Врожденные пороки развития половых органов, возникающие вследствие нарушений эмбрионального развития мюллеровых протоков, наблюдаются в общей популяции женщин с частотой от 4 до 7% [1]. Клинические проявления врожденных аномалий могут быть весьма разнообразными — от полного отсутствия какой-либо симптоматики до серьезных нарушений в функционировании органов репродуктивной системы. Отклонения в анатомическом строении половых органов могут приводить к различным осложнениям в акушерской практике. Известно, что перевязка маточных и яичниковых артерий в сочетании с наложением гемостатических компрессионных швов широко применяется при лечении гипотонических маточных кровотечений. Использование указанных методик в большинстве случаев не приводит к негативным последствиям ввиду наличия обширных коллатералей, обеспечивающих восстановление кровоснабжения матки [2]. В нашем сообщении приводится клинический случай некроза правого рога аномально сформированной матки после изолированной перевязки правой маточной артерии.
Клиническое наблюдение
Пациентка К., 33 лет, поступила в учреждение здравоохранения «Гродненский областной клинический перинатальный центр» 26.04.2018 с доношенной беременностью для планового родоразрешения. У пациентки имелась врожденная аномалия развития мочеполовой системы: удвоение матки и агенезия правой почки. Настоящая беременность четвертая: первая и вторая беременности закончились самопроизвольными выкидышами в 2013 и 2014 гг., третья — прервана в малом сроке. Диагноз аномалии половых органов у данной пациентки был установлен после прерывания первой беременности в 2013 г. при ультразвуковом исследовании. Со слов пациентки, все беременности развивались в правой матке. Каких-либо дополнительных методов диагностики для уточнения состояния органов мочеполовой системы не проводилось. Настоящая беременность не была запланирована, предгравидарная подготовка не осуществлялась. Беременность протекала без осложнений.
27.04.2018 произошел преждевременный разрыв плодных оболочек. В связи с неготовностью родовых путей к родам, отсутствием родовой деятельности, а также с учетом врожденной аномалии развития внутренних половых органов и отягощенного акушерского анамнеза, пациентка была родоразрешена путем операции кесарева сечения. 27.04.2018 в 01.45 был извлечен плод женского пола массой 2850 г, длиной 50 см, с оценкой по шкале Апгар 8/9 баллов. Во время оперативного вмешательства установлено, что беременность развивалась в правом роге матки, левая матка была слегка увеличена в размерах; придатки с обеих сторон не изменены. Оба маточных рога соединялись между собой в области нижнего сегмента тонкой соединительнотканной перегородкой, сообщения между полостями не установлено. Ввиду гипотонического состояния правого рога матки и в связи с наличием гематомы между листками широкой связки выполнена перевязка восходящей ветви маточной артерии на протяжении без выделения ее из окружающих тканей на фоне внутривенного введения утеротоников. Проведенные мероприятия дали положительный эффект (рис. 1). Операция закончена типично. Общая кровопотеря составила 650 мл.

В послеоперационном периоде пациентка предъявляла жалобы на постоянный субфебрилитет (37,2— 37,4°С), незначительные боли в области послеоперационной раны. Несмотря на проводимую антибактериальную терапию (цефотаксим, метронидазол, с х суток — меропенем), сохранялась субфебрильная температура, имели место лохии с неприятным запахом. При ультразвуковом исследовании, выполненном многократно, отмечалось отсутствие инволюции правого рога матки, в полости матки постепенно увеличивалось количество гиперэхогенного содержимого, а с 19-х суток послеродового периода создавалось впечатление о «разволокнении» миометрия при отсутствии четкой границы между ним и полостью матки (рис. 2). При инструментальном обследовании полости матки получен весьма скудный соскоб. При лабораторном обследовании обращали на себя внимание анемия (гемоглобин 70—78 г/л), сдвиг лейкоцитарной формулы влево, постепенное прогрессивное увеличение содержания тромбоцитов (до 820-896х 109/л); при этом уровни С-реактивного белка и прокальцитонина находились в пределах нормы.

Учитывая отсутствие эффекта от проводимой терапии, на 26-е сутки послеродового периода выполнена диагностическая гистероскопия. Под внутривенным наркозом после фиксации шейки матки слева от нее на стенке влагалища удалось обнаружить гипопла- зированный вход в левый маточный рог, который первоначально и был осмотрен — визуализированы обычный бледно-розовый эндометрий и свободное устье левой маточной трубы. Затем через нормально сформированную шейку гистероскоп был введен в правый рог матки, где обнаружены многочисленные фибринозные наложения, формирующие широкие лентовидные спайки, препятствующие осмотру. После разрушения рыхлых сращений была визуализирована слизистая оболочка желто-серого цвета с мелкими пузырьками газа на стенках, устье правой маточной трубы было облитерировано. Выполнено выскабливание стенок полости правой матки. Гистологический ответ: бесструктурные некротические массы, гнойно-гранулезная ткань.
После гистероскопии была продолжена консервативная терапия линезолидом и метронидазолом, что, впрочем, не дало эффекта: сохранялся субфебрилитет при отсутствии болевого синдрома, ультразвуковая картина не претерпела существенных изменений, лабораторные показатели не имели тенденции к положительной динамике. В данной связи на 33-и сутки послеродового периода выполнена релапаротомия. Установлено, что правый рог матки темно-коричневого цвета, дряблой консистенции, к нему припаяны петли тонкой кишки и сальник, маточная труба резко отечна, яичник представлен образованием 5х6 см с гнойным содержимым внутри. Левый маточный рог и придатки не изменены. Учитывая интраоперационную картину, выполнена гистерэктомия с правыми придатками и левой маточной трубой, дренирование брюшной полости.
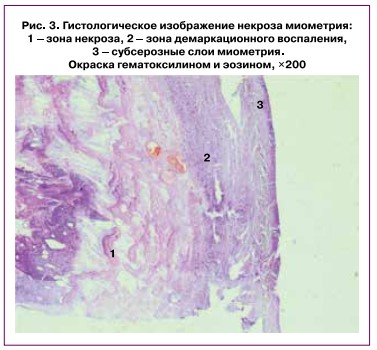
Гистологическое исследование: интрамуральные участки миометрия в состоянии асептического некроза с очаговыми кальцификатами; в субсерозных участках миометрия — демаркационное продуктивное воспаление (рис. 3); сосуды миометрия кавернозно расширены и тромбированы; ткань правого яичника в состоянии гнойного расплавления.
Послеоперационный период протекал без особенностей на фоне антибактериальной терапии линезо- лидом и колистатом. Пациентка выписана из стационара на 42-е сутки послеродового периода в удовлетворительном состоянии.
Обсуждение
Некроз матки является редким осложнением, развивающимся вследствие эмболизации маточных артерий [3, 4], деваскуляризации матки с наложением компрессионных швов [5, 6], инфекции [7]. Факторами, способствующими некрозу при эмболизации маточных сосудов, являются размер эмбо- лизирующих частиц, техника эмболизации (селективная, неселективная) [3], характер существующих анастомозов [4]. В случае наложения гемостатических компрессионных швов ишемия, возникающая после их применения, нивелируется благодаря инволюции послеродовой матки и наличию адекватно функционирующих сосудистых анастомозов [2]. Поэтому строение сосудистого русла имеет очень важный практический аспект. Посвященные изучению данного вопроса исследования свидетельствуют о чрезвычайном разнообразии вариантов отхождения маточных артерий [8]. В основном они берут начало из переднего ствола внутренней подвздошной артерии, однако могут происходить из запирательной, внутренней половой, пупочной, пузырной, наружной подвздошной артерии. Описаны наблюдения полного отсутствия маточных артерий; основным источником кровоснабжения в данном случае являются увеличенные в диаметре яичниковые артерии. Следует отметить, что все указанные варианты описаны при анатомически нормально развитой матке. Исследований, посвященных изучению сосудистого русла при аномалиях развития матки, в доступной литературе мы не обнаружили.
Клинические проявления некроза матки могут быть различными в зависимости от степени возникающей ишемии. При полной деваскуляризации наблюдаются высокая температура, диффузная абдоминальная боль, диарея, зловонные лохии, что не вызывает затруднений в постановке диагноза [9]. При частичной же деваскуляризации клиническая картина весьма стертая, схожая по проявлениям с вялотекущим эндометритом. В данной ситуации весомую роль играют результаты дополнительных методов диагностики. При ультразвуковом исследовании следует обращать внимание на неоднородное изображение миометрия, наличие «неидентифицируемого эндометрия» и гиперэхогенного содержимого в полости матки [5]. Компьютерная томография позволяет выявить наличие пузырьков газа в структуре миометрия [9], а допплерометрия и магнитно-резонансная томография с контрастированием — аваскуляриза- цию миометрия [5]. Незнание врачами клинической картины некроза матки является причиной запоздалой диагностики. Клинический случай, практически идентичный с представленным нами, описан в работе E.J. Treloar et al. [5]. Диагноз некроза матки был установлен спустя 2 месяца (!) после родов у пациентки после кесарева сечения, в ходе которого использовался гемостатический шов по B-Lynch. Постоянные кровянистые выделения, незначительные боли и вздутие живота заставили авторов предполагать новообразование матки, выполнять неоднократные выскабливания стенок полости матки и настойчиво продолжать антибактериальную терапию. Лишь использование инструментальных методов диагностики позволило заподозрить некроз матки и выполнить в последующем гистерэктомию.
Поздней манифестацией некроза матки может быть появление на коже передней брюшной стенки свища, сообщающегося с полостью матки [6] — в описываемом авторами наблюдении массивное послеродовое кровотечение было купировано путем лигирования сосудистых пучков и применения шва по B-Lynch. Следует учитывать, что дополнительными факторами, усугубляющими ишемию при использовании указанных методик, могут быть как дефицит объема циркулирующей крови и коагулопатия, всегда имеющие место при массивных акушерских кровотечениях, так и быстрота выполнения мероприятий по достижению хирургического гемостаза [10].
Приведенное наблюдение наводит на следующие размышления. Во-первых, помимо порока развития матки, имело место и аномальное формирование сосудистого русла в ней. Правая маточная артерия, видимо, оказалась единственным источником кровоснабжения правого рога матки, правая же яичниковая артерия могла быть несостоятельной либо вообще отсутствовать по причине агенезии почки, что, вероятно, способствовало гнойному расплавлению правого яичника. Лигирование восходящего отрезка маточной артерии в данных условиях привело к некрозу миометрия даже при отсутствии дефицита объема циркулирующей крови. Именно аномальное развитие сосудистого русла матки явилось основным предрасполагающим фактором некроза в описываемой ситуации.
Во-вторых, течение асептического некроза было вялым, маскировалось массивнейшей антибактериальной терапией, что позволило предотвратить вторичную бактериальную инфекцию. Данная клиническая ситуация, по сути, поставила в тупик акушеров-гинекологов, использовавших все возможные способы лечения предполагаемого послеродового эндомиометрита (иных альтернатив не было!) и не получивших абсолютно никакого положительного результата. В этой связи следует признать, что именно неосведомленность врачей о возможности некроза матки и незнание вариантов его клинических проявлений послужили причиной ошибочной тактики — длительного наблюдения за пациенткой даже при неэффективности проводимой консервативной терапии. Ретроспективный анализ также позволяет сделать вывод и о том, что целесообразна была более активная тактика в отношении данной пациентки — выполнение релапаротомии или диагностической лапароскопии для уточнения диагноза. Наконец, необходимо было более активное использование дополнительных методов исследования, в частности, допплерометрических методик, магнитно-резонансной томографии [11], которые, вероятно, позволили бы выявить гипо- либо аваскуляризацию правого рога матки по сравнению с левым. Кроме того, видимо, есть смысл использовать указанные дополнительные методы исследования у всех пациенток с аномалиями развития половых органов не только при беременности, но и на этапе предгравидарной подготовки, учитывая разнообразие клинических вариантов пороков развития матки [11, 12].
Заключение
В соответствии с классификацией врожденных аномалий развития половых органов ESHRE/ ESGE [1], представленное клиническое наблюдение можно охарактеризовать как U3 C3 V0 — полное удвоение тела матки с односторонней гипоплазией шейки матки. Лигирование восходящей ветви правой маточной артерии явилось причиной ишемии и последующего некроза правого рога матки. Правая маточная артерия являлась безальтернативным источником кровоснабжения маточного рога. Диагностика некроза матки возможна при сопоставлении клинической картины с данными дополнительных методов исследования, при которых следует обращать внимание на отсутствие нормальной архитектоники матки и аваскуляризацию миометрия. При подозрении на некроз матки следует выполнять диагностическую лапароскопию или лапаротомию для своевременной диагностики этого осложнения.