The computer-assisted clinical and diagnostic data analysis system for planning an optimal surgical intervention in newborns with lung malformations
Objective. To develop a computer-assisted clinical and diagnostic data analysis system and to evaluate its effectiveness for the preoperative preparation and choice of an optimal surgical treatment for children with congenital lung malformations.Dorofeeva E.I., Podyrovskaya Yu.L., Tumanova U.N., Nemkovskyi G.B., Balashov I.S., Prokhin A.V., Bychenko V.G., Degtyarev D.N.
Subjects and methods. The investigators carried out a retrospective and prospective analysis of the clinical and instrumental data of a total of 144 neonatal patients with bronchopulmonary sequestration and/or cystic adenomatoid lung malformation for the period of January 1, 2012 to June 31, 2018. Segmentation of DICOM chest CT images was performed to create a three-dimensional model with an evaluation of the impact on the duration of surgery for lung defects in newborns.
Results. The standardization and computer-assisted analysis of clinical and diagnostic information made it possible to optimize the stage of training of a surgeon for endoscopic surgery and to considerably reduce the duration of surgery.
Conclusion. The structured visual diagnostic, clinical, and phenotypic signs included in the libraries of the computer expert system (neural network) are a reason to subsequently create a data model with a wide range of practical applications.
Keywords
Currently, the development of neonatal surgery involves the creation of new technical solutions for visualizing the patient’s organs and systems as well as estimating their pathological changes that cause the disease. Complex assessment of these data is of particular importance for preparing and performing surgical interventions in the neonatal period. Modern neonatal surgery is aimed at conducting minimally invasive surgical interventions to correct congenital malformations. Preference is given to endoscopic surgical access, which has already proved to be effective; however, it is technically complicated and accompanied by increased intraoperative risks [1-3]. Existing research methods and technologies for processing visual information including computer graphics are the basis for solving the technical problem of automated accompaniment of the surgeon’s work in the natural environment and augmented reality [4].
Congenital malformations of the lungs (bronchopulmonary sequestration (BS) and congenital cystic adenomatous malformation (CCAM)) occur with a frequency of 1:8000 to 1:35000 live births and are characterized by the presence of tissue sites of an abnormal cystic structure of various sizes; these sites are not completely involved in respiration and gas exchange that is accompanied by a high risk of respiratory failure and infectious complications [1–3]. A feature of the BS is the lack of direct connection with the bronchi, abnormal blood supply along the vessels of systemic blood circulation. The pathological tissue site can be located separately from the healthy lung, or can be a part of it. CCAM is a pathological cystic part of the lung connected with the tracheobronchial tree, and it is usually limited by one of the lobes.
The most accurate diagnostic method for visualizing these malformations is multispiral computed tomography (MSCT). Intravenous contrast, iopromide, is used to reconstruct the differences of vascularisation of the affected parts of the lung as well as to detect the presence of abnormal feeding vessels from the aorta [1–3]. A method for treating BS and CCAM is a surgical intervention aimed at removing abnormal areas of the lung that may be associated with an increased risk of complications during searching, mobilizing and ligation of one or several large abnormal vessels with a diameter not less than the kidney and spleen arteries. In the treatment of congenital CCAM, lobectomy of the affected lobe is recommended [1–3]. As a rule, access to vascular and bronchial elements of the lobe is carried out along the inter-lobe fissure, but in some cases the fissure is not apparent or absent at all, which in combination with an abnormal blood supply presents difficulties for the surgical correction of the defect. The experience of developing intelligent systems for medical applications has shown their effectiveness in adopting complex multi-component solutions [5, 6]. A key stage in the development of an effective intraoperative navigation complex in neonatal surgery is the creation of the system of automated analysis and segmentation of diagnostic information. Segmentation is necessary for the transformation of DICOM images into a 3D model of the affected organ at the preoperative stage.
The objective of the study was to develop and evaluate the effectiveness of a computer-assisted clinical and diagnostic data analysis system on the basis of standards for data collection, classification of laboratory and instrumental studies, and segmentation of 3D images of the chest. The assessment of the system is conducted for preoperative preparation and the choice of the optimal method of surgical treatment in children with congenital lung diseases.
Materials and Methods
The work was carried out in the Neonatal Surgery Department of National Medical Research Center for Obstetrics, Gynecology and Perinatology, in Moscow. It included the following stages:
- retrospective analysis of primary medical records of newborn patients who were examined and surgically treated from January 1, 2012 to December 31, 2016 and selection of cases according to the main diagnosis criterion as BLS and/or CCAM;
- collection and prospective analysis of clinical and instrumental data of newborn patients with BLS and/or CCAM for the period from January 1, 2017 to June 31, 2018;
- formation of a bank of diagnostic DICOM images in patients with signs of congenital lung disease;
- segmentation of diagnostic images using specialized software Myrian Expert, Intrasense (France) according to the original developed algorithms followed by the creation of a 3D model of the respiratory tract and lungs in the patient with diagnosed pathological focus;
- comparative analysis of the features and duration of thoracoscopic surgical intervention in patients with lung malformations during the preoperative image analysis and before its implementation.
The newborns were examined using general clinical, instrumental and laboratory methods during the period of early adaptation, which were supplemented by a direct X-ray of the chest, ultrasonic studies of the pleural cavities with SIEMENS ACUSON S2000 (Germany-USA), linear probe 7 to 14 MHz and 18 to 20 MHz (original method developed in the Centre) and computed tomography of the chest (Toshiba Aquilion Prime, Japan) low volume scanning and contrast-enhanced vessels with iopromide drug.
Results and Discussion
A total of 144 patients with lung malformations (BLS and CCAM) were examined and treated in the Neonatal Surgery Department of the Center from January 1, 2012 to June 31, 2018.
At the first stage of the study (retrospective analysis of medical documentation) from January 1, 2012 to December 31, 2016, the doctors took the decision on the preparation for operation and extent of surgery using traditional logical medical analysis of clinical and diagnostic information on the basis of professional experience. During this period, 58 children with diagnoses of BLS and CCAM underwent thoracoscopic surgery. The detailed analysis of the primary medical records showed that the clinical and diagnostic data included non-formalized descriptions, which were highly susceptible to variability depending on the experience of the specialist and the perception of information. This fact makes it difficult to use information technology in the processing different medical data.
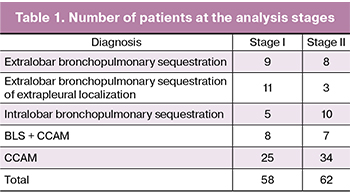 At the second stage of the study (clinical diagnostic data analysis) since January 1, 2017, in addition to the classical method of decision-making, there has been a system of computer analysis of clinical diagnostic data and image segmentation with the creation of 3D models of the respiratory tract and lungs in BLS and CCAM. Using this system 62 newborns were examined and prepared for surgery. The range of diagnoses in patients with congenital lung diseases included in the study is presented in Table 1.
At the second stage of the study (clinical diagnostic data analysis) since January 1, 2017, in addition to the classical method of decision-making, there has been a system of computer analysis of clinical diagnostic data and image segmentation with the creation of 3D models of the respiratory tract and lungs in BLS and CCAM. Using this system 62 newborns were examined and prepared for surgery. The range of diagnoses in patients with congenital lung diseases included in the study is presented in Table 1.
As can be seen in the table, the total number of patients with congenital lung diseases included in the study as well as within each type of abnormality at stages I and II was comparable.
At the second stage of the study, clinical and diagnostic data were typed and structured to standardize all the information received about the patient. An example of such processing would be the translation of textual medical descriptions of the radiation studies performed by different specialists in conventional form into the system of specified information fields. The principle of unifying the textual description of the organs structure and pathological foci in congenital lung malformations is presented in Table 2. In case of identification of the parameters demanding specification, additional information was indicated in the column ‘Note’. For example, when an abnormal supply vessel from the aorta was detected, the anatomical origin of the vessel entrance was placed in the column ‘Note’.
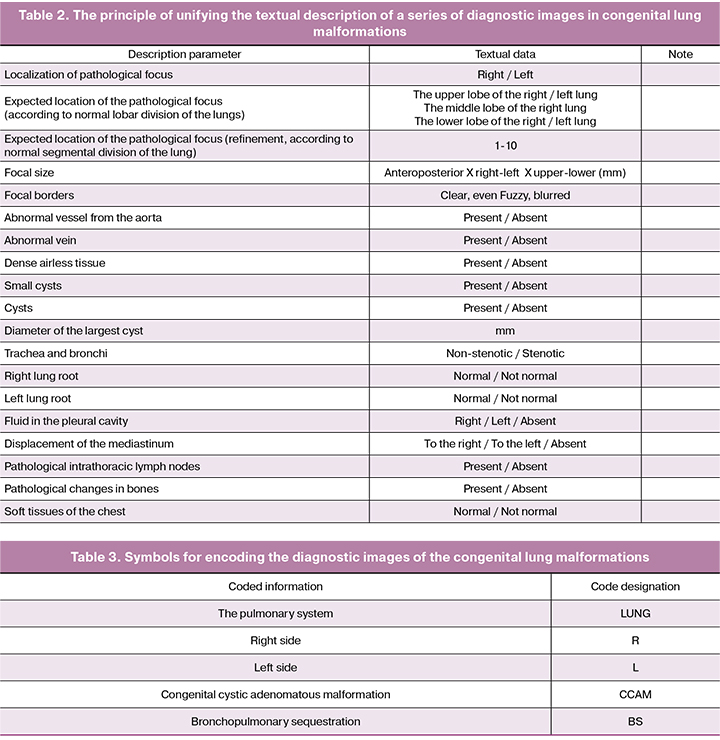
Diagnostic series of computed tomography images of the patients’ chest organs obtained at the second stage of the study as well as patients’ archival results of the retrospective first stage were copied to the data bank with the creation of a personal catalog. In order to use the information for the purpose of research, personal identity information was excluded from the database due to the current legislation. Each series of diagnostic images of patients with congenital lung malformations was assigned an identification code with a number. The symbols of the encoded information are presented in Table 3.
Thus, if the series was encoded «LUNG_L_BS_217», it corresponded to the series number 217 of the patient with congenital bronchopulmonary sequestration on the left; if it was «LUNG_R_CCAM_121», it related to the series number 121 of the patient with congenital cystic adenomatous malformation of the right lung. The data on the assigned codes were stored in the primary directory, accessible only to the head of the medical unit. Thus, the data bank contained 1082 series of diagnostic images, which met the criteria of the required quality for subsequent software processing.
We have developed an original algorithm of actions when performing preoperative segmentation of a series of diagnostic images using tools of specialized software Myrian Expert. This algorithm is presented by means of the example with congenital extralobar BLS (Fig. 1a):
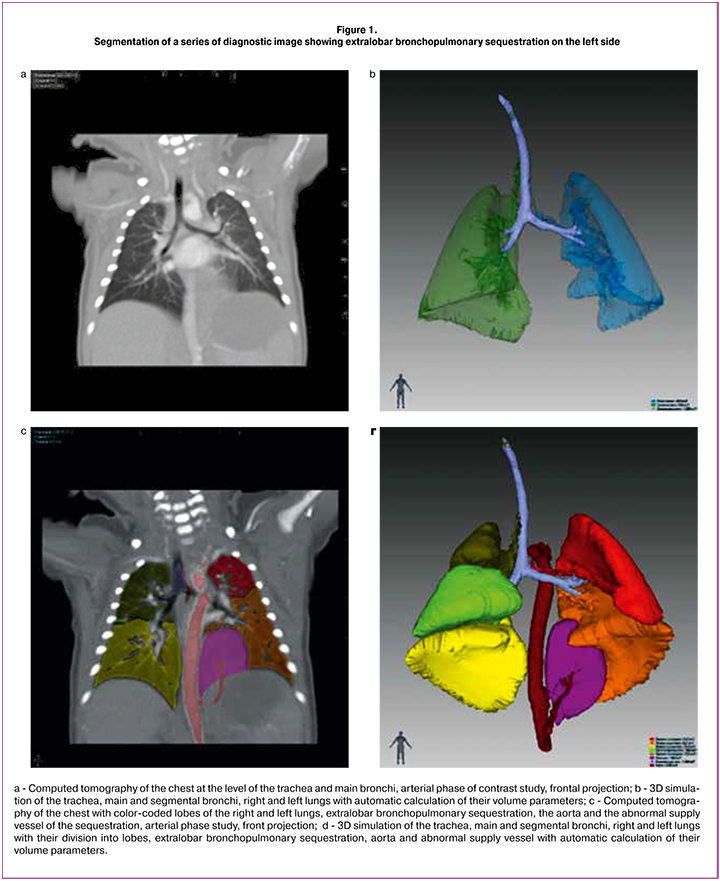
Volumetric visualizing the trachea, major and segmental bronchi, automatic calculation of the diameter and length of the airway (Fig. 1b);
Auto-filling the volume of the right and left lungs, automatic calculation of the volume of the right and left lungs (Fig. 1c);
Division of the right and left lungs into lobes (Fig. 1c); Detection of the extralobar lung sequestration tissue (Fig. 1c);
Volumetric visualizing the aorta and abnormal supply vessel (it is possible only on a series with intravenous contrast), automatic or semi-automatic calculation of the diameter and length of the abnormal supply vessel (Fig. 1d).
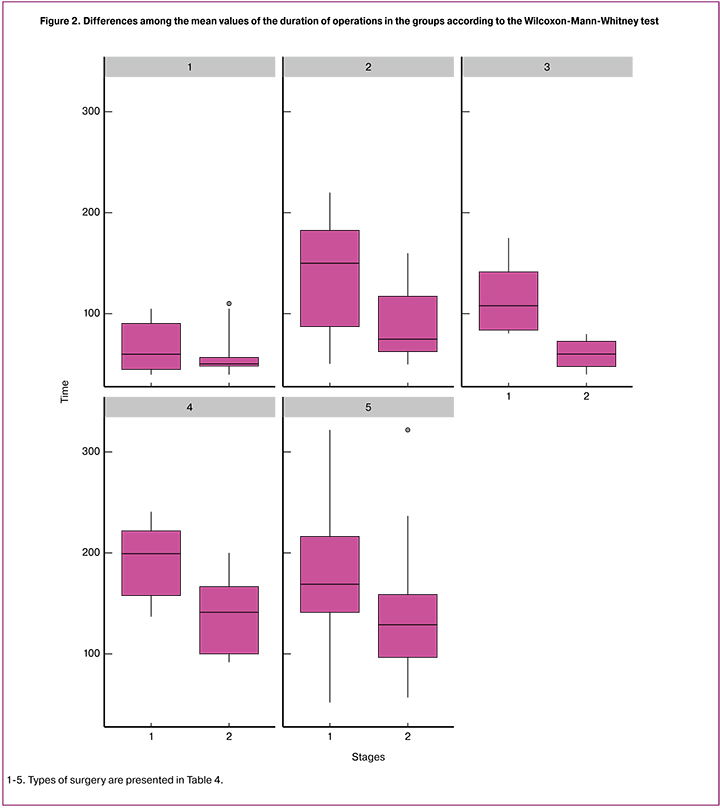
At all stages of segmentation, the data on automatic calculation of the volumes of normal and pathological lung areas were obtained. According to the developed algorithms, all the accumulated series were segmented. The 3D models were used for the preparation to operate on a child by changing their position in the space on the monitor, by comparing the patient’s fixed anatomical structures and indicating areas of increased risk for intraoperative complications and potential technical difficulties. The extent of surgical care was based on the characteristics and nature of lung malformation, as well as capabilities of modern medical technologies aimed at reducing the invasiveness of surgery. Upon confirmation of CCAM, a large intralobar lung sequester as well as their combination, lobectomy of the affected lung lobe was performed; extralobar BLS was removed with a reliable ligation of the supply vessel; intralobar BLS with a small area of fusion with the lung lobe was removed with careful aerostasis of healthy lung tissue at the border. All operations were performed by thoracoscopic access using 3-mm optical system and working tools. There was a comparative analysis of the average duration of the main types of operations for the lung malformations (Table 4) as well as anatomical features that determine the technical difficulties and intraoperative complications in patients before the introduction of the preoperative data analysis system (stage I) and after its introduction (stage II). The Wilcoxon-Mann-Whitney test was used to assess the significance of differences between the mean values of the operations duration in the group (Fig. 2).
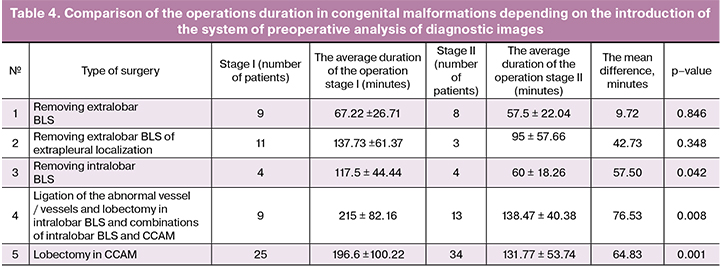
As can be seen from Table 4 and Figure 2, the reduction in the average duration of the operation was observed in all types of operations, however, when removing extralobar lung sequesters (operations 1 and 2), the time difference compared to the variance in the groups was small, so the differences between the averages were insignificant. In contrast, the differences were significant in the removal of intralobar BLS and operations associated with lobectomy due to the greater difference in mean and smaller variance. This is due to the fact that extralobar BLS in any localization has no connection with the lung; supply vessels in most cases are available for examination and the duration of the intervention is determined by the number of supply vessels and the anatomical version of their location. The duration of operations associated with the separation of pathological and healthy lung tissue, as well as lobectomy, is due to various features of anatomy of the affected lung. These features include the dense fusion of pathological tissue with healthy lung tissue of other lung lobes, abnormal incomplete separation of lung lobes, lack of access to large vessels of the affected lung lobe and the presence of additional abnormal supply vessels of the circulatory system. In connection with these features one patient from the retrospective group had to be installed an additional thoracoport to retain the pathological lobe of the lung, and another patient had conversion performed due to severe bleeding.
Conclusion
This study has shown that we accumulated a significant amount of clinical and diagnostic information; its standardization and computer analysis allowed us to optimize the stage of surgeon’s preparation for a complex endoscopic surgery. The construction of virtual 3D models of the patient’s chest organs in the preoperative period allows surgeons to plan effectively the repair of the anatomical variant of the lung structure in malformation, which is important in preparing a doctor for surgery. It also improves a surgeon’s spatial navigation during the operation; it reduces the duration of surgery and decreases the risk of intraoperative complications and technical difficulties.
The formed bank of reference diagnostic images is used to fill libraries of expert diagnostic artificial neural network (self-learning computer expert system) and to create reference virtual 3D models. The expert diagnostic system, in turn, is supplemented by unified descriptions of the radiation studies, as well as a wide range of clinical data specific to this congenital malformation of the lung. Structured visual diagnostic, clinical and phenotypic features included in the libraries of the computer expert system compose the basis for the subsequent creation of a data model, which is also necessary for the implementation of remote patient counseling and training programs for young specialists.
References
1. Исаков Ю.Ф., Володин Н.Н., Гераськин А.В., ред. Неонатальная хирургия. М.: Династия; 2011. 680с. [Isakov Yu.F., Volodin N.N., Geraskin A.V., ed. Neonatal surgery. M .: Dynasty; 2011. 680 p. (in Russian)]
2. Разумовский А.Ю., Мокрушина О.Г. Эндохирургические операции у новорожденных. М.: МИА; 2015. 344с. [Razumovsky A.Yu., Mokrushina O.G. Endosurgical operations in newborns. M .: MIA; 2015. 344 p. (in Russian)]
3. Polites S.F., Habermann E.B., Zarroug A.E., Thomsen K.M., Potter D.D. Thoracoscopic Vs open resection of congenital cystic lung disease- utilization and outcomes in 1120 children in the United States. J. Pediatr. Surg. 2016; 51(7): 1101-5.
4. Tack P., Victor J., Gemmel P., Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed. Eng. Online. 2016; 15: 115.
5. Lebedev G., Gureeva A., Tikhonova Y. Software system for dynamic athlete health monitoring. Procedia Computer Science. 2017; 112: 1664-9.
6. Lebedev G., Tikhonova Y. Information system for pharmacotherapy method selection. Procedia Computer Science. 2017; 112: 1658-63.
Received 07.09.2018
Accepted 21.09.2018
About the Authors
Dorofeeva, Elena I., PhD, Clinical Chief of Neonatal Surgery Department, Federal State Budget Institution “National Medical Research Center for Obstetrics,Gynecology and Perinatology” Ministry of Healthcare of the Russian Federation.
117997, Russia, Moscow, Oparina str. 4. Tel.: +74954381424. E-mail: dorofey_i@mail.ru
Podyrovskaya, Yulia L., PhD, Head of Neonatal Surgery Department, Federal State Budget Institution “National Medical Research Center for Obstetrics, Gynecology and Perinatology” Ministry of Healthcare of the Russian Federation. 117997, Russia, Moscow, Oparina str. 4. Tel.: +74954381424. E-mail: y_podurovskaya@oparina4.ru
Tumanova, Uliana N., PhD, researcher at the Laboratory of Morphology, Federal State Budget Institution “National Medical Research Center for Obstetrics, Gynecology
and Perinatology” Ministry of Healthcare of the Russian Federation. 117997, Russia, Moscow, Oparina str. 4. Tel.: +79057285905. E-mail: u.n.tumanova@gmail.com
Nemkovskyi, Gleb B., head of IT solutions implementation Department «Vesttreid Ltd».
115201, Russia, Moscow, 1-st Warshawsky pr. 1A/9. Tel.: +79636230862. E-mail: gbn.fun@gmail.com
Balashov, Ivan S., junior researcher at the Laboratory of Bioinformatics. Federal State Budget Institution “National Medical Research Center for Obstetrics, Gynecology
and Perinatology” Ministry of Healthcare of the Russian Federation. 117997, Russia, Moscow, Oparina str. 4. Tel.: +79104462005. E-mail: i_balashov@oparina4.ru
Prokhin, Alexey V., analyst of «Vesttreid Ltd». 115201, Russia, Moscow, 1-st Warshawsky pr. 1A/9. Tel.: +7 9160733881. E-mail: aleksprohin@gmail.com
Bychenko, Vladimir G., head of the Department of Radiation Diagnostics. Federal State Budget Institution “National Medical Research Center for Obstetrics, Gynecology
and Perinatology” Ministry of Healthcare of the Russian Federation. 117997, Russia, Moscow, Oparina str. 4. E-mail: v_bychenko@oparina4.ru
Degtyarev, Dmitry N., MD, professor, Deputy of Director on Researches, Federal State Budget Institution “National Medical Research Center for Obstetrics, Gynecology
and Perinatology” Ministry of Healthcare of the Russian Federation. 117997, Russia, Moscow, Oparina str. 4. Tel.: +79260072630. E-mail: glav_neolog@yahoo.com
For citations: Dorofeeva E.I., Podyrovskaya Yu.L., Tumanova U.N., Nemkovskyi G.B., Balashov I.S., Prokhin A.V., Bychenko V.G., Degtyarev D.N. The computer-assisted clinical and diagnostic data analysis system for planning an optimal surgical intervention in newborns with lung malformations. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (12): 117-24. (in Russian)
http://dx.doi.org/10.18565/aig.2018.12.117-124



