Врастание плаценты является одной из наиболее тяжелых аномалий прикрепления, обусловленной высоким риском массивного кровотечения. По данным ВО, за последние годы кровотечение занимает одну из лидирующих позиций в структуре причин материнской смертности, варьируя от 19,9 до 36,2% [1]. По данным Минздрава РФ за 2016 г., кровотечения занимают 3-е место (12,8%) среди прочих акушерских факторов, причем непосредственный вклад врастания плаценты в долю материнской смертности составляет 7% [2].
Чрезвычайно важным является антенатальное определение факта врастания плаценты, а также степени врастания. При отсутствии должной диагностики данной патологии до родоразрешения врач неизбежно сталкивается с очень сложной задачей принятия решения об оперативной тактике, а также с неизбежной массивной кровопотерей.
Можно выделить три основных подхода, реализуемых при родоразрешении данных пациенток: выполнение гистерэктомии (одномоментной [3, 4] или отсроченной [5]), проведение органосохраняющей операции, а также консервативное ведение пациенток на фоне цитостатиков с оставлением плаценты in situ [6–8]. Само по себе удаление матки травматично, способствует увеличению кровопотери и дискредитирует функцию репродуктивной системы и тазового дна, что связано с локальным изменением кровотока, иннервации и лимфодренажа, приводящим к развитию полисистемных синдромов [9]. Тем не менее схоластичность сознания или отсутствие соответствующей материально-технической базы, а в ряде случаев клиническая ситуация не оставляют выбора в пользу органосберегающего родоразрешения [10]. При этом общий объем кровопотери при гистерэктомии по поводу врастания плаценты варьирует в широком диапазоне от 2000 мл до 7800 мл, в 90% случаев превышая 3000 мл [11–13].
Клиническое наблюдение
Беременная Г., 40 лет, госпитализирована 24.10.2018 г. в центральную районную больницу по месту жительства в сроке 31 неделя беременности, с жалобами на периодические тянущие боли внизу живота.
Из анамнеза: замужем, работает ночным свиноводом. Вредные привычки – курение с 18 лет. Рост 162 см, вес 63,5 кг.
Сопутствующие и перенесенные заболевания: хронический пиелонефрит, латентное течение, блокада ножки пучка Гиса.
Менархе с 12 лет, менструации регулярные. Данная беременность девятая, на учете в женской консультации с 16 недель. Первая беременность в 1996 г. закончилась медицинским абортом в сроке до 12 недель, без осложнений. Далее в 1997 г. срочные самопроизвольные роды, девочкой 3500 г, осложнились кровотечением в раннем послеродовом периоде с проведением гемотрансфузии. В 1998 г. неразвивающаяся беременность в сроке 8 недель с последующим abrasion cavi uteri. В 1999 г. – медицинский аборт в сроке до 12 недель, без осложнений. Пятая беременность в 2002 г. – роды срочные, самопроизвольные, девочка 3250 г, без осложнений. В 2007 г. преждевременные роды путем операции кесарева сечения (КС), причину не знает, девочка – 2150 г, послеоперационный период протекал без осложнений. В 2008 г. – самопроизвольный выкидыш в сроке 7 недель беременности, в 2009 г. – медицинский аборт в 8 недель, без осложнений.
При прохождении ультразвукового скрининга в перинатальном центре ГБУЗ «Самарская областная клиническая больница им. В.Д. Середавина» (СОКБ) в сроке беременности 19 недель 4 дня выявлено центральное предлежание плаценты.
По данным УЗИ, в 30 недель беременности выявлено: «Беременность 30 недель 6 дней. Неустойчивое положение плода. Центральное предлежание плаценты. Выраженное многоводие», в связи с чем женщине рекомендовано стационарное лечение в перинатальном центре СОКБ, от которого она категорически отказалась. Данные ультразвуковой допплерографии (УЗДГ) в данном сроке – без нарушений.
При поступлении в центральную районную больницу предварительный диагноз: «Беременность IX, 31 неделя. Угрожаемые преждевременные роды. Полное предлежание плаценты. Рубец на матке после операции КС в 2007 г. Многоводие. Вызванные беременностью отеки с незначительной протеинурией. Хроническая плацентарная недостаточность. Холестатический гепатоз. Хронический пиелонефрит, латентное течение». Начата профилактика РДС плода на фоне токолитической терапии.
Через 2 ч от момента поступления, в 11.45, у беременной на фоне спокойствия возникло обильное кровотечение из половых путей. Выставляется диагноз: «Беременность IX, 31 неделя. Полное предлежание плаценты. Кровотечение. Рубец на матке после операции КС».
В экстренном порядке в 12.05 24.10.2018 г. начата операция КС в нижнем маточном сегменте. Извлечен живой недоношенный мальчик 1930 г, 47 см, оценен по шкале Апгар 5 баллов на 1 минуте, через 5 минут – 6 баллов.
Одновременно вызваны бригада отделения оказания экстренной и плановой консультативной помощи перинатального центра СОКБ (САС) и детская неонатологическая бригада.
Интраоперационно обнаружено: плацента расположена по передней стенке матки, полностью перекрывает внутренний зев. Признаков отделения плаценты нет, диагностировано врастание плаценты, кровотечение.
Врачами центральной районной больницы принято решение расширить объем операции до ампутации матки. Кровопотеря на данном этапе составила 1800 мл. Уровень гемоглобина – 59 г/л. На этапе ЦРБ трансфузия эритроцитарной взвеси в количестве 889 мл и плазмы 2100 мл.
24.10.2018 г. в 13.00 вызвана бригада САС: операционная рана открыта. Состояние после ампутации матки без придатков. При оценке культи шейки матки гемостаз неполный, кровотечение продолжается. Принято решение расширить объем операции до экстирпации культи шейки матки с трубами с предварительной перевязкой внутренних подвздошных артерий. Дренирование брюшной полости.
Гемостаз достигнут полный. Гемодинамика стабильная. Кровопотеря 1200 мл. Таким образом, общая кровопотеря составила 3000 мл (табл. 1).

Ввиду нетранспортабельности по тяжести состояния решено оставить пациентку на первом уровне с проведением дистанционного наблюдения. Лечение согласовано. Даны рекомендации о назначении НМГ.
Ребенок через сутки переведен в детскую областную клиническую больницу в отделение реанимации.
Данные гистологического исследования. Матка: гравидарный эндометрий и плацентарная площадка с резко выраженными дистрофическими изменениями, обширными очагами некроза, в одном из участков отмечается врастание промежуточно дифференцированных ворсин хориона в толщу эндометрия, рассеянная очаговая и лимфоцитарная инфильтрация, кровоизлияния из разрушенных эритроцитов, отек. Тромбоз отдельных сосудов.
Далее 25.10.2018 в 11.10 родильница доставлена бригадой САС в перинатальный центр СОКБ, в отделение анестезиологии, реанимации и интенсивной терапии, с диагнозом: «1-е сутки после IV преждевременных родов на 31 неделе беременности. Полное предлежание плаценты с врастанием. Кровотечение. Геморрагический шок I ст. ДВС-синдром. Рубец на матке после операции КС в 2007 г. Тяжелая постгеморрагическая анемия. Гистопатическая матка.
24.10.2018. Лапаротомия. КС в нижнем сегменте матки. Ампутация матки без придатков.
24.10.2018. Экстирпация культи шейки матки с маточными трубами. Перевязка внутренних подвздошных артерий. Дренирование брюшной полости».
Осматривается ех consilium врачами перинатального центра. При поступлении жалобы на общую слабость. Состояние средней степени тяжести. Отмечается бледность кожных покровов. Живот мягкий, умеренно болезненный в области оперативного вмешательства. По дренажам – умеренное сукровичное отделяемое. Перистальтика активная. Диурез достаточный. Моча светлая, прозрачная. Решено продолжить лечение и дальнейшее обследование. Получает лечение: антикоагулянтная (гепарин 5000 ЕД п/к, 3 раза в день), антибактериальная (цефтриаксон) и инфузионная терапия (солевой сбалансированный раствор).
25.10.2018 в 13.25 выполнено УЗИ органов брюшной полости и малого таза. Обнаружено: гепатомегалия. Культя влагалища без особенностей. В общей подвздошной вене тромб толщиной 6,5 мм, длиной 21,5 мм. Рекомендовано цветовое допплеровское картирование (ЦДК) вен нижних конечностей, консультация сосудистого хирурга.
25.10.2018 в 16.00 пациентка отмечает нарастание отеков нижних конечностей, осмотрена ангиохирургом, рекомендовано ЦДК вен нижних конечностей.
ЦДК вен нижних конечностей: Признаки тромбоза нижней полой вены с флотацией верхушки тромба, тромба общей подвздошной вены справа. Учитывая вышеизложенные данные, пациентке показано оперативное лечение по жизненным показаниям в объеме установки противоэмболического кава-фильтра.
25.10.2018 в 17.30 выполнена илеокаваграфия. Имплантация противоэмболического кава-фильтра в нижнюю полую вену. В ходе операции обнаружено: проходимость подвздошных вен сохранена, признаков тромбоза нет, в просвете нижней полой вены дефект контрастирования линейной формы, не фиксированный к стенке сосуда, с основанием в области правой почечной вены протяженностью до 9 см. Выполнена имплантация противоэмболического кава-фильтра Cordis в супраренальный отдел нижней полой вены, выше верхушки тромба.
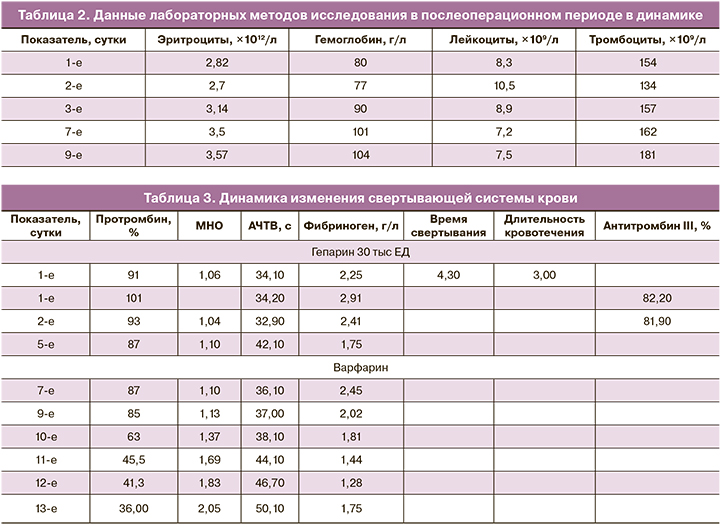
В послеоперационном периоде получала гепарин 30 000 ЕД в течение 5 суток с последующим переходом на варфарин под контролем МНО. После операции отмечается положительная динамика.
На 7-е сутки в удовлетворительном состоянии переводится из отделения реанимации в послеродовое отделение, где продолжена комплексная терапия (табл. 2–3).
При исследовании: волчаночный антикоагулянт отрицательный.
На 14-е сутки родильница выписана домой в удовлетворительном состоянии под наблюдение врача женской консультации, с необходимыми рекомендациями.
Ребенок на 2-е сутки после рождения был переведен в реанимацию детской областной больницы ГБУЗ «СОКБ им. В.Д. Середавина», после стабилизации состояния переведен на второй этап выхаживания. Через 3 недели выписан домой в удовлетворительном состоянии.
Описанный клинический случай может быть расценен как «near-miss», причем как в связи с кровотечением из-за врастания плаценты, так и в связи с тромбозом нижней полой вены и высоким риском тромбоэмболии легочной артерии (ТЭЛА).
Частота врастания плаценты увеличивается в геометрической прогрессии, и если в 1960 г. составляла 1 случай на 30 000 родов, то в настоящее время в больших центрах – 1 случай на 350 родов. В НМИЦ АГиП им. В.И. Кулакова за 2018 г. из 8500 родов прошло 60 случаев врастания плаценты (1 случай на 140 родов). Необходимы мультидисциплинарная команда, грамотная диагностика, а также достаточно простая хирургическая операция для снижения массивного кровотечения. В мире существует несколько методик оперативной тактики при врастании плаценты [14]. В настоящее время в Российской Федерации внедрены различные методики органосохраняющих операций, не требующих дорогостоящего оборудования (рентгеноперационная, баллонирование магистральных сосудов), наличия сосудистых хирургов и характеризующихся минимальной кровопотерей (до 1500 мл).
Операция в представленном случае выполнялась в ЦРБ, диагноз врастания плаценты не был выставлен антенатально, операция была экстренной в связи с возникшим кровотечением на 31-й неделе беременности. Все эти факторы представляли максимальный риск массивного кровотечения, кровопотеря в 3000 мл представляется невысокой в данной клинической ситуации, однако не было достигнуто надежного хирургического гемостаза, что потребовало вмешательства специалистов из перинатального центра и перевода пациентки в перинатальный центр для дальнейшего наблюдения.
Кровотечение и тромбоз являются разнонаправленными патофизиологическими процессами системы гемостаза, однако они всегда идут «рука об руку» [15]. И если такие факторы риска тромбоза, как венозные тромбоэмболические осложнения (ВТЭО) в анамнезе, преэклампсия, ожирение, тромбофилии, экстренное КС и др., в основном учитываются врачами, и вовремя назначается профилактика НМГ, то ситуация после возникшего массивного кровотечения с применением гемотрансфузии не всегда оценивается как очень высокий риск тромбоза, помимо этого, имеется боязнь назначения НМГ после массивного кровотечения, сомнения в надежности хирургического гемостаза, которые приводят к отсрочке назначения антикоагулянтной терапии или назначению субоптимальных доз НМГ.
Конечно, ВТЭО продолжают оставаться одной из ведущих причин материнской заболеваемости и смертности во всем мире. Следует отметить, что приблизительно 50% связанных с беременностью ТЭЛА и более 30% связанных с беременностью ВТЭО происходят именно после родов [16]. Повышенный риск ВТЭО, ассоциированных с беременностью, сохраняется в течение первых 3–6 недель послеродового периода [17, 18].
Заключение
Клиническое наблюдение демонстрирует благоприятный исход как для матери, так и для новорожденного, несмотря на ряд усложняющих факторов, таких как отсутствие антенатальной диагностики врастания плаценты, экстренное родоразрешение в связи с кровотечением, отсутствие в бригаде сосудистого хирурга, несколько запоздалое назначение антикоагулянтной терапии.
Несмотря на данные факторы, кровопотеря в данной ситуации была в пределах «нормы компенсированной патологии», снижение гемоглобина было некритичным, вовремя поставленный диагноз тромбоза нижней полой вены позволил оперативно произвести имплантацию кава-фильтра и избежать возможной тромбоэмболии. Вероятно, в данном случае необходимо было более раннее назначение антикоагулянтной терапии, и препаратом выбора должен был быть НМГ, а не НФГ.
Следует особо подчеркнуть, что беременные с предлежанием плаценты с 26-й недели беременности не должны находиться в учреждениях первого уровня оказания медицинской помощи.
Данное клиническое наблюдение демонстрирует важность определения оптимальной тактики при врастании плаценты и необходимости профилактики тромбоэмболических осложнений после массивного кровотечения.



