Своевременная диагностика и коррекция аномалий развития половых органов является актуальной проблемой современной гинекологии, так как у пациенток с этой патологией часто возникают бесплодие, осложнения процесса гестации и родов [1, 2]. В общей популяции аномалии развития матки выявляются с частотой 4,3–12%, среди пациенток с бесплодием – в 8%, у женщин с самопроизвольным выкидышем в анамнезе – в 13%, у пациенток с привычной потерей беременности в 5–16,7% случаев [1, 3–5]. Истинная распространенность пороков развития матки неизвестна, так как у многих пациенток эти аномалии не проявляются клинически. От 33,3 до 59,5% женщин с пороками развития матки имеют успешную первую беременность [6].
Первые классификации аномалий развития органов репродуктивной системы были предложены в середине девятнадцатого века. Они были основаны на данных эмбриологии и представлениях о развитии мюллеровых протоков. В первой половине ХХ века Ombredanne и Martin (1905), Strassmann (1907), Piquand (1910), а также ряд других авторов, предложили свои классификации. Позднее, в 1981 году, Jones разделил мюллеровы аномалии на три группы: агенезия, дефекты вертикального и латерального слияния. Эта классификация была достаточно простой и широко используемой. Наиболее приемлемой для применения в практике стала классификация Buttram V. и Gibbons W. (1983). Именно она в последующем с небольшими изменениями была принята и рекомендована для общего использования Американским обществом репродуктивной медицины (ASRM). Единственным отличием классификации ASRM от классификации Buttram V. (1983) стало выделение uterus arcuate в отдельный класс [7].
Классификация ASRM выделяет семь классов аномалий развития матки на основании анатомических изменений. Она не является исчерпывающей, а используется для идентификации мюллеровых аномалий внутри общей классификации генитальных пороков развития. Согласно классификации ASRM, I класс – это «мюллеровы» агенезии и гипоплазии, hypoplasis/agenesis (I.А. вагинальные, I.В. цервикальные, I.С. донные, I.D. трубные, I.Е. комбинированные). II класс – однорогая матка, uterus unicornuate (II.А. с рудиментарным рогом, сообщающимся с полостью основного рога, II.B. с рудиментарным рогом, не сообщающимся с полостью основного рога, II.C. с рудиментарным рогом без полости, II. D. однорогая матка без добавочного рога). Класс III – удвоение матки с шейкой, uterus didelphus. Класс IV – двурогая матка, uterus bicornuate (IV.А. полное разделение до внутреннего зева, IV.В. частичная). Класс V – матка с внутриматочной перегородкой, uterus septate (А. полная, В. частичная). Класс VI – uterus arcuate. Класс VII – матка с изменениями формы полости, обусловленными внутриутробным воздействием диэтилстильбэстрола, DES Drug Related (матка с Т-образной формой полости, тяжи в полости, матка расширенная в нижних ¾ полости матки). Причиной для выделения uterus arcuate в отдельный класс явилось то, что неблагоприятные клинические исходы при этой аномалии наблюдаются редко [8].
В эмбриологической классификации женских мочеполовых нарушений Acien P. и соавт. (2004) выделена группа мюллеровых аномалий – изолированная или распространенная маточная или маточно-вагинальная аномалии, связанные с парамезонефральными или мюллеровыми протоками. В этой группе выделяется подгруппа A.1. – агенезия/гипоплазия матки, А.2. – однорогая матки (unicornuate uterus) и ее различные варианты, А.3. – удвоение матки с шейкой (uterus didelphus), А.4. – двурогая матка (uterus bicornuate), А.5. – матка с внутриматочной перегородкой полной, неполной (septate and subseptate uterus). В подгруппу А.6. выделена uterus arcuate, в A.7. – аномалии, связанные с синдромом DES (последствия внутриутробного воздействия диэтилстильбэстрола) [9].
Классификация аномалий развития половых органов VCUAM (2005) построена по аналогии с классификацией TNM (2003), используемой для характеристики онкологических опухолей. В соответствии с данной классификацией V (vagina) – обозначает аномалии развития влагалища, С (cervix) – шейки матки, U (uterus) – матки, А (adnex) – придатков матки, М (associated malformations) – сочетанные аномалии развития мочевыделительной, костно-суставной, сердечно-сосудистой и нервной системы. По мнению авторов, в отличие от предыдущих классификаций, данная позволяет детально описать сложные пороки развития половых органов и сопутствующие аномалии других органов и систем. Если какая-то аномалия не может быть учтена с помощью пунктов данной классификации, то она может быть задокументирована символом «+». Если вид порока остается невыясненным, то этой категории аномалий присваивается знак «#». В соответствии с данной классификацией, нормальная матка обозначается как 0, uterus arcuate – 1а, продольная внутриматочная перегородка (septate), занимающая менее 50% полости матки – 1b, продольная внутриматочная перегородка, занимающая более 50% полости матки – 1с, двурогая матка (bicornuate) – 2, гипопластическая матка (hypoplastic uterus) – 3, односторонний рудиментарный рог при однорогой матке (unilaterally rudimentary or aplastic) – 4а, двусторонние маточные рудименты или рудиментарные рога при аплазии матки - синдром Рокитанского (bilaterally rudimentary or aplastic) – 4b, другие – «+», неизвестные – «#» [10, 11].
В 2013 году Европейское общество репродукции человека и эмбриологии (ESHRE) и Европейское общество гинекологической эндоскопии (ESGE) разработали клинико-анатомическую классификацию аномалий развития женских половых органов. В качестве основной характеристики в данной классификации используется анатомия женских половых органов. В отличие от других классификационных систем, в данную введено понятие нормальной матки, что позволяет, по мнению авторов, более эффективно систематизировать шеечные и вагинальные аномалии. В данной классификации отказались от терминов двурогая матка и удвоение матки (uterus bicornuate, uterus didelphus), эти два понятия были заменены на термин бикорпоральная матка (bicorporeal uterus). Uterus arcuate не выделяется в отдельную категорию, так как определение и клиническое значение данной аномалии не совсем понятно. Данная классификация состоит из 5 классов. U0 – нормальная матка. Класс U1 морфологически измененная или дисморфичная матка. В этот класс включены матки с нормальным наружным контуром дна, но с аномальной полостью матки, исключая перегородки. U1а – матка с Т-образной полостью. U1b – инфантильная матка. U1c – «другие». В группу «другие» включаются матки с незначительной деформацией полости в дне, отличающиеся от внутриматочной перегородки. Класс U2 – матка с перегородкой или септированнная матка. U2a – частичная внутриматочная перегородка (полость матки разделена выше уровня внутреннего зева шейки матки). U2b – полная внутриматочная перегородка (полость матки разделена полностью, до уровня внутреннего зева). Эта перегородка может распространятся на шейку матки и влагалище. Класс U3 – бикорпоральная матка. Внешний контур такой матки в области дна деформирован. Углубление в дне частично или полностью разделяет тело матки на две части, это деление может касаться как шейки матки, так и/или влагалища. U3a – частичная бикорпоральная матка. Тело матки разделено выше внутреннего зева шейки матки. U3b – полная бикорпоральная матка. Тело матки разделено до уровня внутреннего зева. U3c – бикорпоральная матка с перегородкой. Помимо деления тела матки на две части, имеется перегородка в полости матки. Класс U4 – однорогая матка. U4a – однорогая матка с рудиментарной полостью. В данном случае имеется контрлатеральный функционирующий, сообщающийся или не сообщающийся с основной полостью, рог. U4b – однорогая матка с наличием рудиментарного рога без эндометриальной полости (то есть с наличием нефункционирующего рудиментарного рога). Класс U5 – аплазия матки. U5a – аплазия матки с односторонней или двусторонней рудиментарной функционирующей полостью. U5b – аплазия матки без рудиментарной функционирующей полости. Класс U6 – не классифицируемые случаи. Класс С – сопутствующие аномалии шейки матки. Класс V – сопутствующие аномалии влагалища [12].
В России широко используется классификация Е.А. Богдановой и Г.Н. Алимбаевой (1991). В III класс этой классификации – пороки, связанные с отсутствием слияния или неполным слиянием (удвоением) протоков репродуктивной системы, наряду с удвоением тела и шейки матки при наличии одного влагалища, выделены такие аномалии развития, как удвоение тела матки при наличии одной шейки матки и одного влагалища. В этой подгруппе выделяется седловидная матка, двурогая матка и матка с полной или неполной внутренней перегородкой [13]. В нашей стране также хорошо известны классификации Е.М. Демидовой и А.Г. Курбановой (1983), в которых основное внимание уделено порокам развития матки и влагалища, затрудняющим отток менструальной крови [14].
Классификация З.Н. Макияна (2010) включает: аномалии развития гонад, матки, влагалища и наружных половых органов. В соответствии с этой классификацией выделяется матка с внутриматочной перегородкой. Перегородка может быть полной, протяженностью до наружного зева шейки матки (в сочетании/или без удвоения влагалища) и неполной – не доходящей до внутреннего зева. По этой классификации выделяется двурогая матка в двух формах: полная форма (раздвоение полости на уровне внутреннего зева) и неполная форма (раздвоение полости выше внутреннего зева), а также седловидная матка [15].
Л.В. Адамян и А.З. Хашукоева (1998) на основании клинического обследования и лечения 855 больных предложили классификацию пороков развития матки и/или влагалища, отличающуюся клинико-анатомическим подходом. Она позволяет правильно установить характер патологии и выработать оптимальную тактику лечения. В IV класс этой классификации выделена двурогая матка. Этот класс включает 3 подкласса. Подкласс 1 – седловидная матка, подкласс 2 – неполная форма двурогой матки, подкласс 3 – полная форма двурогой матки. В V класс вынесена внутриматочная перегородка. Подкласс 1 – полная внутриматочная перегородка (до внутреннего зева), подкласс 2 – неполная внутриматочная перегородка. В классификации указывается на то, что перегородка может быть тонкой или на широком основании, одна гемиполость может быть длиннее другой [16].
Сложность диагностики аномалий развития матки во многом определяется тем, что в современных классификациях, включая классификацию ASRM, отсутствуют четкие определения и объективные характеристики пороков развития матки. Использование различных методологических подходов в диагностике аномалий развития половых органов не позволяет в настоящее время четко отработать принципы консультирования и лечения пациенток [1].
На сегодняшний день наиболее доступным, безопасным и точным методом диагностики аномалий матки является ультразвуковой метод исследования [4, 17–19]. Существует несколько принципиально различных подходов к диагностике аномалий половых органов с использованием эхографии.
Аномалия развития матки может быть диагностирована при ультразвуковом исследовании в 2D режиме. При проведении этого исследования необходимо получить несколько продольных и поперечных срезов тела матки для оценки наружного контура матки и контура эндометрия. Для uterus arcuate характерна одинаковая длина тела на центральном, правом и левом боковых продольных срезах. Длина тела матки на центральном срезе может быть короче, но не более чем на 10 мм длины матки на уровне боковых срезов. То же самое характерно для длины контура эндометрия. На поперечных срезах через дистальные отделы контур матки в виде овала, вытянутого в поперечном направлении. Эндометрий определяется в виде двух овальных структур, расположенных ближе к наружному контуру правой и левой стенки матки. На поперечном срезе через среднюю часть матка представлена овальной структурой, по центру которой расположено срединное маточное эхо. При матке с внутриматочной перегородкой длина тела на боковых и центральном продольных срезах одинакова или длина тела матки на центральном срезе короче, но не более чем на 10 мм длины на уровне боковых срезов. На поперечных срезах, полученных на уровне дистальных и центральных отделов, контур тела матки правильный, в виде овала, срединное маточное эхо удвоено. При двурогой матке длина тела и контура эндометрия на боковых продольных срезах больше длины тела матки и контура эндометрия на уровне центрального среза. Разница в длине превышает 10 мм. На поперечном срезе через дистальные отделы тело матки представлено двумя отдельными овальными структурами, каждая из которых имеет срединное маточное эхо. На поперечном срезе через среднюю часть тело матки представлено овальным образованием с удвоенным срединным маточным эхо. Исследование в 2D режиме позволяет опытному специалисту поставить диагноз мюллеровой аномалии, однако ультразвуковое исследование с использованием режима 3D реконструкции является более чувствительным и специфичным [4].
Методика ультразвукового исследования в режиме 3D реконструкции основана на оценке коронарной плоскости. Все современные подходы к диагностике маточных аномалий основываются на оценке расположения наружного и внутреннего контура дна матки по отношению к линиям, проведенным через устья маточных труб и на уровне наружного контура дна матки.
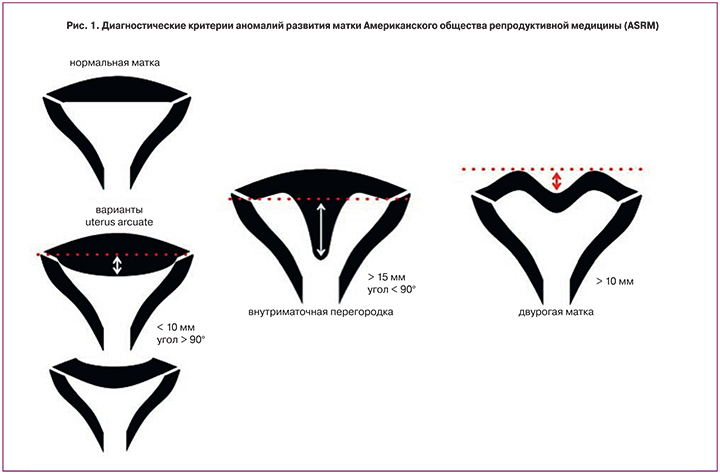
В соответствии с классификацией ASRM, нормальная матка и uterus arcuate имеют нормальный внешний контур дна. Внутренний контур плоский или расположен не более чем на 10 мм ниже линии, проведенной через устья маточных труб. Угол, который образует выступающий в полость матки внутренний контур дна, тупой. Матка с внутриматочной перегородкой имеет нормальный внешний контур дна. Внутренний контур расположен более чем на 15 мм ниже линии, соединяющей устья маточных труб. Угол, который образует выступающий в полость матки внутренний контур дна, острый. Диагноз двурогой матки ставится, если в дне матки есть углубление и наружный контур дна располагается более чем на 10 мм ниже линии, проведенной через наружный контур дна матки. Внутренний контур дна матки похож на контур дна матки при внутриматочной перегородке [3, 8] (рис. 1).
Второй подход к диагностике аномалий развития матки представлен в консенсусе ESHRE и ESGE. Отправной точкой в диагностике аномалий развития матки является оценка толщины стенки матки. В соответствии с этим подходом на коронарном срезе матки проводят линию, соединяющую устья маточных труб и линию на уровне внешнего контура дна. Если внешний контур дна не деформирован, то толщина стенки матки – это расстояние между линией, проведенной через устья маточных труб, и внешним контуром дна. При наличии углубления в дне матки под толщиной стенки понимается расстояние между построенными раннее линиями. В качестве альтернативы оценивается толщина передней, задней или боковой стенки матки в средней части тела. Измерение проводится на уровне середины расстояния между внутренним зевом и дном полости, под углом 90° к границе эндометрия и миометрия. Толщина стенки – это средняя величина от толщины двух стенок. Если внутренний контур дна матки выступает в полость, то нужно оценить длину выступающей части, измерив расстояние между линией, соединяющей устья маточных труб и самой нижней точкой внутреннего контура дна [20].
В соответствии с данным подходом в нормальной матке наружный контур дна без углублений, а внутренний – ровный или изогнутый. Внутренний контур дна полости матки может выступать в полость относительно линии, соединяющей устья маточных труб, но не более чем на 50% от толщины стенки матки. Морфологически измененная или дисморфичная матка имеет нормальный наружный контур дна и аномальную форму полости матки. Полость Т-образной матки сужена за счет утолщения боковых стенок. Соотношение длины тела и шейки в такой матке 2/3 и 1/3 соответственно. Полость инфантильной матки узкая, но без утолщения боковых стенок. Соотношение длины тела и шейки матки 1/3 и 2/3. В соответствии с классификацией ESHRE/ESGE, в группу «другие» выделяются матки, в которых внутренний контур дна матки выступает в полость относительно линии, соединяющей устья маточных труб не более чем на 50% толщины стенки матки. Это uterus arcuate. Матка с продольной перегородкой имеет нормальный внешний контур в области дна. Выступающая в полость матки часть дна имеет длину, превышающую 50% толщины стенки матки. При частичной внутриматочной перегородке полость матки разделена выше уровня внутреннего зева шейки матки, при полной перегородке полость матки разделена до уровня внутреннего зева. Эта перегородка может распространяться на шейку матки и/или влагалище. Если внешний контур матки в области дна деформирован, имеет углубление, то такую матку характеризуют, как бикорпоральную. Углубление в области дна расположено ниже линии, проведенной через наружный контур дна матки, и превышает по длине 50% толщины стенки матки. Это углубление может частично или полностью разделять тело матки, касаться как шейки матки, так и/или влагалища. В частичной бикорпоральной матке тело разделено выше внутреннего зева шейки матки. В полной бикорпоральной матке тело матки разделено до уровня внутреннего зева. В бикорпоральной матке с перегородкой, помимо деления тела матки на две части, имеется перегородка в полости матки, длина этой перегородки более 50% толщины стенки матки [12] (рис. 2).
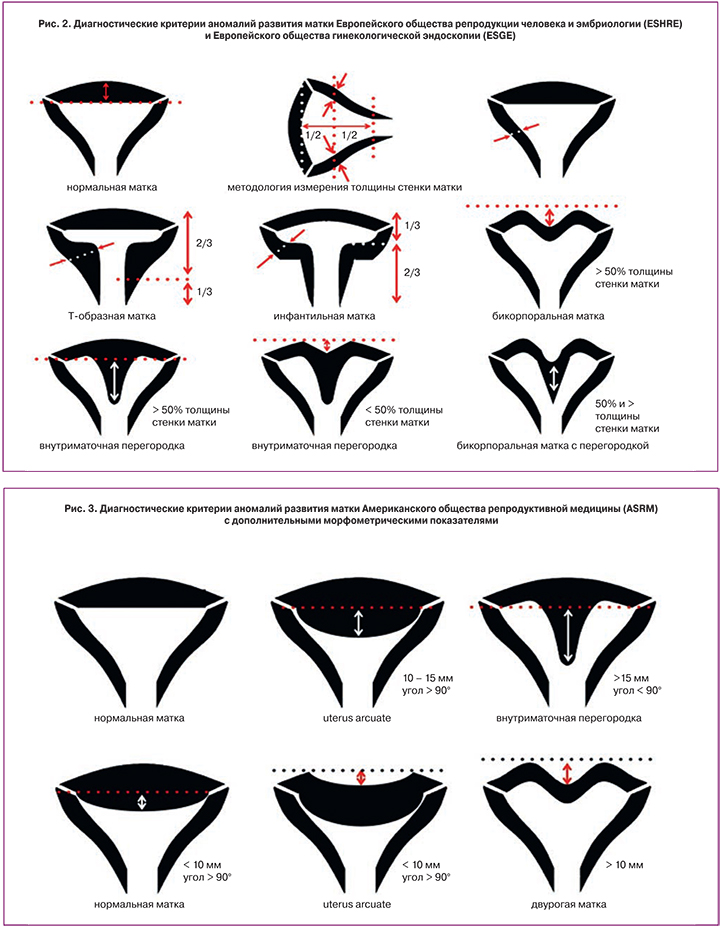
Оба подхода к диагностике пороков развития матки не являются оптимальными. Использование диагностических критериев ESHRE/ESGE не позволяет отличить нормальную матку от uterus arcuate, а также, по мнению ряда авторов, приводит к гипердиагностике матки с внутриматочной перегородкой. Эти исследователи считают, что диагностические критерии ASRM, дополненные некоторыми простыми морфометрическими критериями, являются более объективными [21–23]. Предложенные дополнительные морфометрические критерии позволяют более четко дифференцировать внтуриматочную перегородку и uterus arcuate. В соответствии с данным подходом, если внутренний контур дна расположен менее чем на 10 мм ниже линии, соединяющей устья маточных труб, а угол, образуемый внутренним контуром дна тупой, то такую матку следует характеризовать как нормальную. Наружный контур дна нормальной матки не имеет углублений. Если внутренний контур дна располагается на 10–15 мм ниже линии, соединяющей устья маточных труб, а угол, образуемый внутренним контуром дна матки, является тупым, то в такой ситуации следует поставить диагноз uterus arcuate. При uterus arcuate наружный контур дна матки ровный или имеет углубление в центре. Нижняя точка этого углубления располагается не более чем на 10 мм ниже горизонтальной линии, проведенной через наружный контур дна матки. В том случае, если внутренний контур дна матки выступает в полость более чем на 15 мм, а угол, образуемый внутренним контуром дна, острый, то в этом случае необходимо поставить диагноз внутриматочной перегородки. Матка характеризуется как двурогая, если по средней линии дна матки есть углубление. Нижняя точка этого углубления расположена более чем на 10 мм ниже линии, проведенной через внешний контур дна матки. При этом внутренний контур дна такой же, как при внутриматочной перегородке [6, 7] (рис. 3).
Этот диагностический подход позволяет более точно охарактеризовать аномалии развития матки, однако в соответствии с ним, при uterus arcuate внутренний контур дна матки расположен на 10–15 мм, а при внутриматочной перегородке более чем на 15 мм ниже линии, соединяющей устья маточных труб. Граница между этими двумя состояниями нечеткая. Не понятно, нужно ли проводить метропластику для улучшения исхода последующей беременности, если дно матки выступает в полость на 10–15 мм. Именно поэтому ряд исследователей считают, что диагноз матки с внутриматочной перегородкой следует ставить уже тогда, когда внутренний контур дна полости матки расположен более чем на 10 мм ниже линии, соединяющей устья маточных труб [5].
Заключение
Таким образом, в настоящее время наиболее определенными и точными диагностическими критериями аномалий матки являются критерии ASRM, дополненные рядом морфометрических показателей, а также критерии ESHRE и ESGE. Совместное использование этих критериев позволяет достаточно четко дифференцировать вид аномалии развития матки и определять оптимальную тактику лечения.