Anthropometric predictors of cephalopelvic disproportion
Tysyachnyi O.V., Babich D.A., Baev O.R.
Background: The discrepancy between the sizes of the maternal pelvis and fetus is associated with high operative delivery rates, as well as obstetric and neonatal morbidity and mortality. The use of classical pelvimetry to predict cephalopelvic disproportion is currently considered insufficient. Evidence suggests that in the formation of a clinically narrow pelvis, the ratio of the head circumference to the maternal height plays a major role rather than the body weight of the fetus. Therefore, studying the anthropometric data of both the mother and fetus during full-term pregnancies in Russia is essential for identifying the risk groups for clinically narrow pelvises.
Objective: To investigate the prognostic significance of anthropometric data of women and fetuses at full term concerning the risk of a clinically narrow pelvis.
Materials and methods: This retrospective cohort study analyzed 12,034 delivery case records, which were divided into two groups. The study group (n=183) comprised women who underwent cesarean delivery due to a narrow pelvis, while the control group (n=915) included women who underwent vaginal delivery.
Results: The highest frequency of a clinically narrow pelvis and operative abdominal delivery was observed with a head circumference >342.15 mm and fetal body weight >3670 g. The median ratio of fetal head circumference measured by ultrasound to maternal height in the vaginal delivery group was lower, at 2.0 (1.94; 2.05), compared to 2.08 (2.02; 2.13) in the clinically narrow pelvis group (p<0.001).
Conclusion: The ratio of fetal head circumference to maternal height was lower in vaginal deliveries, measuring 2.0 versus 2.08 for the clinically narrow pelvis group. A fetal body weight of 3670 g and head circumference above 342.15 mm, as measured by ultrasound one week before the onset of labor, likely represent the threshold beyond which the probability of cephalopelvic disproportion significantly increases.
Authors' contributions: Baev O.R. – conception and design of the study; Tysyachnyi O.V. – data collection and processing, statistical analysis, visualization, drafting of the manuscript; Babich D.A. – editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Tysyachnyi O.V., Babich D.A., Baev O.R. Anthropometric predictors of cephalopelvic disproportion.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (10): 53-61 (in Russian)
https://dx.doi.org/10.18565/aig.2025.160
Keywords
Maternal-fetal pelvic size discrepancy, also known as cephalopelvic disproportion, occurs with a frequency of 1.3–17% and is associated with a high rate of operative delivery, as well as obstetric and neonatal morbidity and mortality [1–3].
Currently, pelvimetry based on classical data to predict cephalopelvic disproportion is considered ineffective. This is because normative values were established in the mid-20th century for women of European descent and do not account for variations in ethnicity and height [4].
Recent studies have indicated that a 1 cm increase in a woman's height is inversely correlated with cesarean section rates due to a clinically narrow pelvis, with an odds ratio of 0.67 (95% CI 0.64–0.70) [5]. However, clinical discrepancies can also arise with lower fetal weights, particularly in women with anatomical pelvic narrowing and short stature [6]. Moreover, evidence suggests that the ratio of fetal head circumference to maternal height, rather than fetal weight, significantly influences the development of a clinically contracted pelvis [7].
Consequently, research on the course of pregnancy and the anthropometric data of women and fetuses at full-term pregnancy in Russia is essential for identifying risk groups for clinically contracted pelvises.
This study aimed to examine the predictive power of anthropometric data of women and fetuses at full-term pregnancy concerning the risk of clinically contracted pelvises.
Materials and methods
From May 1 to May 31, 2025, we conducted a retrospective cohort study analyzing 12,034 birth records from the electronic database for 2024–2025 at V.I. Kulakov National Medical Research Center for Obstetrics and Gynecology, Ministry of Health of Russia.
Inclusion Criteria: Women of Slavic descent, primiparous, aged 18–40 years, with a spontaneously conceived singleton pregnancy, fetal cephalic presentation, gestational age ≥36 weeks, and a fetal ultrasound performed no later than one week before delivery.
Exclusion Criteria: Severe somatic pathology, complicated pregnancy (preeclampsia, gestational hypertension, gestational diabetes mellitus), cesarean section due to fetal distress or labor anomalies, uterine anomalies, fetal malformations, and fetal compromise as indicated by functional studies (cardiotocography, Doppler ultrasound).
The sample size was calculated using the sample size calculator from https://medstatistic.ru/calculators/calcsize.html using the following equation:

where significance level α = 0.05; variable A = 1.96 (with a study power of 80%); variable B = 0.84; confidence coefficient (t) = 3; maximum permissible error (Δ) = 2.
The standard deviation for the primary study parameter (σ), obtained in the pilot study [8], was 591, and the minimum clinically significant difference (δ) was 123.
Based on these results, the required sample size was determined to be at least 363 participants, with 181 participants in each group.
Clinical data regarding the mothers' pregnancies and the children's information were obtained from archival birth and newborn records. Clinical and anamnestic data, pregnancy and childbirth characteristics, fetal ultrasound data performed no later than one week before delivery, and the condition of the children at birth were analyzed. A total of 1,098 women met the inclusion criteria and were included in the study.
After selection based on the inclusion criteria, the women were divided into two groups. The control group (n=915) comprised women who delivered vaginally, while the study group (n=183) included women who underwent cesarean section due to a clinical mismatch between the maternal pelvis and fetal size.
The outcome of interest was the diagnosis of cephalopelvic disproportion based on maternal anthropometric parameters (height, weight, body mass index [BMI]) and fetal ultrasound parameters (biparietal diameter [mm], fronto-occipital diameter [mm], head circumference [mm], estimated body weight [g], estimated body weight [percentile], abdominal circumference [mm], and femur length [mm]).
The study was reviewed and approved by the Research Ethics Committee of V.I. Kulakov NMRC for OG&P.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 27 for Windows. The hypothesis of a normal distribution was tested using the Kolmogorov–Smirnov test. Continuous variables with a non-normal distribution were described using the median (Me) and lower and upper quartiles (Q1; Q3). The Mann–Whitney U test was used to assess the association between the development of cephalopelvic disproportion and maternal anthropometric and fetal ultrasound parameters. The critical level of statistical significance was set at p<0.05.
To predict the outcome of interest (cesarean section due to clinically narrow pelvis), binary logistic regression was used to calculate the individual predicted probabilities of developing the outcome based on clinical and ultrasound data. Independent variables with p<0.05 in the univariate analysis were tested for collinearity (correlation or interaction) and included in the multivariate model using a forward stepwise approach. The Spearman correlation coefficient was calculated to identify the correlations between the variables. Logistic regression was employed to determine the significance of the studied factors and construct a model. The probability of fetal growth restriction was calculated using the formula: P=1/(1+e-z), where P is the probability value; e is the base of the natural logarithm (e=2.72); z=β1X1+β2X2+…+βnXn+α, with β as the regression coefficients, α as a constant, and Xi as the values of the independent variables.
The resulting probabilities were used to evaluate the predictive ability of the model by constructing receiver operating characteristic (ROC) curves and calculating the area under the curve (AUC). An AUC of 0.9–1.0 indicated a very high predictive value, whereas an AUC of 0.5–0.6 indicated a poor predictive value.
Results
The women's characteristics, medical and gynecological histories, and pregnancy progression are presented in Table 1.
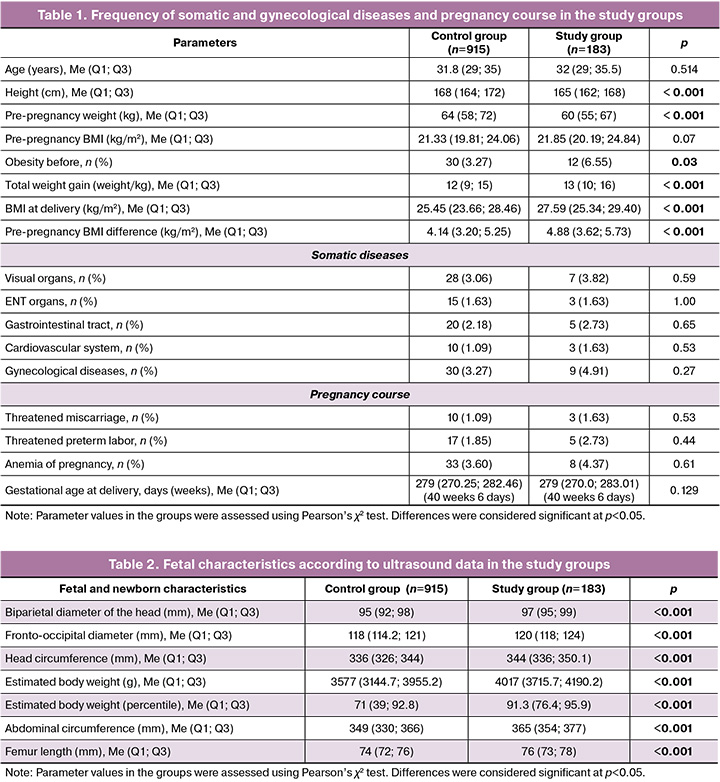
The ages of the patients included in this study were similar. An assessment of weight and height revealed that the pregnant women in the study group were shorter (165 cm vs. 168 cm) and had a higher incidence of obesity and total weight gain (6.55% vs. 3.27% and 13 kg vs. 12 kg, respectively). Furthermore, the BMI at delivery and the difference between the pre-pregnancy and post-partum BMI were higher in the study group (27.59 kg/m² vs. 25.45 kg/m² and 4.88 kg/m² vs. 4.14 kg/m², respectively).
Analysis of the medical and gynecological histories and pregnancy progression revealed no differences between the groups.
We assessed the differences in fetal ultrasound results between the groups. The results showed that all anthropometric parameters were higher in the study group (Table 2).
In the next step, we conducted a univariate linear regression analysis for each indicator, where differences were identified to assess their impact on the development of cephalopelvic disproportion (Table 3). In the regression analysis, a clinically narrow pelvis was used as the dependent (response) variable, and maternal anthropometric parameters and fetal ultrasound parameters were used as independent (predictor) variables.

In the next step, to include the combination of independent variables (head circumference and fetal birth weight) in the overall model, we checked for collinearity. The collinearity index (VIF) for both parameters was 1.810, indicating that the resulting model was robust to potential biases caused by the interaction.
The p-values for the Wald test for head circumference and estimated fetal birth weight based on ultrasound were 0.028 and 0.001, respectively, which are statistically significant predictors of the development of cephalopelvic disproportion. Moreover, with each millimeter increase in fetal head circumference measured by ultrasound, the likelihood of developing cephalopelvic disproportion increased by 1.03 times (or 3%). For fetal body weight, this indicator was 1.003 (or 0.3%), indicating that each gram of body weight increased the likelihood of cephalopelvic disproportion by 0.3%. The remaining independent variables were statistically insignificant in predicting dependent variables.

To assess the prognostic significance of fetal head circumference and body weight measured by ultrasound performed one week before delivery in predicting clinically narrow pelvises, binary logistic regression followed by ROC analysis was conducted in our population (Figure). The presence (1) or absence (0) of cephalopelvic disproportion was considered a binary predictor, whereas head circumference and fetal body weight were considered continuous. When conducting logistic regression to predict a clinically narrow pelvis based on fetal head circumference, the following standard equation was obtained: P=1/(1+e-z), where z=-20.2497+0.0558×head circumference (mm). The area under the ROC curve was 0.68 (95% CI 0.637–0.724), p<0.001, with a cut-off value of P=0.2391, corresponding to a fetal head circumference of 342.15 mm, with a sensitivity of 56.5% and a specificity of 70.1%. The positive predictive value of the result was 33.83%, the negative predictive value was – 85.54%, and the accuracy was 67.07%, as presented in Table 4. The Wald test was 46.165; OR 1.056 (95% CI 1.039–1.072), p<0.001.
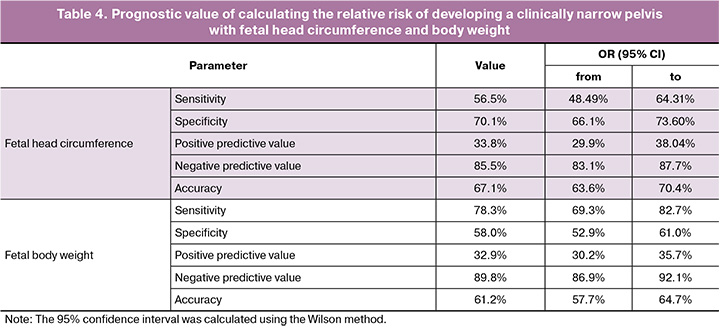
When conducting logistic regression to predict a clinically narrow pelvis based on fetal weight, the following standard equation was obtained: P=1/(1+e-z), where z=-9.0498+0.0021×fetal weight (g). The area under the receiver operating characteristic (ROC) curve was 0.744 (95% CI 0.706–0.782), p<0.001, with a cutoff of P=0.2071, corresponding to a fetal weight of 3670 g, with a sensitivity of 78.3% and specificity of 58%. The positive predictive value of the result was 32.90%, the negative predictive value was 89.79%, and the accuracy was 61.20%, as presented in Table 4. The Wald test was 72.642; OR 1.002 (95% CI 1.002–1.002), p<0.001.
When conducting logistic regression to predict a clinically narrow pelvis based on head circumference and fetal weight, the following standard equation was obtained: P=1/(1+e-z), where z=-14.6194+0.0189×head circumference (mm)+0.0018×fetal weight (g). The area under the receiver operating characteristic (ROC) curve was 0.750 (95% CI 0.712–0.788), p<0.001, with a fetal weight cutoff of P=0.1607, yielding a sensitivity of 83.2% and a specificity of 56.2%. The positive predictive value (PPV) of the result was 34.1%, the negative predictive value (NPV) was 92.5%, and the accuracy was 62.0% (Table 4).
The interpretation of the risk of developing cephalopelvic disproportion using the developed mathematical model is as follows.
For example, the fetal head circumference according to ultrasound was 343.18 mm, and the fetal weight was 3670 g. Therefore, P=1/(1+e-z), where z=-14.6194+0.0189×343.18+0.0018×3670; z=-1.5273; P=0.1784, indicating a low risk of cephalopelvic disproportion.
In the next step, we analyzed the incidence of a clinically narrow pelvis based on the head circumference and fetal weight obtained from the ROC analysis. For this purpose, all women in the study were divided into four groups based on head circumference and fetal weight, as determined by ultrasound data. The analysis revealed that the highest incidence of a clinically narrow pelvis was diagnosed with a head circumference >342.15 mm and fetal weight >3670 g, as presented in Table 5.
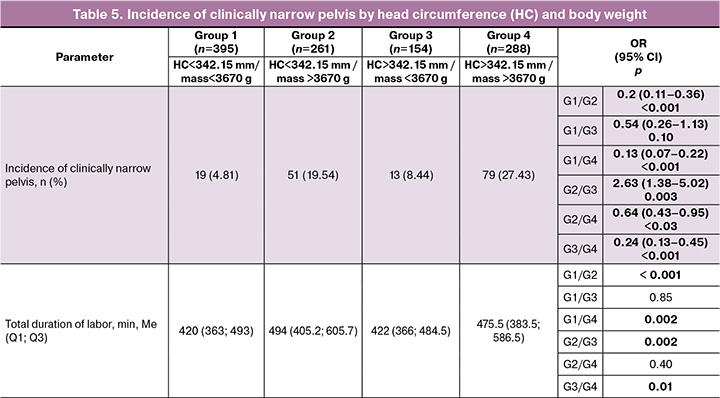
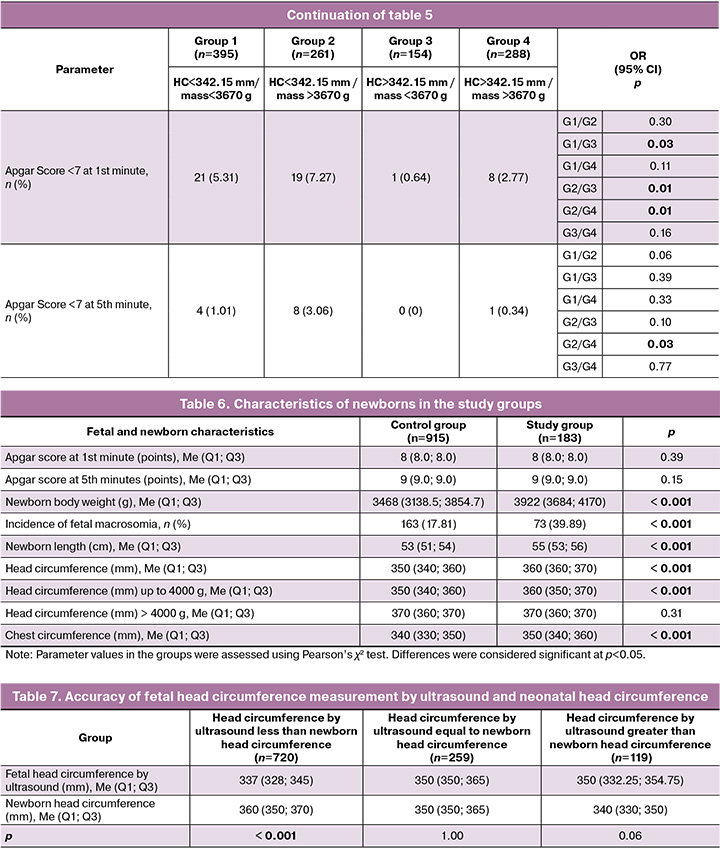
Anthropometric data analysis of newborns (Table 6) consistently revealed significantly higher fetal weight, incidence of fetal macrosomia, fetal length, and head and chest circumferences in the study group (p<0.001). When assessing the head circumference of newborns weighing up to 4000 g, it was found to be larger in the clinically narrow pelvis group (360 mm vs. 350 mm, p<0.001). No differences were found for fetuses weighing >4000 g – 370 mm vs. 370 mm (p=0.31).
A comparative analysis was conducted to determine the comparability of fetal head circumference measurements based on ultrasound and neonatal head circumferences. The results showed that in 65.57% (720/1098) of observations, the fetal head circumference was smaller according to ultrasound data; in 23.58% (259/1098), the measurements were the same; and in 10.83% (119/1098), the circumference according to ultrasound data was larger (Table 7).
Next, we analyzed the ratio of fetal head circumference to the mother’s height using ultrasound. The results showed that the median for the vaginal delivery group was lower and amounted to 2.0 (1.94; 2.05) vs. 2.08 (2.02; 2.13) for the clinically narrow pelvis group (p<0.001).
Discussion
In our study, we examined the predictive value of maternal and fetal anthropometric data at full-term pregnancy for the risk of developing a clinically narrow pelvis.
According to Meyer R. et al. (2016), the incidence of cesarean section is inversely related to maternal height, ranging from 41.0% for women with a height of ≤150 cm to 13.1% for those with a height of ≥166 cm [5].
After analyzing the women's anthropometric data, we found that the average height of pregnant women in the vaginal delivery group was greater. In contrast, pre-pregnancy weight, BMI, total weight gain, and BMI at delivery were higher in the clinically narrow pelvis group. The literature indicates that weight loss during pregnancy enhances the rate of vaginal delivery among overweight [OR 1.12 (95% CI 1.01–1.25)] and obese [OR 1.24 (95% CI 1.04–1.48)] women, compared to those who maintained their weight [9]. Furthermore, an increase in BMI of >2 kg/m² elevates the likelihood of cesarean section during childbirth from 4.5% to 7.4% [OR 1.78 (95% CI 1.10–2.86)] [10]. Our findings support those of previous studies, underscoring the critical importance of weight changes before and during pregnancy in preventing adverse gestational outcomes.
Next, we assessed the fetuses using ultrasound data to predict a clinically narrow pelvis. The results indicated that all measured parameters were higher in fetuses that underwent surgical delivery due to a clinically narrow pelvis.
Previous studies have shown that fetal macrosomia is not a definitive factor for the development of a clinically narrow pelvis. The likelihood of cesarean section increases with fetal body weight exceeding 3500 g [OR 1.8 (95% CI 1.3–2.7)] [11]. Additionally, a head circumference ≥35 cm raised the frequency of cesarean sections [OR 2.49 (95% CI 1.40–2.18)] when compared with a size <35 cm. Similarly, a fetal weight ≥3900 g corresponds to an increased likelihood of cesarean section [OR 2.90 (95% CI 2.48–3.39)] compared to weights <3900 g [12].
To evaluate the predictive value of fetal head circumference and birth weight based on ultrasound data obtained one week before delivery, we conducted a receiver operating characteristic (ROC) analysis. The results indicated that, for our population, the cutoff value for fetal head circumference was 342.15 mm (sensitivity 56.5%, specificity 70.1%), and the cutoff for birth weight was 3670 g (sensitivity 78.3%, specificity 58%).
Current data suggest that the ratio of fetal head circumference to maternal height, rather than fetal birth weight, significantly influences the development of a clinically narrow pelvis. Consequently, cesarean sections due to a clinically narrow pelvis are associated with lower maternal height (160.4 cm versus 164.5 cm), larger fetal head circumference (339.6 mm versus 330.7 mm), and a higher fetal head circumference to maternal height ratio (2.12 versus 2.01) compared to vaginal deliveries, making it a risk factor for cesarean section [OR 2.65 (95% CI 1.85–3.79), p<0.001] [7].
Our data indicated that the fetal head circumference to maternal height ratio in the clinically narrow pelvis group was lower, measuring 2.0 compared to 2.08 (p<0.001).
Conclusion
Based on the data presented, we can infer that a fetal body weight of ≥ 3670 g and a head circumference greater than 342.15 mm, as determined by ultrasound performed one week before the onset of labor, likely represent the threshold beyond which the likelihood of cephalopelvic disproportion increases significantly.
References
- Чернуха Е.А., Волобуев А.И., Пучко Т.К. Анатомически и клинически узкий таз. М.: Триада-Х; 2005. 256 с. [Chernukha E.A., Volobuev A.I., Puchko T.K. Anatomically and clinically narrow pelvis. Moscow: Triada-X; 2005. 256 p.(in Russian)].
- Ayenew A.A. Incidence, causes, and maternofetal outcomes of obstructed labor in Ethiopia: systematic review and meta-analysis. Reprod. Health. 2021; 18(1): 61. https://dx.doi.org/10.1186/s12978-021-01103-0
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Медицинская помощь матери при установленном или предполагаемом несоответствии размеров таза и плода. Лицевое, лобное или подбородочное предлежание плода, требующее предоставления медицинской помощи матери. 2023. [Ministry of Health of the Russian Federation. Clinical guidelines. Medical care for the mother in case of established or suspected discrepancy between the size of the pelvis and the fetus. Facial, frontal, or submental presentation of the fetus requiring medical care for the mother. 2023. (in Russian)].
- Betti L., Manica A. Human variation in the shape of the birth canal is significant and geographically structured. Proc. Biol. Sci. 2018; 285(1889): 20181807. https://dx.doi.org/10.1098/rspb.2018.1807
- Meyer R., Yinon Y., Levin G. Vaginal delivery rate by near delivery sonographic weight estimation and maternal stature among nulliparous women. Birth. 2023; 50(3): 557-64. https://dx.doi.org/10.1111/birt.12679
- Cohen G., Schreiber H., Shalev‐Ram H., Biron‐Shental T., Kovo M. Do neonatal birth weight thresholds for labor dystocia outcomes differ between short and normal stature women? Int. J. Gynecol. Obstet. 2024; 166(3): 1023-30. https://dx.doi.org/10.1002/ijgo.15139
- Dall’Asta A., Ramirez Zegarra R., Corno E., Mappa I., Lu J.L.A., Di Pasquo E. et al. Role of fetal head‐circumference‐to‐maternal‐height ratio in predicting Cesarean section for labor dystocia: prospective multicenter study. Ultrasound Obstet. Gynecol. 2023; 61(1): 93-8. https://dx.doi.org/10.1002/uog.24981
- Meyer R., Tsur A., Tenenbaum L., Mor N., Zamir M., Levin G. Sonographic fetal head circumference is associated with trial of labor after cesarean section success. Arch. Gynecol. Obstet. 2022; 306(6): 1913-21. https://dx.doi.org/10.1007/s00404-022-06472-w
- Callegari L.S., Sterling L.A., Zelek S.T., Hawes S.E., Reed S.D. Interpregnancy body mass index change and success of term vaginal birth after cesarean delivery. Am. J. Obstet. Gynecol. 2014; 210(4): 330.e1-7. https://dx.doi.org/10.1016/j.ajog.2013.11.013
- Kawakita T., Franco S., Ghofranian A., Thomas A., Landy H.J. Interpregnancy body mass index change and risk of intrapartum cesarean delivery. Am. J. Perinatol. 2021; 38(08): 759-65. https://dx.doi.org/10.1055/s-0040-1721698
- Little S.E., Edlow A.G., Thomas A.M., Smith N.A. Estimated fetal weight by ultrasound: a modifiable risk factor for cesarean delivery? Am. J. Obstet. Gynecol. 2012; 207(4): 309.e1-6. https://dx.doi.org/10.1016/j.ajog.2012.06.065
- Lipschuetz M., Cohen S.M., Israel A., Baron J., Porat S., Valsky D.V. et al. Sonographic large fetal head circumference and risk of cesarean delivery. Am. J. Obstet. Gynecol. 2018; 218(3): 339.e1-7. https://dx.doi.org/10.1016/j.ajog.2017.12.230
Received 18.06.2025
Accepted 08.10.2025
About the Authors
Oleg V. Tysyachnyi, PhD, Researcher at the 1st Maternity Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,Ministry of Health of Russia, 117997, Russia, Moscow, Oparina str., 4, o_tysyachny@oparina4.ru, https://orcid.org/0000-0001-9282-9817
Dmitry A. Babich, PhD, obstetrician-gynecologist at the 1st Maternity Department, Associate Professor at the Department of Continuous Professional Education and Simulation Technologies, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia,
117997, Russia, Moscow, Oparina str., 4, d_babich@oparina4.ru, https://orcid.org/0000-0002-3264-2038
Oleg R. Baev, Dr. Med. Sci., Head of the 1st Maternity Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,
Ministry of Health of Russia, 117997, Russia, Moscow, Oparina str., 4; Professor at the Department of Obstetrics, Gynecology, Perinatology and Reproductology,
I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia, +7(495)438-11-88, o_baev@oparina4.ru, https://orcid.org/0000-0001-8572-1971