j.jri.2021.103369.
Received 18.04.2024
Accepted 25.06.2024
About the Authors
Marina B. Igitova, Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology, Altay State Medical University, Ministry of Health of the Russian Federation,656038, Russia, Barnaul, Lenin Ave., 40, +7(923)718-60-14, Igitova-2011@mail.ru, https://orcid.org/0000-0003-1267-4179
Anastasia B. Kazanina, Teaching Assistant at the Department of Neonatology and Pediatric Anesthesiology, Altay State Medical University, Ministry of Health of the
Russian Federation, 656038, Russia, Barnaul, Lenin Ave., 40, asia_kor@mail.ru, https://orcid.org/0009-0006-2320-4964
Tatiana M. Cherkasova, PhD, Associate Professor at the Department of Neonatology and Pediatric Anesthesiology, Altay State Medical University, Ministry of Health of
the Russian Federation, 656038, Russia, Barnaul, Lenin Ave., 40, tanechka.cherkasova.2013@mail.ru, https://orcid.org/0000-0001-6841-7134
Svetlana D. Yavorskaya, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology, Altay State Medical University, Ministry of Health of the
Russian Federation, 656038, Russia, Barnaul, Lenin Ave., 40, L2001@bk.ru, https://orcid.org/0000-0001-6362-5700
Ksenia V. Dmitrienko, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Altay State Medical University, Ministry of Health of the
Russian Federation, 656038, Russia, Barnaul, Lenin Ave., 40, tishovakseni@mail.ru, https://orcid.org/0000-0003-0886-4471
Nadezhda S. Dolgova, PhD, Teaching Assistant at the Department of Obstetrics and Gynecology, Altay State Medical University, Ministry of Health of the Russian Federation, 656038, Russia, Barnaul, Lenin Ave., 40, dolgovans@yandex.ru, https://orcid.org/0000-0002-3646-6596
Corresponding author: Ksenia V. Dmitrienko, tishkovakseni@mail.ru