Myomectomy during cesarean section
Krot I.F., Rukhlyada N.N., Romanova L.A., Reznik V.A., Sergienko O.I., Chikhladze B.U., Vartanyan R.A.
Objective: The purpose of this study was to assess the feasibility of performing myomectomy during cesarean section using different techniques, the effect of extension of surgery on duration of operation, intraoperative blood loss, and the course of the postoperative period.
Materials and methods: The study was conducted at the Department of Pregnancy Pathology, the University Clinic of Saint Petersburg State Pediatric Medical University. The surgical protocols of 377 patients, who delivered babies through cesarean section, and the delivery histories of 69 women with uterine fibroids were investigated. The patients were divided into 2 groups: group 1 consisted of 24 women who underwent myomectomy during cesarean section and group 2 consisted of 45 patients, who did not undergo myomectomy.
Results: Uterine fibroids were diagnosed in 69/377 (18.3%) patients. Myomectomy during cesarean section was performed in 24/377 (6.4%). In 12/24 (50%) women, uterine fibroids were the major indication for surgical delivery. The total number of removed myoma nodules was 39. Most of removed myoma nodules were located on the anterior uterine wall and were divided by fibroid growth into interstitial (type 4), and interstitial-subserous (type 5). Different surgical techniques were used for removal of the nodules: fetal extraction before hysterotomy; in a typical manner; on the uterine cavity side (endometrial myomectomy); transmural route. Duration of operation in group 1 was longer, however, there was no significant difference in the length of fetal extraction and intraoperative blood loss. The newborns in both groups had no signs of hypoxia. Extension of surgery did not lead to postoperative complications.
Conclusion: The results obtained in the study confirm the feasibility of performing myomectomy during cesarean section and safety approach, that helps to improve immediate and long-term treatment results and has significant medical and cost effectiveness.
Authors' contributions: Krot I.F., Romanova L.A., Rukhlyada N.N., Reznik V.A. – the concept and design of the study; Krot I.F., Romanova L.A., Sergienko O.I., Chikhladze V.U., Vartanyan R.A. – material collection and processing; Krot I.F. – statistical data processing; Krot I.F., Romanova L.A. – article writing; Rukhlyada N.N., Reznik V.A. – article editing.
Conflicts of interest: The authors declare that they have no conflict of interest to declare.
Funding: The study was conducted without any sponsorship.
Ethical Approval: The study was approved by the local Ethics Committee of Saint Petersburg State Pediatric Medical University, Ministry of Health of the Russian Federation, Protocol No 32/10 of November 08, 2023.
Patient Consent for Publication: The patients signed informed consent for publication of their medical data that were obtained when receiving healthcare for the educational and scientific purpose without indication of their personal data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Krot I.F., Rukhlyada N.N., Romanova L.A., Reznik V.A., Sergienko O.I., Chikhladze B.U., Vartanyan R.A. Myomectomy during cesarean section.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2024; (2): 72-78 (in Russian)
https://dx.doi.org/10.18565/aig.2023.262
Keywords
Uterine fibroids are the most common gynecological disorder. According to some authors, it prevails in 20–70% of women of reproductive age [1–4]. The prevalence of uterine fibroids in pregnant women is 0.5–6% [3, 5–7], and is steadily increasing and correlates with advanced maternal age, the increasing use of assisted reproductive technologies, the prevalence of hormonal therapy and contraception, as well as endocrine disorders. During pregnancy, growth of uterine fibroids occurs in the first trimester [8]. Currently, there is no consensus on performing myomectomy during cesarean section. It is a known that Victor Bonney, a British gynecological surgeon performed the first myomectomy during caesarean section in 1913. He performed myomectomy (removed six large fibroids) in 30-year-old patient, and she had 3 vaginal births afterwards [9]. Over 100 years have passed since that publication, but the situation was not significantly clarified. Currently, there are no clear indications or description of techniques to perform myomectomy during cesarean section. Online information search for “myomectomy during cesarean section” is presented by descriptions of clinical cases in most publications in the Russian and English languages [10–17]. There are controversial opinions on advisability of myomectomy during cesarean section due to prolonged operative duration, larger wound surface area and increased blood loss, as well as possible complications, such as intraoperative hemorrhage, intramuscular hematoma formation in the area of surgical incision, postoperative purulent-septic complications, venous thromboembolism, abdominal adhesive disease and long-term complications associated with uterine scar and its effect on subsequent fertility [18–22]. Moreover, the area of expertise of the vast majority of today’s doctors is focused on obstetrics, and they have no necessary skills in gynecological surgery that allow them, if necessary, to extend surgical intervention to hysterotomy.
The latest clinical guidelines “Uterine fibroids” (2020) of the Ministry of Health of Russia indicate that during cesarean delivery it is advisable to perform myomectomy only in the presence of fibroids preventing extraction of the fetus [4]. However, most practicing obstetricians are well aware that postpartum uterine contractions lead to malnutrition and ischemia of large uterine fibroids, subinvolution and abnormal lochia after giving birth that worsens the course of the postpartum period. Broader indications for myomectomy during cesarean section are presented in the national guidelines “Obstetrics” (2018). It is stated there that myomectomy during cesarean section should be performed in the presence of subserous fibroids in thin layer in any accessible location, subserous fibroids at the wide base (excluding the lower segment), in the presence of no more than 5 large intramural fibroids > 10 cm (no more than one fibroid with centripetal growth (more than 10 cm (no more than one fibroid), with good access to fibroids in different locations, excluding intramural fibroids < 5 cm [1]. In addition, in the presence of multiple uterine fibroids with low location (cervical or isthmic fibroids), malignancy of the fibroid that is histologically confirmed during surgery, when the circumstances require ssimultaneous removal of the uterine appendages (ovarian tumors, tubo-ovarian masses), hysterectomy is indicated.
The technique for performing myomectomy to remove intramural (interstitial) uterine fibroids was described by V.I. Krasnopolsky [23]. The technique comprises performing a linear or oval uterine incision with a scalpel, until the capsule of fibroid is visualized, which is also dissected. Fibrous connective tissue is fixed with bullet forceps in the longitudinal direction and pulled into the wound. Fibroid is removed and the uterine fibroid bed is sutured with double-row or three-row of sutures. The disadvantage of this method is increased bleeding due to gestational changes in myometrium; hemostasis is time consuming due to injury of serous membrane of the uterus, and there is a risk adhesion development at the site of the injury to visceral peritoneum. The problems for providing effective hemostasis increase the duration of surgery, the amount of needed suture material, and the risk of early and late postoperative complications. Surgical techniques of endometrial myomectomy, which is performed during cesarean section through incision in the uterus, are described in literature [24].
Unfortunately, the latest mandatory clinical guidelines do not provide legal protection for doctors against extension of surgery during cesarean section. Under these circumstances, the surgeon is responsible for making a decision about the choice of surgical methods for myomectomy and surgical outcome.
The purpose of our study was to assess the feasibility of performing myomectomy during cesarean section using different techniques, the effect of extension of surgery on the duration of surgery, intraoperative blood loss, and the course of the postoperative period.
Materials and methods
The study was conducted at the Department of Pregnancy Pathology, the University Clinic of Saint Petersburg State Pediatric Medical University. The surgical protocols of 377 patients, who delivered babies through cesarean section, and the delivery histories of 69 women with uterine fibroids were investigated. The patients were divided into 2 groups: group 1 consisted of 24 women who underwent myomectomy during cesarean section and group 2 consisted of 45 patients, who did not undergo myomectomy. The medical histories, surgical protocols, laboratory data (clinical laboratory tests results, biochemical, bacteriological, histological findings) and instrumental data (ultrasound examination) were analyzed.
Statistical analysis
Statistical analysis of the data was performed using Statistica software program. The Lilliefors-corrected Kolmogorov–Smirnov test was used for normality of distribution of the parameters. Descriptive statistics for normal distribution of the data is presented as mean (M) and standard deviation (SD). The quantitative data that do not follow a normal distribution are presented as median and interquartile range – Me (Q1; Q3). Comparison of data sets for quantitative characteristics with a normal distribution was made using the independent samples T-test. Skewed distribution of data were analyzed using the Mann–Whitney U-test. The threshold value, that determined statistical significance, was considered as p=0.05. Descriptive statistics for qualitative data is presented as absolute frequency and relative frequency.
Results
Delivery records of 377 patients of the Department of Pregnancy Pathology, the University Clinic of Saint Petersburg State Pediatric Medical University, who underwent elective cesarean delivery in 2022, were investigated. Uterine fibroids were diagnosed in 69/377 (18.3%) patients. Myomectomy during cesarean section was performed in 24/377 (6.4%) patients. The decision about necessity to perform myomectomy taking into account personalized risks, was made collectively together with the deputy Chief Physician and the Head of the Department, on the day before surgery or intraoperatively. Depending on the volume of surgery, the patients were divided into 2 groups. Group 1 included 24 women who underwent myomectomy during cesarean section and group 2 consisted of 45 patients with uterine fibroids, who underwent elective cesarean delivery without extension of surgery to myomectomy. The mean age of patients in group 1 was 36/08 (4/4/) years versus 38.58 (5.1) years in group 2, p=0.048.
Detailed evaluation of the group of women who underwent myomectomy during cesarean section showed that in 12/24 (50%) women, uterine fibroids were the major indication for cesarean delivery due to the fact, that uterine fibroids were located in the isthmus of uterus along the anterior and posterior walls and would obstruct the passage of the fetus through the maternal birth canal, or due to very large fibroids that would lead to abnormalities of labor. A total of 39 uterine fibroids 2–15 cm in size were removed in 24 patients. The analysis of localization of removed fibroids showed that most of them were located on the anterior uterine wall – 23/39 (59.0%), 5/39 (12.8%) and 5/39 (12.8%) fibroids were removed from the anterior uterine wall in the region of isthmus and the fundus of the uterus, 3/39 (7.7%) and 3/39 (7.7%) were located on the posterior site of uterine isthmus and on the posterior wall of the uterus. According to the FIGO classification system for fibroids, most of removed fibroids 18/39 (46.1%) were intramural (type 4), 14/39 (35.9%) were subserosal/intramural (type 5), and 5/39 (12.8%) were subserosal (type 6–7). Submucosal and intramural fibroids (type 2–3) and intraligamentary fibroids (type 8) were removed less often – 1/39 (2.6%) and 1/39 (2.6%), respectively.
We could use various fibroid removal options. The final decision was made intraoperatively after the fibroid was assessed by visualization or palpation. For fetal extraction, myomectomy was performed to remove 2/39 (5.1%) fibroids before hysterotomy. These were the cases when large fibroids were located in the anterior uterine wall of the lower uterine segment in the area of incision of the uterus to remove the fetus. However, despite the abnormal signs of cesarean section, fetal extraction in these situations was performed at 4 and 5 minutes from the start of surgery and did not affect the Apgar birth scores for newborns. More than half of uterine fibroids 22/39 (56.4%) were removed using traditional surgical technique after opening uterine serous membrane [23]. However, in these cases, we made sagittal incision above the fibroid that was 2 times smaller than the size of palpated fibroid. Adequate uterine contractility and smaller incision size makes it possible to reduce the number of complications associated with hemostasis of the wound. Myomectomy of 2/39 (5.1%) fibroids, which is called endometrial myomectomy, was performed at the site of uterine cavity. In our opinion, this technique is most successful for submucosal/intramural and intramural fibroids. Postpartum uterine plasticity allows expulsion of the fibroid during palpation in the direction desirable for the surgeon. Surgery performed without damaging uterine serous membrane has the advantage of reducing intraoperative blood loss. In 13/39 (33.3%) cases, transmural myomectomy was performed, when intramural fibroid was located on the anterior wall of the uterus at a distance of no more than 4 cm from the edge of uterine incision in caesarean section. The performance of myomectomy in this case was as follows: the classical cesarean section was performed. The transverse uterine incision was done in the lower segment. Then the size, location and the growth pattern of uterine fibroid was determined by visual examination and palpation. When intramural fibroid (type 3–5 according to the FIGO classification) measuring 5 cm was located in the anterior wall of the uterus at a distance of no more than 4 cm from the edge of the hysterotomy incision, transverse uterine muscle splitting incision was performed at the site of hysterotomy incision in cesarean section.
The lower pole of fibroid was reached through formation of the tunnel, the capsule of fibroid was opened, the fibroid was grasped with bullet forceps, the fibroid was enucleated using a combination of sharp and blunt dissection. The length of the incision and the depth of the tunnel depend on the size of fibroid. Then, uterine fibroid bed and the tunnel made for its removal were sutured using U-shaped suture technique through uterine wall thickness, and the knots were tied involving the uterine serous membrane. The number of U-shaped sutures depends on the size of the removed fibroid. We believe that transmural myomectomy during cesarean section leads to reduction of uterine injuries, preserving the structural integrity of uterine serous membrane, reduction of intraoperative bleeding intensity, shortening the operative time, lesser amount of suture material, and lower number of postoperative complications [25].
Cesarean section and myomectomy was performed in 11/24 (45.8%) women, who underwent additional surgical procedures. In particular, 7/24 (29.2%) patients underwent uterine devascularization by ligation of the branches of the uterine arteries: 1/24 (4/2%) patient underwent ovariocystectomy and 1/24 (4/2%) patient underwent adhesiolysis. Endometrial myomectomy was performed on one of the patients, and intrauterine Zhukovsky balloon catheter was used to prevent bleeding in the early postoperative period. One patient in the group of cesarean section with myomectomy underwent hysterectomy. This was patient Z, aged 38 years, who gave birth the second time and had multiple large uterine fibroids, that were located in the isthmus of the uterus. Intraoperative examination found that the size of dominant intramural fibroid No.1 was 15 cm. It was located in the isthmus of uterus along the posterior wall, and deformation of the uterine cavity was due to its size. Below fibroid No.1, subserosal fibroid No. 2 with restricted mobility, 8 cm in diameter, was visually determined in the uterine isthmus. Given a high risk of massive intraoperative hemorrhage in myomectomy, due to the topography and size of fibroids, the intraoperative concilium made a decision to perform total hysterectomy without removal of the appendages.
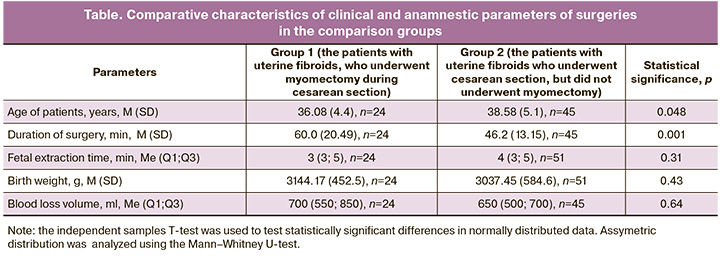
The comparative analysis of surgeries performed in the groups and surgical outcomes included duration of surgical intervention, the time of fetal extraction, blood loss, the length of postoperative period in patients in group 1 (who underwent myomectomy during cesarean section, n=24) and in patients in group 2 (who had uterine fibroids, but did not underwent myomectomy during cesarean section, n=45) (Table). It was found that duration of surgical intervention was significantly longer in patients in group 1, and was 60.0 (20.49) minutes versus 46,2 (13.15) minutes in group 2, p=0.001. In group 2, 6 pregnant women gave birth to twins, and 45 patients gave birth to 51 infants. There was no statistically significant difference between the groups in the time of fetal extraction from the start of surgery – 3 (3; 5) minutes in group 1 and 4 (3; 5) minutes in group 2, p=0.31. There was no statistically significant difference between the groups in intraoperative blood loss – 700 (550; 850) ml in group 1 and 650 (500; 700) ml in group 2, p=0.64. Uterine fibroids had no significant effect on the weight and condition in newborns. The babies in both groups were born without hypoxia weighing 3144.17 (452.5) g in group 1 and 3037.45 (584.6) g in group 2, p=0,43. In the postoperative period, antimicrobial therapy with ceftriaxone daily dose of 2.0 g for 5 days was indicated. Low molecular weight heparin was indicated for the prevention of venous thromboembolism. The duration of intake depended on the calculated risk of venous thromboembolism. Extension of surgery did not lead to occurrence of postoperative complications. The puerperant women in both groups were timely discharged from hospital on day 4–6 in the postpartum period.
Conclusion
The rational approach to planning and performance of myomectomy during abdominal delivery does not lead to increased blood loss and other intra- and postoperative complications. Myomectomy during cesarean section should be performed by a multidisciplinary team at level 3 facility. The surgical team should include surgeons (who have experience in hysterotomy technique, ligation of blood vessels, different suturing techniques), anesthesiologist, transfusiologist, and neonatologist. Preoperative preparation requires thorough physical examination, including ultrasound and magnetic resonance imaging for an accurate topographic description of the tumor. It is necessary to communicate with the patient regarding peculiarities of surgery, risks and possible intraoperative complications, and obtain informed consent to perform cesarean section with expansion of surgical intervention to hysterectomy. The risk of intraoperative blood loss is reduced by preoperative blood components procurement for possible blood transfusion, the use of blood-saving techniques (intraoperative reinfusion of blood), and surgical hemostatic technologies. The technique for optimizing myomectomy depends on the location of fibroid, its growth pattern, and surgeon’s preferences. Traditionally, myomectomy can be performed by transmural access through surgical wound, opening serous membrane over the fibroid and further enucleation of the fibroid via trans-endometrial approach. The results obtained in the study confirm the feasibility of performing myomectomy during cesarean section and safety approach, that helps to improve immediate and long-term treatment results and has significant medical and cost effectiveness.
References
- Савельева Г.М., Сухих Г.Т., Серов В.Н., Радзинский В.Е., ред. Акушерство. Национальное руководство. М.: ГЭОТАР-Медиа; 2018; 1088 с. [Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., eds. Obstetrics. National Guide. M.: GEOTAR-Media; 2018. 1088 р. (in Russian)].
- Сидорова И.С., Унанян А.Л., Агеев М.Б., Ведерникова Н.В., Жолобова М.Н. Современное состояние вопроса о патогенезе, клинике, диагностике и лечении миомы матки у женщин репродуктивного возраста. Акушерство, гинекология и репродукция. 2012; 4: 22-8. [Sidorova I.S., Unanyan A.L., Ageev M.B., Vedernikova N.V., Zholobova M.N. The current state of the issue of the pathogenesis, clinic, diagnosis and treatment of uterine fibroids in women of reproductive age. Obstetrics, Gynecology and Reproduction. 2012; (4): 22-8. (in Russian)].
- Савельева Г.М., Серов В.Н., Сухих Г.Т., ред. Клинические рекомендации. Акушерство и гинекология. 4-е изд. М.: ГЭОТАР-Медиа; 2019. 1008 с. [Savelyeva G.M., Serov V.N., Sukhikh G.T., ed. Clinical guidelines. Obstetrics and gynecology. 4th edition, revised and expanded. Moscow: GEOTAR-Media; 2019. 1008 p. (in Russian)].
- Министерство здравоохранения Российской Федерации. Клинические рекомендации «Миома матки». 2020. [Ministry of Health of the Russian Federation. Clinical guidelines "Uterine fibroids". 2020. (in Russian)].
- Guler A.E., Guler Z.Ç.D., Kinci M.F., Mungan M.T. Myomectomy during cesarean section: why do we abstain from? J. Obstet. Gynaecol. India. 2020; 70(2): 133-7. https://dx.doi.org/10.1007/s13224-019-01303-6.
- Loverro G., Damiani G.R., Malvasi A., Loverro M., Schonauer L.M., Muzzupapa G., Dinaro E. Myomectomy during pregnancy: an obstetric overview. Minerva Obstet. Gynecol. 2021; 73(5): 646-53. https://dx.doi.org/10.23736/S2724-606X.21.04676-5.
- Тайц А.Н., Рухляда Н.Н., Матухин В.И., Сомова А.Д., Дудова К.А. Современные представления о патогенезе миомы матки. Педиатр. 2019; 10(1): 91-9. [Taits A.N., Ruhljada N.N., Matukhin V.I., Somova A.D., Dudova K.A. Contemporary concepts of uterine fibroids’ pathogenesis. Pediatrician (St. Petersburg). 2019; 10(1): 91-9. (in Russian)]. https://dx.doi.org/10.17816/PED10191-99.
- Rosati P., Exacoustòs C., Mancuso S. Longitudinal evaluation of uterine myoma growth during pregnancy. A sonographic study. J. Ultrasound. Med. 1992; 11(10): 511-5. https://dx.doi.org/10.7863/jum.1992.11.10.511.
- Jauniaux E., Khan K.S. Caesarean myomectomy: Victor Bonney reports the first case in 1913. BJOG. 2014; 121(2): 193. https://dx.doi.org/10.1111/1471- 0528.12548.
- Garg P., Bansal R. Cesarean myomectomy: a case report and review of the literature. J. Med. Case Rep. 2021; 15(1): 193. https://dx.doi.org/10.1186/s13256-021-02785-7.
- Goyal M., Dawood A.S., Elbohoty S.B., Abbas A.M., Singh P., Melana N., Singh S. Cesarean myomectomy in the last ten years; A true shift from contraindication to indication: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021; 256: 145-57. https://dx.doi.org/10.1016/j.ejogrb.2020.11.008.
- O' Sullivan R., Abder R. Myomectomy at the time of cesarean delivery. Ir. J. Med. Sci. 2016; 185(4): 973-5. https://dx.doi.org/10.1007/s11845-015-1378-2.
- Бабунашвили Е.Л., Буянова С.Н., Новикова С.В., Гукасян С.А., Юдина Н.В., Ермолаева Е.Е. Кесарево сечение и миомэктомия гигантского перешеечно-интралигаментарного узла. Российский вестник акушера-гинеколога. 2019; 19(5): 68-71. [Babunashvili E.L., Buianova S.N., Novikova S.V., Gukasian S.A., Iudina N.V., Ermolaeva E.E. Cesarean section and a myomectomy of a giant atypical uterine fibroid. Russian Bulletin of Obstetrician-Gynecologist. 2019; 19(5): 68-71. (in Russian)]. https://dx.doi.org/10.17116/rosakush20191905168.
- Тусупкалиев А.Б., Балмагамбетова С.К., Дарибай Ж.Ж., Карманова А.А. Консервативная миомэктомия субмукозного узла при кесаревом сечении Медицинский журнал Западного Казахстана. 2012; 4: 133-5. [Tusupkaliev A.B., Balmagambetova S.K., Daribay Zh.Zh., Karmanova A.A. Conservative myomectomy of submucouse node while caesarian section. West Kazakhstan Medical Journal. 2012; (4): 133-5. (in Russian)].
- Özcan A., Kopuz A., Turan V., Sahin C., Töz E., Aksoy S., Ozeren M. Cesarean myomectomy for solitary uterine fibroids: Is it a safe procedure? Ginekol. Pol. 2016; 87(1): 54-8. https://dx.doi.org/10.17772/gp/57833.
- Курцер М.А., Лукашина М.В., Тищенко Е.П. Консервативная миомэктомия во время кесарева сечения. Вопросы гинекологии, акушерства и перинатологии. 2008; 7(3): 82-7. [Kurtser M.A., Lukashina M.V., Tishchenko E.P. Conservative myomectomy during cesarean section. Gynecology, Obstetrics and Perinatology. 2008; 7(3): 82-7. (in Russian)].
- Каримов З.Д., Ниязматова Г.И., Абдикулов Б.С., Хусанходжаева М.Т., Тухтабаева Б.М. Органосберегающее хирургическое лечение миомы матки во время беременности. Акушерство и гинекология. 2009; 6: 31-3. [Karimov Z.D., Niyazmatova G.I., Abdikulov B.S., Khusankhodzhayeva M.T., Tukhtabayeva B.M. Organ-preserving surgical treatment for uterine myoma during pregnancy. Obstetrics and Gynecology. 2009; (6): 31-3. (in Russian)].
- Huang Y., Ming X., Li Z. Feasibility and safety of performing cesarean myomectomy: a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2022; 35(13): 2619-27. https://dx.doi.org/10.1080/14767058.2020.1791816.
- Маринкин И.О., Пивень Л.А., Пушкарев Г.А. Дискуссионные вопросы миомэктомии при кесаревом сечении. Журнал акушерства и женских болезней. 2013; 62(4): 106-11. [Marinkin I.O., Piven L.A., Pushkarev G.A. Debatable issues of myomectomy in case of caesarean operation. Journal of obstetrics and women's diseases. 2013; 62(4): 106-11. (in Russian)]. https://dx.doi.org/10.17816/JOWD624106-111.
- Беженарь В.Ф., Долинский А.К. Мнение редакции о статье «Дискуссионные вопросы миомэктомии при кесаревом сечении». Журнал акушерства и женских болезней. 2013; 62(4): 112-3. [Bezhenar V.F., Dolinskiy A.K. Editorial opinion on the article "Discussion issues of myomectomy in caesarean section". Journal of obstetrics and women's diseases. 2013; 62(4): 112-3. (in Russian)].
- Буянова С.Н., Бабунашвили Е.Л., Логутова Л.С., Щукина Н.А., Юдина Н.В., Гукасян С.А., Кащук М.Г., Ермолаева Е.Е., Ахвледиани К.Н., Магилевская Е.В., Стоцкая Т.В. Взгляд на проблему миомэктомии при беременности и во время кесарева сечения. Акушерство и гинекология. 2020; 8: 22-8. [Buyanova S.N., Babunashvili E.L., Logutova L.S., Shchukinа N.A., Yudinа N.V., Gukasyan S.A., Kashchuk M.G., Ermolaeva E.E., Akhvlediani K.N., Magilevskaya E.V., Stotskaya T.V. A look at the problem of myomectomy during pregnancy and cesarean section. Obstetrics and Gynecology. 2020; (8): 22-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2020.8.22-28.
- Пекарев О.Г., Майбородин И.В., Пекарева Е.О., Поздняков И.М., Попова С.П. Опыт самопроизвольного родоразрешения женщин с рубцом на матке после миомэктомии. Акушерство и гинекология. 2012; 5: 88-92. [Pekarev O.G., Maiborodin I.V., Pekareva E.O., Pozdnyakov I.M., Popova S.P. Experience with spontaneous delivery in women with a uterine scar after myomectomy. Obstetrics and Gynecology. 2012; (5): 88-92. (in Russian)].
- Краснопольский В.И., Буянова С.Н., Щукина Н.А., Попов А.А. Оперативная гинекология. М.: МЕДпресс-информ; 2018. 320 р. [Krasnopolsky V.I., Buyanova S.N., Shchukina N.A., Popov A.A. Operative gynecology. Moscow: MEDpress-inform; 2018. 320 р. (in Russian)].
- Wang Q., Lin J., Dai Y. Outcomes of cesarean myomectomy via trans-endometrial approach in women with single intramural fibroid in the posterior uterine wall. J. Matern. Fetal Neonatal Med. 2023; 36(2): 2232655. https://dx.doi.org/10.1080/14767058.2023.2232655.
- Крот И.Ф., Романова Л.А., Рухляда Н.Н., Сергиенко О.И., Чихладзе В.У., Вартанян Р.А. Способ миомэктомии. МПК А61В 17/00. Заявка №202392091 принята Евраз. Пат. Ведомством 11.08.23. [Krot I.F., Romanova L.A., Rukhlyada N.N., Sergienko O.I., Chikhladze V.U., Vartanyan R.A. Method of myomectomy MPC A61B 17/00. Application No. 202392091 was accepted by Evraz. Pat. Dept. on 11/08/2023. (in Russian)].
Received 14.11.2023
Accepted 22.01.2024
About the Authors
Irina F. Krot, MD, PhD, Obstetrician-Gynecologist, St. Petersburg State Pediatric Medical University, Ministry of Health of Russia, +7(812)416-52-05, irinakrot@mail.ru, 194100, Russia, St. Petersburg, Litovskaya str., 2.Nikolai N. Ruhlyada, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology, St. Petersburg State Pediatric Medical University,
Ministry of Health of Russia, +7(812)295-17-42, nickolasr@mail.ru, 194100, Russia, St. Petersburg, Litovskaya str., 2.
Larisa A. Romanova, MD, PhD, Associate Professor, Associate Professor at the Department of Neonatology with courses of Neurology and Obstetrics and Gynecology,
St. Petersburg State Pediatric Medical University, Ministry of Health of Russia, +7(812)416-52-05, l_romanova2011@mail.ru, 194100, Russia, St. Petersburg, Litovskaya str., 2.
Vitaly A. Reznik, Dr. Med. Sci., Chief Physician of the Children’s Clinical Hospital, St. Petersburg State Pediatric Medical University, Ministry of Health of Russia,
+7(812)416-52-21, klinika.spb@gmail.com, 194100, Russia, St. Petersburg, Litovskaya str., 2.
Olga I. Sergienko, MD, Head of the Department of Pregnancy Pathology, St. Petersburg State Pediatric Medical University, Ministry of Health of Russia, +7(812)416-52-05, lelya.sergienko.80@mail.ru, 194100, Russia, St. Petersburg, Litovskaya str., 2.
Vano U. Chikhladze, MD, Obstetrician-Gynecologist, St. Petersburg State Pediatric Medical University, Ministry of Health of Russia, +7(812)416-52-05,
komrad.ushangi2010@yandex.ru, 194100, Russia, St. Petersburg, Litovskaya str., 2.
Ruzanna A. Vartanian, MD, Obstetrician-Gynecologist, St. Petersburg State Pediatric Medical University, Ministry of Health of Russia, +7(812)416-52-05,
ruzannavar@icloud.com, 194100, Russia, St. Petersburg, Litovskaya str., 2.