Применение вспомогательных репродуктивных технологий (ВРТ) сопряжено с развитием различных структурно-функциональных нарушений системы мать–плацента–плод. В 30–35% случаев происходит прерывание беременности вследствие фетоплацентарной недостаточности, задержки роста плода, невынашивания, преэклампсии. Вероятность отрицательных исходов ВРТ увеличивается с возрастом и при отягощенном анамнезе [1], включающем ожирение, уровень которого в мире постоянно растет [2].
Влияние ожирения на функцию репродуктивной системы женщин и пути устранения последствий
Ожирение – частая причина ановуляторного бесплодия/невынашивания беременности; формируется на фоне патологической нейроэндокринной регуляции гомеостаза, вызванной стрессом, нарушением адаптационных резервов, инфекционными и токсическими факторами, наличием заболеваний. Риск ожирения повышен в периоды детства, полового созревания, беременности и климакса [3]. При высоком индексе массы тела (ИМТ) увеличивается время с момента планирования беременности до зачатия в связи с развитием субфертильности, которая может сочетаться с регулярным менструальным циклом и отсутствием овуляторной дисфункции. Отмечена линейность снижения фертильности при ИМТ>29 кг/м2 [2]. Среди женщин с синдромом поликистозных яичников (СПЯ) 75% страдают ожирением [4]. На его фоне возникают овуляторная дисфункция, гиперандрогения, увеличенный объем яичников [3], психические расстройства (нарушение питания, булимия, депрессия) [5, 6]. Ожирение – результат нарушения функции гипоталамо-гипофизарно-яичниковой оси (рисунок).

Сравнительный анализ гормонального статуса у женщин с нормальным и высоким ИМТ показал противоречивые результаты в отношении уровней лютеинизирующего гормона, фолликулостимулирующего гормона и эстрадиола. Наряду с их превышением [7] отмечено отсутствие различий по данным маркерам. Однако установлено явное превышение уровня тестостерона и уменьшение уровня антимюллерова гормона в комплексе со снижением количества антральных фолликулов и объема яичников по мере увеличения степени ожирения. Гормональные показатели в основном остаются в пределах референсных значений, но свидетельствуют о тенденции снижения овариального резерва [8].
Специальные программы по нормализации веса приводят к уменьшению уровней гиперандрогении, резистентности к инсулину и атерогенных фракций липидов, а также к регулярности менструального цикла, полноценным овуляциям и улучшению психологического статуса [6, 9–11]. Увеличение потребления белка, фруктов, овощей, цельных зерен и молочных продуктов с низким содержанием жира/холестерина приводят к потере веса у женщин с СПЯ без стандартной низкокалорийной диеты. Улучшаются показатели глобулина, связывающего половые гормоны, и антимюллерова гормона [10]. Признано, что сбалансированная средиземноморская диета снижает риск гестационного диабета, так как нормализует уровни глюкозы/липидов/липопротеинов [12].
Влияние высокого ИМТ матери на здоровье плода недостаточно изучено. Известно, что гиперлипидемия, гипергликемия и гиперинсулинемия приводят к нарушениям развития и функции плаценты, накоплению активных форм кислорода в связи с дефицитом антиоксидантов и к снижению толерантности к глюкозе. Повышаются риски развития у плода кардиометаболического синдрома [13] и сахарного диабета [14]. При гиперкалорийном жировом питании женщины возникает нарушение функции инфундибулярного ядра гипоталамуса у плода и развиваются резистентность к лептину, подавляющему ощущение голода, макросомия, предрасположенность к ожирению [15]. Возникает также дефицит адипонектина [16], в результате снижаются чувствительность к инсулину и сосудорасширяющая реакция на ацетилхолин, появляется предрасположенность к сердечно-сосудистым заболеваниям [17].
Обнаружена обратная связь между ИМТ и содержанием фолиевой кислоты [18], дефицит которой приводит к дефектам нервной трубки [2]. Отмечен позитивный эффект комбинированных оральных контрацептивов с дроспиреноном и фолатами в подержании уровня витамина [19]. Ожирение относится к эндокринопатиям и вызывает нарушения, сходные с таковыми для невынашивания беременности [9, 20]. Недостаточность лютеиновой фазы при высоком ИМТ возникает в связи с дефицитом прогестерона [9, 21], что приводит к нарушению инвазии трофобласта [2] и возрастанию риска развития рака эндометрия [22–25]. Поэтому необходима нормализация веса, в том числе посредством бариатрической хирургии [26]. Зависимость уровня прогестерона и риска рака эндометрия формируется на этапе менархе, и важен контроль ИМТ девочки-подростка. Чрезмерное накопление жировой ткани в детстве/пубертатном периоде приводит к развитию выраженного морбидного (ИМТ>40 кг/м2) ожирения в репродуктивном возрасте с отложением жира во внутренних органах (висцеральный тип) и к гипоталамическому синдрому. Раннее ожирение встречается у 40–50% женщин с бесплодием. Средняя длительность менструального цикла у них составляет 35,5 дня против 28,1 дня для группы репродуктивно-здоровых. Отмечено увеличение объемов яичников в 1,4–1,5 раза [3].
Эффективность ВРТ при избыточном ИМТ
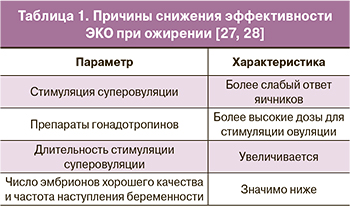 Установлено, что эффективность ВРТ у женщин с ИМТ ≥30,8 кг/м2 значимо снижена (табл. 1), и оптимальной тактикой лечения является предварительная нормализация веса [27]. Необходимо применение более высоких доз препаратов гонадотропинов [28].
Установлено, что эффективность ВРТ у женщин с ИМТ ≥30,8 кг/м2 значимо снижена (табл. 1), и оптимальной тактикой лечения является предварительная нормализация веса [27]. Необходимо применение более высоких доз препаратов гонадотропинов [28].
Повышенная потребность в дозе гонадотропина может быть связана с изменением фармакодинамических характеристик препаратов, вводимых подкожно, у тучных женщин с увеличенной толщиной жировой прослойки. У таких пациентов зарегистрированы изменения в абсорбции, метаболизме, биодоступности и клиренсе препаратов [7].
При использовании пероральной формы экзогенного прогестерона действует только 10% вещества, поэтому при проведении ВРТ процент беременностей выше в случае использования внутримышечного или вагинального препаратов [2, 29]. Последний в микронизированной форме обладает максимальным эффектом в нормализации гормонального состояния при ожирении до и во время беременности. Его клинические эффекты (прогестагенный, антиэстрогенный, антиальдостероновый, антиандрогенный, токолитический, нейротропный), а также поддержка лютеиновой фазы и при угрозе выкидыша более выражены, чем для дигидрогестерона [2, 30].
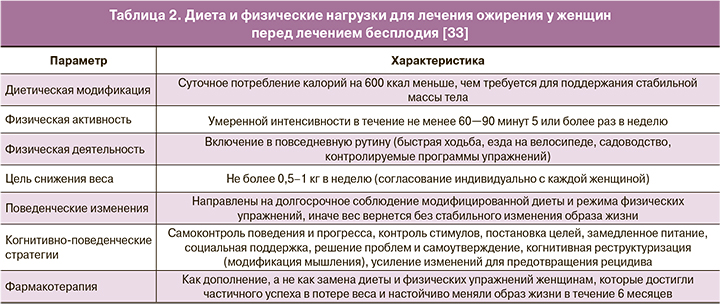
Результаты многих исследований показывают, что потеря веса должна проводиться у женщин с избыточным весом и ожирением до начала лечения бесплодия [31]. Рассматриваются варианты применения фармакологического подхода к лечению ожирения. Хорошие результаты показал орлистат (антиабсорбционный препарат) – ингибитор панкреатической липазы, приводящий к снижению всасывания жирных кислот из кишечника примерно на 30%. Его прием дополняют экзогенными источниками жирорастворимых витаминов (в основном D) с соблюдением паузы 2 ч до/после приема орлистата. Противопоказаниями к его применению являются синдромы хронической мальабсорбции и холестаза. Метформин (инсулин-сенсибилизирующий агент), подавляющий выработку глюкозы в печени, повышает чувствительность периферических тканей к инсулину, что приводит к снижению уровней циркулирующего инсулина и андрогенов и сопровождается уменьшением массы тела/висцерального жира. Хороший результат применения метформина достигается при его сочетании с низкокалорийной диетой [32]. В Великобритании метформин широко используется в лечении синдрома поликистозных яичников (СПЯ), но не лицензирован как препарат для лечения ожирения. Сибутрамин и римонабант (блокатор аппетита и антагонист каннабиноидных рецепторов соответственно) были изъяты с рынка в Великобритании вследствие опасений побочных эффектов на сердечно-сосудистую систему (гипертония, сердцебиение) и нервно-психиатрических реакций (депрессия, суицидальные риски). Прием орлистата на ранних сроках гестации позиционируется как безопасный, однако все же лучше провести нормализацию веса до беременности. При сравнении метформина и орлистата выявлено, что они показывают примерно сходные (без достоверных отличий) результаты при лечении пациенток с ожирением и СПЯ: снижение ИМТ, уровня андрогенов [33].
Существуют данные успешного применения ЭКО после бариатрической хирургии. Через 1–5 лет после применения метода у женщин отмечались доношенные роды без осложнений; при этом данный метод нормализации веса позволяет снизить риск гестационного диабета, преэклампсии, гипертонических расстройств и макросомии [32].
Выбор терапии для нормализации веса зависит от сопутствующих патологий (сахарный диабет, артериальная гипертензия, дислипидемия, сердечно-сосудистые заболевания и синдром обструктивного апноэ сна), с учетом которых, а также по окружности талии (<80, 80–88 или >88 см) необходимо определять уровень риска [33]. Количества рандомизированных исследований, направленных на улучшение результатов лечения ожирения у женщин, получающих лечение бесплодия в целом и ВРТ в частности, недостаточно. Для достижения стабильного результата необходим междисциплинарный подход (табл. 2).
Поздний репродуктивный возраст и ВРТ
Данные о взаимосвязи ожирения и позднего репродуктивного возраста противоречивы. Некоторые авторы показали, что ИМТ оказывает минимальное влияние на фертильность по сравнению с возрастом у женщин в возрасте 35 лет и более [7]. Другие утверждают, что ожирение оказывает значительное неблагоприятное влияние на исход ВРТ, независимо от возраста и других факторов, а отрицательный эффект, по-видимому, более выражен у молодых женщин [33]. Поздний репродуктивный возраст (после 35 лет) отличается снижением вероятности (лишь 5%) зачатия и риском (34–52%) несохранения беременности [34].
Причины развития бесплодия в позднем репродуктивном возрасте [35]: более высокая соматическая и гинекологическая заболеваемость (отягощение анамнеза); повышение вероятности наличия хромосомных (анеуплоидии, в частности) аномалий ооцитов; снижение овариального резерва и частоты оплодотворения. В результате действия вышеуказанных факторов снижается вероятность наступления спонтанной беременности, а эффективность ВРТ не превышает 10–15% с ежегодным снижением показателя на 4,7%. По сравнению с группой 35 лет и моложе успешность лечения и перспективы живорождения ниже в 2–2,2 раза [34]. Число женщин позднего репродуктивного возраста, обращающихся в центры ЭКО, постоянно растет. Механизмы, приводящие к бесплодию в позднем репродуктивном возрасте, включают яичниковое звено, высшие регулирующие центры репродуктивной системы и периферические эндокринные железы [35]. Предположительно, снижение количества фолликулов вызывает ухудшение их качества. Появление аномальной васкуляризации в яичниках и уменьшение перфузии в микроокружении созревающих ооцитов приводят к гипоксии и окислительному стрессу. Известно также, что у женщины с возрастом сокращается менструальный цикл в связи с уменьшением фолликулярной фазы и более ранней овуляцией. Причина заключается в уменьшении количества антральных фолликулов, продуцирующих ингибин В, снижающий базальный уровень фолликулостимулирующего гормона, повышение которого вызывает ускорение селекции доминантного фолликула [36]. Технология ЭКО считается наиболее экономичной и эффективной для лечения бесплодия. Однако в позднем репродуктивном возрасте даже при получении высококачественных эмбрионов повышается вероятность неудач вследствие различных нарушений при инвазии бластоцисты в ткань эндометрия, включающих совокупность факторов развития ооцитов и эмбрионов, а также секреторной трансформации эндометрия [35]. Единственным решением является комплексная подготовка перед ВРТ для адекватной оценки функционального состояния репродуктивной системы и соблюдение здорового образа жизни. Например, мелатонин секретируется в темное время суток эпифизом, а также вырабатывается в яичниках и в плаценте [37, 38]. Гормон противодействует окислительному стрессу и регулирует клеточный метаболизм, поэтому рассматривается как компонент для лечения бесплодия и улучшения результатов ВРТ [39]. С возрастом продукция данного гормона снижается. Особенно повышен риск развития ановуляции у женщин, не спящих ночью [40]. Ряд специалистов утверждают, что мелатонин улучшает качество яйцеклетки и эмбриона [35].
Заключение
Высокий ИМТ повышает риск репродуктивных нарушений для матери и плода: СПЯ, гестационного диабета, онкологических исходов. Для повышения эффективности ВРТ необходимы внедрение в гинекологические алгоритмы программ снижения веса и консультация диетологов. После решения проблемы лишнего веса и диагностики наличия гинекологических/системных патологий требуется контроль пищевого поведения до и в течение беременности с подключением обучающих технологий и психологической сферы. В позднем репродуктивном возрасте необходимы тщательный сбор данных анамнеза и лечение заболеваний. Требуется изучение перспектив коррекции гормонального фона и/или отдельных компонентов эндокринной системы. Вмешательство в образ жизни женщины для коррекции ее ожирения необходимо, но существует пробел в доказательствах, полученных в результате рандомизированных контролируемых исследований. Отсутствуют также исследования, касающиеся применения препаратов против ожирения в условиях ЭКО в сравнении с плацебо.