Ovarian-conserving surgery for large ovarian mature teratomas and cystadenomas: impact of surgical hemostasis techniques on ovarian reserve
Ibragimova U.D., Kozachenko I.F., Goryachev A.A., Adamyan L.V.
Benign ovarian tumors are common in women of reproductive age and often require ovarian-conserving surgery. The primary goal of such procedures is to remove the cystic lesion while maximizing the preservation of healthy ovarian tissue and reproductive potential. A critical aspect of the intervention is the choice of hemostasis method, as it can significantly affect ovarian reserve. Bipolar coagulation is associated with thermal damage to the ovarian stroma and microvasculature, potentially leading to a reduction in ovarian reserve, while the suture method offers mechanical vessel compression.
Objective: To evaluate the impact of hemostasis techniques on changes in ovarian reserve following laparoscopic cystectomy in reproductive-age patients with benign ovarian tumors.
Materials and methods: The study included 50 women aged 18–45 years with large (>8 cm) benign cystic ovarian tumors (mature teratomas and cystadenomas) who underwent surgery at the Gynecological Department of the V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology from 2022 to 2024. Patients were divided into two groups (n=25 each): following cystectomy, either suture hemostasis or bipolar coagulation was performed. Serum anti-Müllerian hormone (AMH) levels and antral follicle count (AFC) were assessed via transvaginal ultrasound before surgery and three months postoperatively; reproductive outcomes were also recorded.
Results: Baseline demographic and hormonal parameters were comparable between the groups. All surgeries were uneventful, with no statistically significant differences in operative duration or blood loss between the groups. Three months after cystectomy, both groups exhibited statistically significant reductions in AMH levels and AFC compared with baseline values; however, intergroup differences in the degree of reduction were not significant. Reproductive outcomes were also comparable between the groups.
Conclusion: Laparoscopic fertility-sparing cystectomy for benign ovarian tumors is associated with a reduction in ovarian reserve, the extent of which is influenced by the hemostasis technique employed. Both bipolar coagulation and suture-based hemostasis resulted in decreased AMH levels and AFC. Therefore, selecting a modern, effective hemostasis technique that minimizes damage to ovarian tissue is crucial for preserving reproductive potential.
Authors' contributions: Adamyan L.V., Kozachenko I.F. – conception and design of the study; Kozachenko I.F., Ibragimova U.D., Goryachev A.A. – data collection and processing; Ibragimova U.D., Kozachenko I.F., Goryachev A.A. – statistical analysis; Ibragimova U.D., Kozachenko I.F. – drafting of the manuscript; Adamyan L.V. – editing of the manuscript
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Ibragimova U.D., Kozachenko I.F., Goryachev A.A., Adamyan L.V. Ovarian-conserving surgery for large ovarian mature teratomas and cystadenomas: impact of surgical hemostasis techniques on ovarian reserve.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2026; (1): 70-77 (in Russian)
https://dx.doi.org/10.18565/aig.2025.290
Keywords
Benign ovarian tumors are highly prevalent in women of reproductive age. According to the literature, approximately 7% of women encounter benign ovarian neoplasms [1]. These tumors include mature cystic teratomas (dermoid cysts) and cystadenomas (serous or mucinous ovarian cystomas), which are frequently diagnosed in younger patients [2, 3]. Despite their benign nature, these tumors can cause complications. For example, dermoid cysts are associated with adnexal torsion in up to 3.5–11% of cases and carry a malignancy risk of approximately 1–2%, particularly in older women or when the cyst exceeds 10 cm in diameter [1]. Consequently, surgical treatment is necessary in such cases. The primary objective is to remove the tumor while preserving healthy ovarian tissue and the patient’s reproductive function, which underpins the strategy of organ-preserving surgery. The current gold standard is laparoscopic cystectomy with maximal preservation of the ovarian stroma [2]. In cases with a high risk of malignancy, more radical interventions, such as ovarian resection, may be considered; however, ovarian preservation is preferred in young women [2].
Surgical removal of an ovarian tumor can reduce the ovarian reserve. The reduction in the follicular pool is associated with inadvertent excision of healthy ovarian tissue along with the cyst capsule and impaired blood supply to the remaining stroma [1, 4]. Additionally, the choice of hemostatic technique plays a significant role in the extent of ovarian tissue injury. Traditionally, two hemostatic approaches have been used: ovarian suturing and bipolar electrocoagulation of the bleeding sites. Suturing provides mechanical compression of vessels without thermal injury, whereas coagulation controls bleeding through exposure to high temperatures. It is known that the use of electrosurgery may cause thermal damage to adjacent follicles and reduce ovarian reserve [5, 6]. Electrocoagulation is believed to destroy oocytes in the surrounding ovarian parenchyma, whereas tissue suturing is less traumatic for the follicular apparatus [5, 7]. Accordingly, recent literature has discussed which hemostatic method is more sparing for the ovary and better preserves the patient’s ovarian reserve [7, 8]. The surgical techniques employed and the method of hemostasis significantly influence the preservation of the ovarian reserve, as reflected in serum anti-Müllerian hormone (AMH) levels and antral follicle count (AFC). These findings underscore the need to optimize surgical techniques and select the most tissue-sparing hemostatic methods, particularly in patients planning to become pregnant [9].
Various markers are used for the objective assessment of ovarian reserve, including follicle-stimulating hormone and estradiol levels on cycle days 2–3, inhibin B, ultrasound-based antral follicle count (AFC), and others. Serum AMH levels and antral follicle count are considered the most sensitive indicators of POI [4]. AMH is produced by the granulosa cells of small growing follicles and reflects the size of the primordial follicle pool; its level does not depend on the phase of the menstrual cycle, making it suitable for longitudinal monitoring of the ovarian reserve [4]. A reduction in AMH levels after ovarian surgery is regarded as a sign of the loss of part of the follicular reserve [4].
This study aimed to evaluate the impact of different surgical hemostatic methods on the dynamics of ovarian reserve (changes in AMH and AFC levels) after laparoscopic cystectomy in reproductive-age patients with benign ovarian tumors (mature teratomas and cystadenomas).
Materials and methods
The study involved 50 patients of reproductive age (18–45 years) hospitalized in the Gynecological Department of V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, all diagnosed with “ovarian cystic formation” (cystadenoma and/or teratoma) between 2022 and 2024. All patients provided informed consent to participate in this study.
Each patient underwent a standard examination according to the accepted protocol, which included clinical and laboratory assessments, measurement of AMH levels in the blood serum, and ultrasound examination of the pelvic organs. Patients were divided into two groups based on the chosen method of surgical hemostasis: group 1 – suture hemostasis (n=25) and group 2 – bipolar coagulation hemostasis (n=25). This study specifically included patients with large benign ovarian tumors (≥ 8 cm).
Organ-sparing surgery was performed using laparoscopic access in all cases. The laparoscopic procedure followed standard technique. After creating a pneumoperitoneum in the abdominal cavity, a laparoscope (Karl Storz, Germany) and additional puncture trocars were sequentially inserted. Depending on the size of the cyst and anatomical features, 3 to 4 trocars were utilized: an optical trocar in the umbilical region and additional trocars in the iliac and suprapubic areas. The main stages of the operation included tumor enucleation, hemostasis, approximation of the ovarian margins, and removal of surgical material. An atraumatic clamp was used to fix a section of the tunica albuginea above the cyst with minimal thickness and vascularization, followed by a longitudinal incision of the membrane sufficient to initiate enucleation. The plane between the cyst wall and the adjacent ovarian tissue was identified, and the cyst was carefully peeled away using an atraumatic clamp. The macro specimen was removed using an endoscopic container through a trocar opening [10].
After cyst removal, two hemostasis methods were applied based on group assignment: suture hemostasis (n=25) or bipolar coagulation (n=25). In group 1, following cystectomy, the ovary was sutured with a continuous suture using absorbable polyglactin 2.0 material, achieving edge approximation and complete hemostasis through mechanical compression of the tissues. In Group 2, point bipolar coagulation was employed at a power of 36–40 watts under conditions of periodic irrigation of the surgical field, allowing for simultaneous cooling of the tissues and visualization of bleeding vessels. Coagulation was performed pointwise until the bleeding ceased completely. The tips of the bipolar forceps were used to grasp the bleeding areas of the ovarian stroma, followed by the activation of coagulation. The exposure was conducted in short bursts at a minimum power to minimize thermal tissue damage. The surgical material was sent for histological examination to the Anatomical Pathology Department of the I. Kulakov NMRC for OG&P, Ministry of Health of Russia. Cryosections (4–5 μm thick) were prepared from the specimens and stained with hematoxylin and eosin.
The criteria for evaluating the effectiveness of the surgical hemostasis methods included the dynamics of AMH levels in the blood serum, AFC as determined by ultrasound examination data before and three months after surgery, and indicators of reproductive outcomes.
Statistical analysis
Statistical analysis was performed using Microsoft Office Excel 2015 and MedCalc v.12 software. The distribution of continuous variables was tested for normality using the Kolmogorov–Smirnov test. Due to deviations from the normal distribution, all quantitative indicators are presented as medians and interquartile ranges (Me [Q1; Q3]). The nonparametric Mann–Whitney U test was used for group comparisons, while the Wilcoxon test was used for paired intra-group comparisons. In addition to testing the statistical significance of the differences (p-values), effect sizes (differences in medians and coefficient r) were calculated with 95% confidence intervals (CIs) for quantitative data. Categorical variables were described using counts and percentages. Pearson's chi-square test was used for group comparisons. Differences were considered statistically significant at p<0.05.
Results
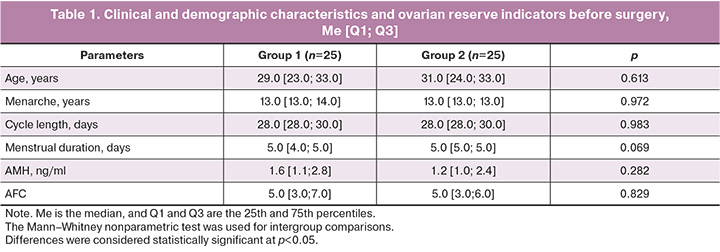
The patient groups were comparable in terms of age and baseline ovarian reserve parameters. The mean age in group 1 was 29.0 [23.0; 33.0] years, and in group 2, it was 31.0 [24.0; 33.0] years (p=0.613). The main complaints in both groups were lower abdominal pain, algomenorrhea, and failure to conceive. In group 1, the mean age at menarche was 13.0 [13.0; 14.0] years, the duration of the menstrual cycle was 28.0 [28.0; 30.0] days, and the duration of menstruation was 5.0 [4.0; 5.0] days. Heavy menstruation was noted in 11/25 (44%) patients, moderate menstruation in 14/25 (56%) patients, and no cases of scanty menstruation were recorded. Painful menstruation was observed in 9/25 (36%) of the women. In the medical history, 11/25 (44%) patients had timely deliveries, and 1/25 (4%) had a missed miscarriage. Combined pathology of the pelvic organs (adhesions, uterine fibroids, endometrial polyps, and genital malformations) was detected in 8/25 (32%) women. Surgical treatment for ovarian cysts had previously been performed in 4/25 (16%) patients.
In the second group, the age at menarche was 13.0 [13.0; 13.0] years, the duration of the menstrual cycle was 28.0 [28.0; 30.0] days, and the duration of menstruation was 5.0 [5.0; 5.0] days. Heavy menstruation was observed in 7/25 (28%) patients, moderate menstruation in 18/25 (72%) patients, and no cases of scanty menstruation were identified. Painful menstruation was noted in 4/25 (16%) women. In terms of reproductive history, 7/25 (28%) patients had timely deliveries, 2/25 (8%) had non-developing pregnancies, and 2/25 (8%) had ectopic pregnancies. Combined pathology of the pelvic organs was diagnosed in 9/25 (36%) women. Surgical treatment for ovarian cysts had previously been performed in 2/25 (8%) of the patients.
The mean baseline AMH level in group 1 was 1.5 [1.1; 2.4] ng/ml, and in group 2, it was 1.6 [1.1; 2.7] ng/ml; the differences were not statistically significant (p=0.357). Ultrasound examination of the pelvic organs revealed cystic formations (mature teratomas or cystadenomas) of varying sizes. AFC before surgical treatment in group 1 was 5.0 [3.0; 6.0], in group 2 – 5.0 [3.0; 7.0]; p=0.829. Thus, initially, the patients in both groups did not differ in terms of clinical and demographic characteristics and ovarian reserve indicators (Table 1).
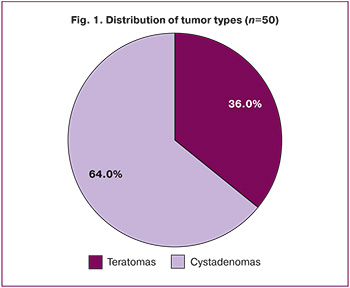
Histological examination revealed mature ovarian teratomas in 32/50 (64%) women and serous/mucinous ovarian cystadenomas in 18/50 (36%) – serous/mucinous ovarian cystadenomas (Fig. 1). In 48/50 (96%) patients, the formations were unilateral, whereas bilateral cysts were found in 2/50 (4%) cases. The sizes of the cystic formations ranged from 8.0 cm to 20.0 cm. The average size of tumors in the first group was 11.0 [9.0; 12.0] cm, and in the second group, it was 9.0 [8.5; 10.0] cm.
Surgical interventions were performed without intraoperative or postoperative complications in all the patients. The average duration of surgery in group 1 was 55.0 [50.0; 70.0] min, and in the second group, 50.0 [40.0; 65.0] min, depending on the size of the tumor and the presence of concomitant gynecological pathology; no statistically significant difference was noted between the groups (p=0.077). Intraoperative blood loss was minimal in both groups (p=1.0), and blood transfusion was not required. Blood loss in the first group averaged 50.0 [50.0; 50.0] ml, and in the second group, 50.0 [30.0; 50.0] ml. In no case was additional hemostasis required after the procedure.
At the time of the study, 28/50 (56%) patients were planning a pregnancy, including 13/25 (52%) in the first group and 15/25 (60%) in the second group. During the observation period, 7/25 (28%) patients in the first group and 10/25 (40%) in the second group became pregnant, of which 1/7 (14%) in the first group and 1/10 (10 %) in the second group. No statistically significant differences were observed between the groups (p>0.05). The timing of pregnancy varied from 3 to 9 months after the surgical treatment. No cases of spontaneous abortion or miscarriages were identified.
Three months after surgery, the dynamics of serum AMH levels and AFC were analyzed (Figs. 2, 3). The average AMH level in group 1 decreased to 1.0 [0.4; 1.5] ng/ml, and in group 2 to 1.2 [0.6; 1.7] ng/ml; intergroup differences remained statistically insignificant (p=0.180). AFC after surgical treatment was 2.0 [1.0; 4.0] in group 1 and 2.0 [1.0; 5.0] in group 2 (p=0.202).
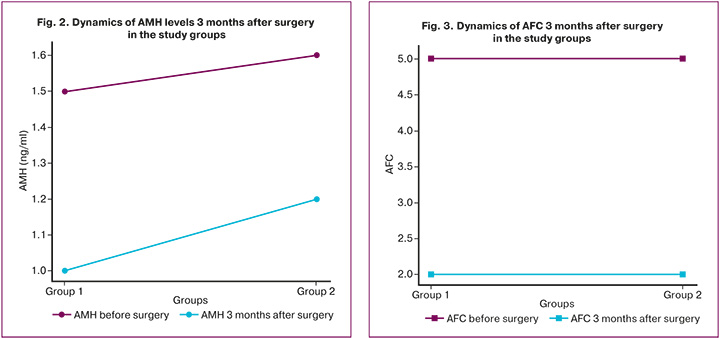
To assess the effect of the hemostasis method on the ovarian reserve, the difference between the postoperative and baseline values (Δ) for each parameter was analyzed (Table 2). In group 1, the average decrease in AMH was approximately 0.5 ng/ml, and in group 2, it was approximately 0.4 ng/ml; that is, the decrease in AMH was comparable, and the intergroup difference in changes was not statistically significant. Similarly, the median decrease in AFC in both groups was approximately three follicles, with no significant differences between the hemostasis methods. The effect size assessment showed that the difference in the median changes in AMH levels between the groups was approximately 0.1 ng/ml (group 2 − group 1; 95% CI: -0.4; 0.6), and the difference in the median changes in AFC was approximately 0.0 (95% CI: -1.5; 1.5), indicating no clinically significant intergroup differences.
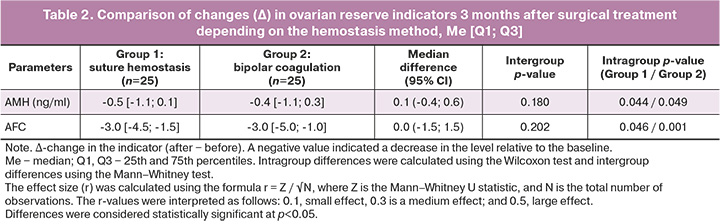
Thus, despite a statistically significant decrease in AMH and AFC levels compared to baseline values in each group, the nature and severity of these changes did not differ between patients who underwent suture hemostasis and those who underwent bipolar coagulation hemostasis.
Discussion
The findings of this study confirm that the choice of hemostatic technique, either suturing or bipolar coagulation, during ovarian-sparing surgery significantly impacts the preservation of the ovarian reserve. Regardless of the mechanism employed (mechanical, thermal, or laser energy; electrocoagulation; ultrasonic scalpel; or chemical adhesive compounds), most surgical hemostasis methods can injure ovarian tissue, leading to a reduction in the ovarian reserve among women of reproductive age [11]. The most commonly used hemostatic techniques following ovarian cystectomy are spot electrocoagulation of bleeding sites and suturing [12]. In bipolar coagulation, thermal energy induces focal necrosis of the ovarian stroma and damages the microvascular bed [12–14]. Thermal injury can extend several millimeters beyond the coagulation point, destroying primordial and preantral follicles that constitute the ovarian reserve [5]. Several studies have indicated that electrocoagulation may damage the primordial follicle pool due to thermal tissue necrosis and impaired microcirculation [6, 15, 16]. Suturing compresses vessels without thermal effects; however, some partial mechanical injury to the ovarian tissue may occur, which is more localized and primarily affects the capsule and stromal areas rather than the entire cortex of the ovary. Even with suture-based hemostasis, there remains a risk of local ischemia in the zone of suture tightening when excessive tension is applied [13]. Currently, no universal standard for hemostasis exists in ovarian surgery that ensures reliable control of bleeding while maximizing the preservation of the ovarian reserve [17]. The mere performance of a cystectomy can lead to a reduced ovarian reserve due to the loss of healthy tissue; the extent of these changes, reported in studies as 13–40%, is influenced by the specifics of the surgical technique, the hemostasis method used, and the morphological characteristics of the tissue [13]. A randomized study demonstrated that the use of a chemical hemostatic agent (oxidized cellulose) was associated with a smaller reduction in AMH levels, highlighting the potential of alternative hemostatic methods [13]. Contemporary reviews indicate that suturing ovarian tissue after cystectomy is a more conservative approach for preserving the ovarian reserve than electro-surgical hemostasis [7, 8].
The clinical relevance of these findings lies in their potential impact on fertility and reproductive prognosis; a substantial reduction in ovarian reserve may shorten the time available for women to achieve their reproductive goals [1]. A difference of 0.5–1.0 ng/mL in AMH levels one year after surgery, as shown in previous studies [18], may be clinically significant for patients, particularly those with a low baseline reserve or those planning delayed childbearing. Therefore, the selection of a tissue-sparing surgical technique is crucial in this case. International and national guidelines for managing patients with benign ovarian tumors emphasize the need to preserve as much healthy ovarian tissue as possible during surgery, particularly in young women [1].
Alternative hemostatic techniques are being developed to minimize this injury. One approach involves the use of modern hemostatic materials and adhesives. Randomized trials have indicated that hemostatic agents (e.g., oxidized cellulose and fibrin glue) can provide bleeding control comparable to coagulation while maximizing the preservation of the ovarian reserve [13, 19].
Thus, optimizing the management of benign ovarian lesions using modern, effective surgical hemostasis techniques that minimize damage to the ovarian tissue remains a pressing challenge in reproductive surgery.
Conclusion
Organ-sparing surgical treatment of benign ovarian tumors (mature teratomas and cystadenomas) is associated with a reduction in ovarian reserve, the extent of which is largely determined by the hemostatic method used during surgery. The present study demonstrated that hemostasis techniques applied after cyst removal led to a statistically significant reduction in AMH and AFC levels. An individualized approach that considers the patient’s reproductive plans is essential for successful treatment. The choice of hemostatic method should be regarded as a key factor in preserving a woman’s reproductive potential and preventing complications. Optimizing surgical techniques for managing benign ovarian tumors can substantially improve the likelihood of maintaining reproductive function. The implementation of modern and tissue-sparing hemostatic methods in clinical practice will enhance long-term treatment outcomes and help preserve ovarian hormonal function and fertility in reproductive-age patients post-surgery.
References
- Guillaume A., Pirrello O. Preservation of fertility in surgery of benign and borderline malignant ovarian tumors. J. Visc. Surg. 2018; 155 Suppl. 1: S17-S21. https://dx.doi.org/10.1016/j.jviscsurg.2018.04.001
- Cong L., Wang S., Yeung S.Y., Lee J.H.S., Chung J.P.W., Chan D.Y.L. Mature cystic teratoma: an integrated review. Int. J. Mol. Sci. 2023; 24(7): 6141. https://dx.doi.org/10.3390/ijms24076141
- Pekar-Zlotin M., Rabinovich I., Goldrat I., Vaknin Z., Gidoni Y., Zur-Naaman H. et al. Ovarian dermoid cysts associated with paraneoplastic syndrome N-methyl-D-aspartic acid receptor antibodies encephalitis. J. Minim. Invasive Gynecol. 2021; 28(6): 1190-3. https://dx.doi.org/10.1016/j.jmig.2020.09.018
- Pergialiotis V., Prodromidou A., Frountzas M., Bitos K., Perrea D., Doumouchtsis S.K. The effect of bipolar electrocoagulation during ovarian cystectomy on ovarian reserve: a systematic review. Am. J. Obstet. Gynecol. 2015; 213(5): 620-8. https://dx.doi.org/10.1016/j.ajog.2015.04.006
- Park E.Y., Hwang K.H., Kim J.H., Lee S.H., Park K.S., Choi S.J. et al. Epinephrine minimizes the use of bipolar coagulation and preserves ovarian reserve in laparoscopic ovarian cystectomy: a randomized controlled trial. Sci Rep. 2020; 10(1): 20911. https://dx.doi.org/10.1038/s41598-020-77781-w
- Chung J.P.W., Law T.S.M., Mak J.S.M., Sahota D.S., Li T.C. Ovarian reserve and recurrence 1 year post-operatively after using haemostatic sealant and bipolar diathermy for haemostasis during laparoscopic ovarian cystectomy. Reprod. Biomed. Online. 2021; 43(2): 310-8. https://dx.doi.org/10.1016/j.rbmo.2021.05.003
- Peters A., Rindos N.B., Lee T. Hemostasis during ovarian cystectomy: systematic review of the impact of suturing versus surgical energy on ovarian function. J. Minim. Invasive Gynecol. 2017; 24(2): 235-46. https://dx.doi.org/10.1016/j.jmig.2016.12.009
- Sun X., Liu D., Guo Z., He L., Wang S. The influence of ovarian cyst type and size on ovarian reserve markers: implications for fertility counseling and preservation strategy. Front. Endocrinol (Lausanne). 2025; 16: 1517789. https://dx.doi.org/10.3389/fendo.2025.1517789
- Филиппова Е.С., Козаченко И.Ф., Адамян Л.В., Дементьева В.О. Влияние хирургического лечения эндометриоидных кист яичников на состояние овариального резерва у женщин репродуктивного возраста. Проблемы репродукции. 2018; 24(4): 71-80. [Filippova E.S., Kozachenko I.Ph., Adamyan L.V., Dementyeva V.O. Influence of surgical treatment of ovarian endometriomas cysts on ovarian reserve in women of reproductive age. Russian Journal of Human Reproduction. 2018; 24(4): 71-80 (in Russian)]. https://dx.doi.org/10.17116/repro20182404171
- Ибрагимова У.Д., Козаченко И.Ф., Адамян Л.В. Овариальный резерв и методы хирургического гемостаза при доброкачественных опухолях яичников. Акушерство и гинекология. 2025; 8: 150-8. [Ibragimova U.D., Kozachenko I.F., Adamyan L.V. Ovarian reserve and surgical hemostasis methods for benign ovarian tumors. Obstetrics and Gynecology. 2025; (8): 150-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2025.175
- Венцковский Б.М., Жегулович В.Г., Жегулович Ю.В. Овариальный резерв при хирургии яичника. Гемостаз путем временной компрессии как альтернатива воздействия физических энергий и химических средств на яичник. Репродуктивное здоровье. Восточная Европа. 2019; 9(2): 120-6. [Ventskovsky B.M., Zhegulovich V.G., Zhegulovich Yu.V. Ovarian reserve in ovarian surgery. Hemostasis by temporary compression as an alternative to the effects of physical energies and chemicals on the ovary. Reproductive Health. Eastern Europe. 2019; 9(2): 120-6 (in Russian)].
- Lachert E. Fibrin glues – the current state of knowledge. J. Transfus. Med. 2021; 14(4): 214-24. https://dx.doi.org/10.5603/JTM.2021.0012
- Park S.J., Seol A., Lee N., Lee S., Kim H.S. A randomized controlled trial of ovarian reserve preservation and hemostasis during ovarian cystectomy. Sci. Rep. 2021; 11(1): 8495. https://dx.doi.org/10.1038/s41598-021-87965-7
- Пивазян Л.Г., Унанян А.Л., Пойманова О.Ф., Бондаренко Е.Н., Ищенко А.И. Эндометриома: овариальный резерв и тактика ведения. Проблемы репродукции. 2021; 27(5): 77-83. [Pivazyan L.G., Unanyan A.L., Poymanova O.F., Bondarenko E.N., Ishchenko A.I. Endometrioma: ovarian reserve and management. Russian Journal of Human Reproduction. 2021; 27(5): 77-83 (in Russian)]. https://dx.doi.org/10.17116/repro20212705177
- Lin Y.H., Hsia L.H., Huang Y.Y., Chang H.J., Lee T.H. Potential damage to ovarian reserve from laparoscopic electrocoagulation in endometriomas and benign ovarian cysts: a systematic review and meta-analysis. J. Assist. Reprod. Genet. 2024; 41(10): 2727-38. https://dx.doi.org/10.1007/s10815-024-03227-1
- Aradağ C., Demircan S., Turgut A., Çalışkan E. Effects of laparoscopic cystectomy on ovarian reserve in patients with endometrioma and dermoid cyst. Turk. J. Obstet. Gynecol. 2020; 17(1): 15-20. https://dx.doi.org/10.4274/tjod.galenos.2020.37605
- Соломатина А.А., Хамзин И.З., Тюменцева М.Ю., Чабиева Л.Б., Тумасян Е.А., Дулаева А.О. Органосберегающие операции у пациенток с доброкачественными образованиями яичников в аспекте сохранения репродуктивного потенциала. Лечебное дело. 2019; 3: 34-41. [Solomatina A.A., Khamzin I.Z., Tyumentseva M.Yu., Chabieva L.B., Tumasyan E.A., Dulaeva A.O. Organ-preserving surgery in patients with benign ovarian masses in terms of maintaining reproductive potential. Lechebnoe delo. 2019; 3: 34-41 (in Russian)]. https://dx.doi.org/10.24411/2071-5315-2019-12138
- Wang J., Wang Y.X., Wu H.T., Li X.M. Long-term effects of bipolar electrocoagulation and suture hemostasis on the ovarian reserve following endometriotic cystectomy: a meta-analysis. Arch. Gynecol. Obstet. 2025; 312(1): 149-58. https://dx.doi.org/10.1007/s00404-024-07926-z
- Кузьмина Н.С., Беженарь В.Ф., Калугина А.С. Опыт интраоперационного использования гемостатических матриц для сохранения овариального резерва у больных с эндометриомами. Проблемы репродукции. 2018; 24(2): 54-62. [Kuzmina N.S., Bezhenar' V.F., Kalugina A.S. Experience in intraoperative use of hemostatic matrices to preserve the ovarian reserve in patients with endometriomas. Russian Journal of Human Reproduction. 2018; 24(2): 54-62 (in Russian)]. https://dx.doi.org/10.17116/repro201824254-62
Received 15.10.2025
Accepted 03.12.2025
About the Authors
Ummusalimat D. Ibragimova, PhD student, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, amintaeva_umm@mail.ru, https://orcid.org/0009-0008-6984-7193Irena F. Kozachenko, Dr. Med. Sci., Leading Researcher, obstetrician-gynecologist, Gynecological Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, irenakozachenko@rambler.ru,
https://orcid.org/0000-0003-1822-9164
Alexander A. Goryachev, 6th year student, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117513, Russia, Moscow, Ostrovityanova str.,
1, build. 7, alexgoryachev2022@mail.ru, https://orcid.org/0009-0003-0221-3050
Leila V. Adamyan, Academician of the Russian Academy of Sciences, Dr. Med. Sci., Professor, Deputy Director for Research, Head of the Department of Operative Gynecology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4; Chief Specialist in Gynecology of the Ministry of Health of Russia; Head of the Department of Reproductive Medicine and Surgery of the Faculty of Postgraduate Education, Russian University of Medicine, 127473, Russia, Moscow, Delegatskaya str., 20-1, adamyanleila@gmail.com,
https://orcid.org/0000-0002-3253-4512
Corresponding author: Ummusalimat D. Ibragimova, amintaeva_umm@mail.ru