Антифосфолипидные антитела (аФЛ) представляют большую гетерогенную группу аутоантител, мишенями которых являются отрицательно заряженные и нейтральные фосфолипиды, фосфолипидсвязывающие протеины плазмы и их комплексы с фосфолипидами, факторы свертывания крови и компоненты комплемента [1]. Антитела классов M и G к кардиолипину (КЛ), β2-гликопротеину-I (β2-ГП-I) и волчаночный антикоагулянт (ВА), ассоциирующиеся с сосудистым тромбозом и акушерскими осложнениями, включая ранний привычный выкидыш (ПВ) до 10-й недели гестации, относятся к классификационным критериям антифосфолипидного синдрома (АФС), принятым в настоящее время [2]. Акушерский и сосудистый АФС признаются отдельными формами синдрома [3, 4]. Тромбоз и самопроизвольный выкидыш развиваются одновременно только в 2,5–5% случаев беременностей на фоне АФС. Так как тромботическими событиями, опосредованными аФЛ, не могут объясняться все акушерские проявления АФС, в качестве дополнительных патогенетических механизмов акушерского АФС рассматриваются воспаление плаценты, активация системы комплемента и прямое воздействие аФЛ на формирование и функционирование плаценты [4, 5].
аФЛ имеют диагностическое, прогностическое и патогенетическое значение как для сосудистого, так и для акушерского АФС [1, 4, 5, 6]. Антигенная и эпитопная специфичность аФЛ, их изотипы, титры, авидность и подклассы IgG, наличие одинарной или множественной позитивности на аФЛ определяют степень риска тромботических и акушерских проявлений [7, 8]. При наличии ВА или одновременном присутствии антител к КЛ и β2-ГП-I и ВА, то есть тройной позитивности, отмечается высокий риск потери беременности и тромбоза [6]. Однако у пациентов с симптомами акушерского и тромботического АФС также описан серонегативный вариант синдрома, при котором с использованием рутинных анализов не выявляются критериальные аФЛ [9]. При исследовании антител другой специфичности, таких как антитела к фосфатидилэтаноламину (ФЭ) и аннексину A5 (Ан A5), были получены противоречивые результаты, возможно, из-за малых объемов клинических данных. Однако некоторыми исследователями показана ассоциация IgM-антител к ФЭ и IgG-антител к Ан A5 с ранним ПВ [6].
Недавно у серонегативных женщин с клиническими проявлениями акушерского АФС были выявлены антитела к Ан A5, ФЭ и к комплексу фосфатидилсерин/протромбин (ФС/ПТ) и показана эффективность проведения терапии АФС для снижения частоты потери беременности [10]. Данные систематического обзора продемонстрировали высокую распространенность некритериальных аФЛ разной специфичности, в том числе антител к домену 1 аβ2-ГП-I у пациентов с АФС, по сравнению с контролем [11]. В настоящее время диагностика АФС не ограничивается определением только критериальных антител, так как определение спектра аФЛ повышает эффективность диагностики АФС у серонегативных пациентов. В качестве перспективных диагностических маркеров АФС рассматриваются IgA-антитела к КЛ и β2-ГП-I, антитела к домену I β2-ГП-I, ФЭ, Ан A5, ФС, ПТ и комплексу ФС/ПТ [12].
В связи с вышеизложенным, цель настоящего исследования – изучить спектр, иммунохимические свойства и диагностическое значение аФЛ у женщин с ранним ПВ.
Материалы и методы
Исследуемую группу (группа 1) составили небеременные женщины, проходившие в НМИЦ АГП им. академика В.И. Кулакова лабораторно-инструментальное обследование и лечение по поводу раннего ПВ неясного генеза, со средним возрастом 30,5 (5,0) года и средним числом потерь беременности 2,4 (1,5) случая. В анамнезе у женщин часто наблюдались инфекционно-воспалительные гинекологические заболевания, такие как хронический сальпингоофорит (14 (15,4%)), наружный генитальный эндометриоз (12 (13,2%)), цервицит (6 (6,6%)), инфекции, передаваемые половым путем (34 (37,4%)). Среди сопутствующих соматических заболеваний у 19 (20,9%) женщин отмечались аллергические заболевания, у 11 (12,1%) – хронический тонзиллит, у 13 (14,3%) – хронические заболевания органов мочевыделительной системы, у 7 (7,7%) – хронические заболевания органов пищеварительной системы. Три пациентки имели в прошлом тромбоз глубоких вен нижних конечностей. Критериями исключения служили: наличие пороков развития половых органов, носительство хромосомных перестроек, генетические аномалии у плода, беременности после программ вспомогательных репродуктивных технологий, тяжелая соматическая и аутоиммунная патология, острые инфекционно-воспалительные заболевания.
Группа сравнения (группа 2) включала здоровых фертильных женщин без отягощенного акушерского анамнеза со средним возрастом 31,28 (3,11) года.
Выполнение исследования одобрено Комиссией по этике Центра. От женщин получено письменное добровольное информированное согласие на участие в исследовании и обработку персональных данных.
В качестве материала для исследования использовали сыворотку (плазму) периферической венозной крови.
Иммунологические исследования проводились с использованием методов иммуноферментного анализа (ИФА) и хемилюминесцентного иммуноанализа (ХЛИА) и включали определение широкого спектра аФЛ классов M и G. Антитела к КЛ, β2-ГП-I, ФС, Ан A5, ПТ, ФЭ и комплексу ФС/ПТ определяли в сыворотке крови количественно с использованием иммуноферментных наборов ORGENTEC Diagnostika и AESKU.DIAGNOSTICS (Германия). Антитела классов M и G к β2-ГП-I и IgG-антитела к его домену I выявляли с помощью полуколичественного метода ХЛИА на автоматическом хемилюминесцентном анализаторе ACL Acustar™ (Instrumentation Laboratory Co., США) с использованием наборов HemosIL Acustar (Instrumentation Laboratory Co.) и QUANTA Flash (Inova Diagnostics, США).
Для определения подклассов IgG аФЛ в ИФА использовали конъюгаты мышиных моноклональных антител с биотином к иммуноглобулинам G1, G2, G3 и G4 человека (Sigma Aldrich, США) и стрептавидин, конъюгированный с пероксидазой хрена (Sigma Aldrich), как описано в статье [13]. Авидность IgG-аФЛ определяли с использованием для разведения исследуемых сывороток крови буферного раствора, содержащего хаотропный агент (0,5 M хлорида натрия), с последующим расчетом индекса авидности (ИА, %), как описано Čučnik S. et al. [14].
Для проведения статистического анализа результатов исследования использовали пакеты прикладных программ Microsoft Office Excel 2010, Statistica for Windows (версия 10) и MedCalc (версия 12). Для оценки нормальности распределения значений в выборках применяли тесты Колмогорова–Смирнова и W-критерия Шапиро–Уилка. При нормальном распределении количественные данные представляли как среднее арифметическое (М) и стандартное отклонение (SD) в формате М (SD). При отклонении распределения от нормального данные представляли медианой (Me) с 95% доверительным интервалом (96% ДИ) и значениями 25-го и 75-го процентилей. Для оценки статистической значимости различий между группами по частотным показателям использовали χ2-тест, по непрерывным величинам – U-тест Манна–Уитни. Наличие взаимосвязи между переменными оценивали путем расчета коэффициента корреляции Спирмена. Для выявления связи между независимыми переменными и зависимой бинарной переменной проводили анализ логистической регрессии и ROC-анализ (Receiver Operating Characteristics). Различия считали статистически значимыми при уровне значимости P<0,05.
Результаты и обсуждение
Суммарно аФЛ классов M и G были найдены у 56 (61,5%) женщин с ранним ПВ: антитела к КЛ – у 20 (22%) пациенток, к β2-ГП-I – у 25 (27,5%), к ФЭ – у 22 (24,2%), к Ан A5 – у 22 (24,2%), к ФС/ПТ – у 22 (24,2%), к ФС – у 14 (15,4%), к ПТ – у 9 (9,9%). При этом антитела, отнесенные к классификационным критериям АФС, так называемые «критериальные» антитела (антитела к КЛ, к β2-ГП-I и ВА), выявлялись только в 29 (32,3%) случаях. Кроме этих антител, с высокой частотой детектировались антитела к Ан A5, ФЭ и комплексу ФС/ПТ. Следует отметить, что суммарные антитела к β2-ГП-I обнаруживались чаще, чем антитела к ФС (P=0,047) и ПТ (P=0,004), а антитела к комплексу ФС/ПТ – чаще, чем антитела к ПТ (P=0,01).
Часто выявлялись одиночные аФЛ – в 23 (41,1%) случаях, среди которых преобладали антитела к Ан A5 – в 12 (52,2%) случаях и β2-ГП-I – в 9 (39,1%) случаях. Антитела к КЛ и β2-ГП-I обнаруживались одновременно у 13 (14,3%) женщин, комбинации нескольких аФЛ – у 17 (18,7%), тройная позитивность на критериальные антитела наблюдалась только у 3 (3,3%) пациенток с венозным тромбозом в прошлом. Полученные результаты согласуются с данными Alijotas-Reig J. et al. (2015), свидетельствующими о более высокой частоте выявления одиночных аФЛ при акушерском АФС, чем двойной и тройной позитивности на аФЛ [15], а также с данными Clark C.A. et al. (2013), демонстрирующими низкую частоту положительного ВА (менее 1%) у пациенток с ранним ПВ [16].
У пациенток с ПВ антитела к β2-ГП-I, КЛ, Ан A5, ФЭ, ФС/ПТ классов M или G обнаруживались в 11–17,6% случаев, а антитела IgG к ФС – в 8,8% случаев, то есть значимо чаще, чем у здоровых женщин без потери беременности (в 1,9–4,8% случаев) (рис. 1). Данные аФЛ выявлялись у пациенток с ранним ПВ в 3,4–8,5 раза чаще, чем у здоровых женщин. Наиболее высокие значения отношения шансов (ОШ) были получены для антител IgG к β2-ГП-I (ОШ=7,2; 95% ДИ 2,02–25,54; P=0,002), Ан A5 (ОШ=8,5; 95% ДИ 1,86–38,78; P=0,006) и ФС/ПТ (ОШ=6,1; 95% ДИ 1,69–22,05; P=0,006). Антитела IgG к ФС/ПТ выявлялись у пациенток чаще (у 15,4%), чем к ПТ (у 4,4%) (P=0,01).
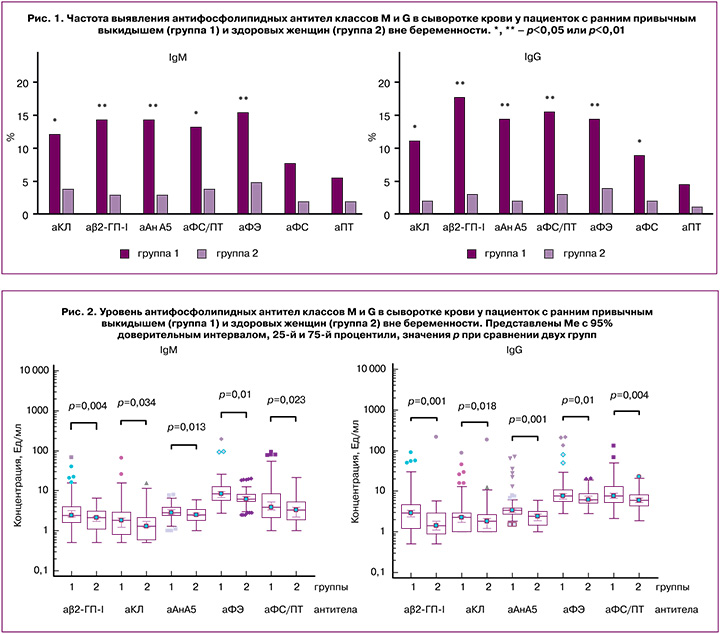
Медианный уровень аФЛ в группе 1 у пациенток с ранним ПВ был выше, чем у здоровых женщин (рис. 2), несмотря на то, что у большинства пациенток отмечались низкие (до 20 Ед/мл) и средние (от 20 до 60 Ед/мл) уровни аФЛ. Исключение составили три пациентки с венозным тромбозом, у которых наблюдались тройная позитивность на критериальные антитела и более высокий уровень антител IgG к КЛ и β2-ГП-I (106 (71,8) GPL-Ед/мл и 120,3 (85,7) Ед/мл соответственно) по сравнению с пациентками без тромботических осложнений (18,6 (7,4) GPL-Ед/мл и 28,5 (19,1) Ед/мл соответственно) (P<0,01). Эти результаты согласуются с данными Gardiner C. et al. (2013) о преобладании у женщин с клиническими признаками акушерского АФС низких титров аФЛ и отрицательных тестов на ВА [17]. Показано, что специфическая терапия АФС значительно улучшает исходы беременности у женщин с низкими титрами аФЛ [18].
Между уровнями антител к КЛ, ФС и β2-ГП-I классов M и G наблюдалась сильная прямая корреляционная связь (r=0,89–0,97; P<0,001) [13]. Корреляционная связь средней силы была найдена между уровнями IgG-антител к ФЭ, ФС/ПТ и аФЛ другой специфичности, что может объясняться особенностями используемой методики, связанными с иммобилизацией на полистирольные планшеты комплексов фосфолипидов и фосфолипидсвязывающих протеинов (β2-ГП-I или ПТ), а также перекрестной реактивностью антител с отрицательно заряженными фосфолипидами. Не найдена значимая корреляционная связь между уровнями антител к Ан A5 и других аФЛ, между уровнями антител к ПТ и комплексу ФС/ПТ, принадлежащими, по-видимому, к разным группам антител.
Именно β2-ГП-I признан главной мишенью аФЛ [1, 6]. Доказано, что β2-ГП-I-зависимые аФЛ проявляют специфический тропизм к плацентарной ткани, связанный с повышенной локальной экспрессией β2-ГП-I на трофобластических и децидуальных клетках, влияют на функционирование этих клеток, вызывают нарушение формирования и развития плаценты [4, 19]. Несмотря на то что во время беременности на клетках дифференцирующегося трофобласта и синцитиотрофобласта экспонируется ФС, именно антитела к β2-ГП-I, а не к ФС ассоциируются с ПВ на раннем сроке. По результатам недавнего систематического обзора (2018), ассоциация между аФС и осложнениями беременности остается недоказанной [20].
Использование метода ХЛИА для исследования эпитопной специфичности антител к β2-ГП-I показало, что у 13 (44,8%) серопозитивных пациенток выявлялись антитела IgG к домену I β2-ГП-I, их медианный уровень составлял 9,85 (3,7; 7664,3) хемилюминесцентных единиц (CU). Уровни антител IgG к β2-ГП-I (по данным ИФА) и к домену I (по данным ХЛИА) хорошо коррелировали между собой (r=0,65; P=0,001). С помощью ROC-анализа установлена высокая вероятность наличия IgG-антител к домену I (ОШ=41,3; 95% ДИ 5,01–339,82; P=0,005) при уровне IgG-антител к β2-ГП-I выше 17,6 Ед/мл. Важно отметить, что полученные данные могут быть использованы для стратификации пациенток по риску тромботических и акушерских осложнений [21].
Хотя антитела могут вырабатываться ко всем пяти доменам β2-ГП-I, именно антитела IgG, направленные против домена I, строго коррелируют с тромботическим АФС и вызывают тромбоз и потерю беременности в биоанализах in vivo [9]. Наблюдаемая корреляция между антителами IgG к домену I и тройной позитивностью на критериальные антитела подтверждает важное значение антител IgG к домену I для выявления пациентов с более высоким риском клинических проявлений АФС [22].
У 25 (40,3%) пациенток, серонегативных на критериальные антитела, с высокой частотой обнаруживались аФЛ другой специфичности: антитела к Ан A5 – у 15 (24,2%), к ФЭ – у 9 (14,5%), к ФС/ПТ – у 5 (8,1%). Антитела к Ан A5 выявлялись чаще, чем антитела к ФС/ПТ, ПТ и ФС (P<0,05), и были единственными аФЛ, обнаруженными у 8 (12,9%) пациенток. Важно отметить, что определение антител к Ан A5, ФЭ и ФС/ПТ может способствовать повышению эффективности диагностики АФС у серонегативных пациенток с ранним ПВ. Полученные результаты согласуются с данными Mekinian A. et al. (2016), демонстрирующими высокую частоту выявления антител к Ан A5, ФЭ и комплексу ФС/ПТ у женщин с клиническими проявлениями АФС, серонегативных на классические критериальные антитела [10].
У пациенток с ПВ отмечались гетерогенная авидность аФЛ и частое выявление IgG-антител со средним (от 30% до 70%) и высоким (более 70%) ИА. При этом средние значения ИА IgG-антител к КЛ, β2-ГП-I и Ан A5 составляли 57,1 (21,2)%, 64,8 (19,7)% и 68,2 (12,9)% соответственно и значимо не различались (P>0,05). Высокоавидные IgG-антитела к КЛ и β2-ГП-I выявлялись в 33,3% и 30% случаев, а высокоавидные IgG-антитела к Ан A5 – в 61,5% случаев. Пациентки с предшествующим венозным тромбозом нижних конечностей характеризовались высоким уровнем, а также высокой авидностью антител класса G к КЛ и β2-ГП-I (ИА>90%). Полученные результаты об ассоциации высокоавидных IgG-антител к КЛ и β2-ГП-I с патологией беременности и тромбозом согласуются с данными Čučnik S. et al. (2012), которые показали более высокое патогенетическое значение высокоавидных аФЛ при тромбозе и акушерской патологии по сравнению с низкоавидными [14].
У пациенток с ПВ на раннем сроке беременности отмечалось повышение уровня аФЛ, принадлежащих к разным подклассам IgG. По частоте выявления преобладали IgG2-антитела к КЛ и β2-ГП-I, эти антитела выявлялись чаще (в 80% и 62,5% случаев), чем IgG1- (в 30% и 18,7%), IgG3- (в 30% и 25%) и IgG4-антитела (в 20% и 25%) данной специфичности (P<0,05). Антитела к Ан A5, принадлежащие к разным подклассам IgG, не различались по частоте выявления, при этом повышение уровня IgG1, IgG2 и IgG3 отмечалось в 30,8–38,5% случаев, IgG4 – в 53,8% случаев (P>0,05).
Мало исследований фокусировалось на определении подклассов аФЛ, хотя принадлежность к определенному подклассу характеризует потенциальную активность антител. Важно отметить, что IgG-антитела разных подклассов имеют различное патогенетическое значение и эффекторные функции [23]. Каждый подкласс IgG характеризуется уникальными свойствами, определяющими связывание антигена, образование иммунных комплексов, активацию комплемента, инициацию эффекторных клеток, экспрессирующих Fcγ-рецепторы, период полужизни и трансплацентарный транспорт. В немногочисленных данных, опубликованных ранее, отмечалась ассоциация антител к КЛ и β2-ГП-I подклассов G2 и G3 с артериальным и венозным тромбозом и потерей плода, а также предиктивное значение их идентификации для повышенного тромботического риска.
Результаты логистического регрессионного анализа при использовании в качестве предикторов аФЛ классов M и G, а в качестве зависимой переменной – диагноза раннего ПВ у женщин показали наиболее выраженную взаимосвязь между ПВ и IgG-антителами к β2-ГП-I (ОШ=1,67; 95% ДИ 1,33–2,11) и Ан A5 (ОШ=2,32; 95% ДИ 1,67–3,23) (p<0,001). Результаты проведенного ROC-анализа показали, что определение IgG-антител к β2-ГП-I и Ан A5 характеризовалось высокими значениями чувствительности, специфичности, площади под кривой (AUC), положительной и отрицательной прогностической значимости для раннего ПВ (таблица), показатели точности тестов достигали 65,5% и 67,1%. При определении антител IgG к ФС/ПТ и антител IgM к ФЭ также были получены высокие значения операционных характеристик тестов.
ROC-кривые позволяли дифференцировать пациенток с ранним ПВ и здоровых женщин по уровню аФЛ классов G и M (рис. 3). Предсказательная способность модели оценивалась по значениям AUC (более 0,7) как хорошая при использовании в качестве предикторов IgG-антител к β2-ГП-I и Ан A5, и была выше, чем при использовании аналогичных IgM-антител, а также IgM- и IgG-антител к ФС и ПТ, IgG-антител к ФЭ (P<0,05). По результатам логистического регрессионного анализа, одновременное определение комбинации IgG-антител к Ан A5, β2-ГП-I, ФС/ПТ и IgM-антител к ФЭ приводило к повышению значения AUC до 0,852 (95% ДИ 0,794–0,899) (P<0,001), а точность теста достигала 78,9%.

Учитывая, что антитела к Ан A5 часто выявляются у пациенток, серонегативных на критериальные антитела (в 24,2% случаев), их определение может способствовать повышению эффективности диагностики акушерского АФС, в связи с этим существует необходимость использования теста на антитела к Ан A5 в клинической практике для обследования женщин с ПВ на раннем сроке. Полученные результаты об ассоциации антител к Ан A5 с ПВ на раннем сроке согласуются с данными Чепанова С.В. и соавт. (2014) [24], а также подтверждаются результатами исследования Bećarević M. и соавт. (2016), демонстрирующими важное значение этих антител при акушерском АФС [25].
Как известно, Ан A5 является естественным антикоагулянтом, который предотвращает активацию факторов свертывания крови путем образования защитного щита над отрицательно заряженной фосфолипидной поверхностью трофобласта и эндотелия сосудов. По-видимому, огромное скопление эндогенного Ан A5 на апикальной поверхности синцитиотрофобласта во время беременности может запустить образование антител против Ан A5. Нарушение сборки или повреждение защитного аннексинового щита под воздействием аФЛ, направленных против ФЛ-связывающих протеинов или Ан A5, представляет важный патогенетический механизм развития тромбоза и потери беременности при АФС [5, 26].
Хотя диагностическое значение антител к ФЭ ниже, чем антител к β2-ГП-I и Ан A5, их обнаружение способствует более полному выявлению АФС у серонегативных пациенток с ранним ПВ. В подтверждение этого, недавно с применением тонкослойной хроматографии была продемонстрирована высокая частота встречаемости антител к ФЭ при серонегативном АФС [27]. Предполагается, что кининогензависимые антитела к ФЭ имеют патогенетическое значение при ранних потерях беременности, так как могут вызывать нарушения в функционировании калликреин-кининовой системы [28].
Важно отметить, что антитела к ФС/ПТ выявлялись у пациенток с ПВ на раннем сроке, серонегативных на критериальные антитела, в 8,1% случаев. При этом именно наличие антител к комплексу ФС/ПТ, а не антител к ПТ, ассоциировалось с ПB. Идентификация антител к ФС/ПТ позволит дополнительно диагностировать АФС в случаях, не выявляемых рутинными методами диагностики АФС [6]. Как показали результаты недавнего международного мультицентрового исследования, IgG-антитела к комплексу ФС/ПТ имеют важное диагностическое значение для акушерского АФС [29]. Тест на антитела к комплексу ФС/ПТ признается пригодным для практического использования при обследовании женщин с ПВ [30].
Заключение
Таким образом, ПВ на раннем сроке беременности ассоциируется с широким спектром аФЛ, включающим, кроме антител, отнесенных к критериям АФС, антитела к Ан A5, ФЭ и ФС/ПТ, выявление которых способствует повышению эффективности диагностики АФС. IgG-антитела к β2-ГП-I и Ан A5 являются независимыми факторами риска раннего ПВ и имеют высокое диагностическое значение при данной патологии. При комбинации IgG-антител к β2-ГП-I, Ан A5, ФС/ПТ и IgM-антител к ФЭ достигается высокая точность теста. При среднем и высоком уровне IgG-антител к β2-ГП-I имеется повышенный риск наличия антител к домену I β2-ГП-I. ПВ ассоциируется с IgG-антителами к КЛ и β2-ГП-I со средним и высоким уровнем авидности с преобладанием подкласса G2 и высокоавидными IgG-антителами к Ан A5, принадлежащими к четырем подклассам. Антитела к Ан A5, ФЭ и ФС/ПТ представляют перспективные диагностические маркеры акушерского АФС.