The role of minimally invasive intrauterine interventions in increasing the effectiveness 0of IVF programs
Objective. To determine intrauterine pathologies in infertile women preparing for IVF and to evaluate the significance of minimally invasive intrauterine interventions in relation to the effectiveness of subsequent IVF programs.Kozachenko I.F., Arakelyan A.S., Smolnikova V.Yu., Adamyan L.V.
Materials and methods. Hysteroscopy and morphological examination of the endometrium were performed in 600 infertile patients of reproductive age. The analysis of clinical data and the results of restoration of reproductive function were conducted in 351 patients, who were divided into the following groups: group 1 (n=140) included patients with chronic endometritis, group 2 (n=116) consisted of women with endometrial hyperplastic processes, group 3 (n=95) included patients with intrauterine pathology (fibroids, septum, synechiae, adenomyosis).
Results. Normal morphological structure of the endometrium was detected in 36% of the examined patients, benign endometrial pathology in 42.7%, atypical hyperplasia and endometrial cancer in 5.5%, and intrauterine pathology in 15.9% of patients. The average duration of infertility was 5.8 (0.6) years. All patients had a history of intrauterine interventions: one intrauterine intervention was in 27.8%, two intrauterine interventions were in 46.6%, and three or more intrauterine interventions were in 25.6% of cases. The results of restoration of reproductive function were evaluated within one year after undergoing complex treatment of assisted reproductive technology (ART) cycles. Pregnancy occurred in 62% of women. Pregnancy resulted in childbirth in 51% of cases.
Conclusion. Intrauterine pathology was observed in 58.5% of infertile women. Surgical and subsequent conservative treatment of intrauterine pathology contributed to a reduction in pregnancy losses, as well as an increase in the frequency of pregnancies that ended in childbirth. The risk factors for repeated ART failures in patients with intrauterine pathology are the maternal age over 35 years, the presence of chronic salpingoophoritis, endometriosis and chronic endometritis, as well as the previous history of three or more different intrauterine interventions.
Keywords
Among patients of reproductive age, there has recently been a growing trend for changing their reproductive behavior and choosing a later age for childbearing. Such a trend leads to an increase in the frequency of various gynecological pathologies in this category of patients [1].
In Russia, the share of infertile couples ranges from 8 to 17.5%, and uterine factor accounts for half of all infertility factors [2].
Pathological processes affecting the uterus as a target organ are known to be based on a number of etiological factors: infectious factor leading to the development of chronic endometritis, which is most common in tubal- peritoneal infertility; dishormonal factor associated with the development of hyperplastic processes in endocrine infertility, uterine fibroids and endometriosis; combined factors leading to the formation of polyps and intrauterine synechiae [3]. However, the cause-and-effect relationships of the impact of uterine fibroids, endometrial polyps, chronic endometritis and a number of other diseases on fertility are not sufficiently defined. Various intrauterine pathologies are observed in 25% of infertile patients [4]. In recent years, hysteroscopy has been recommended after two or more unsuccessful IVF attempts. Endometrial polyps, chronic endometritis, intrauterine septum, intrauterine synechiae, and submucous uterine fibroids are detected during hysteroscopy; they are not detected by other examination methods prior to hysteroscopy [5, 6]. Timely or inaccurately diagnosed diseases of the uterine cavity are detected in patients with repeated unsuccessful programs of assisted reproductive technologies (ART) with a rate ranging from 18 to 50% [4, 6].
A number of studies indicate that routine hysteroscopy is not appropriate to confirm the presence of intrauterine pathology [7]. At the same time, other studies have demonstrated the need for hysteroscopy and surgical intrauterine manipulations as effective ways to overcome infertility in cases of submucous uterine myoma, endometrial polyps, and uterine septum [8–10]. Thus, there was an increased frequency of pregnancies using IVF after removal of polyps up to 51%, after removal of submucous uterine fibroids frequency of pregnancies increased up to 63%, after dissection of synechiae it rose up to 51% [4, 11, 12].
The aim of the study was to determine intrauterine pathologies in infertile women preparing for IVF and to evaluate the significance of minimally invasive intrauterine interventions in relation to the effectiveness of subsequent IVF programs.
Materials and Methods
The study included 600 patients planning to achieve conception using the IVF program. For this purpose, all patients attended V.I. Kulakov National Medical Research Centre for Obstetrics, Gynecology and Perinatology, B.V. Leonov Department of Assisted Reproductive Technologies in the Treatment of Infertility in Moscow, Russia. Prior to IVF program, all patients underwent clinical and laboratory examination in accordance with the order of the Russian Ministry of Health No. 107n «On approval of the use of assisted reproductive technologies, contraindications and restrictions to their use» dated 30.09.2012. All patients met the inclusion criteria (age from 18 to 40 years, normal ovarian reserve, presence of intrauterine pathology, two or more ineffective previous IVF attempts, informed consent to participate in the study).
All patients were performed therapeutic and diagnostic hysteroscopy in the Gynecological Department on day 5–8 of the menstrual cycle; subsequent morphological examination of the endometrium was carried out in the 1st Pathology Department.
In all cases, hysteroscopy was performed under intravenous anesthesia according to the standard procedure using rigid diagnostic hysteroscopes Hopkins II (Karl Storz GmbH & Co., Germany) with an external diameter of 5 mm. The uterine cavity was examined when it was filled with a sterile saline solution of sodium chloride. The solution was supplied using Hamou Endomat infusion pump (Karl Storz GmbH & Co., Germany). Hysteroscopy in all patients was combined with diagnostic endometrial scraping and subsequent histological examination of the smears. Hysteroresectoscope Karl Storz with an outer diameter of 8 mm, an adjustable viewing direction of 00 to 120, and a monopolar current of 60 W in cutting mode was used for resectoscopy. The expansion medium was a 5% glucose solution, which provided optimal conditions for good visualization and had dielectric properties.
During histological examination, macropreparation was fixed for 24 hours in 10% neutral buffered formalin solution; the samples were subsequently embedded in paraffin according to the generally accepted method. Sections 5 mm thick prepared on rotary microtomes were stained with hematoxylin-eosin. The obtained preparations were examined under a Nikon Eclipse 50i light microscope at magnifications of x50 to x400 using a digital camera OLIMPUSE 501.
The analysis of clinical characteristics, anamnestic data and results of the IVF program after hysteroscopy was performed in 351 patients (excluding patients with atypical hyperplasia and endometrial cancer), who were divided into three groups. Group 1 (n=140) included patients with chronic endometritis, group 2 (n=116) consisted of patients with endometrial hyperplastic processes, and group 3 (n=95) consisted of patients with intrauterine pathology (fibroids, septum, synechiae, adenomyosis).
The patients included in the study were treated for infertility using the IVF protocol (IVF+ICSI) with controlled ovarian stimulation and transfer of embryos to the uterine cavity, or in a cycle with transfer of previously cryopreserved embryos to the uterine cavity (cryoprotocol). The IVF program was performed according to the standard protocol with gonadotropin-releasing hormone antagonists. Ovarian stimulation was performed with recombinant follicle stimulating hormone. The trigger of ovulation was injected if the leading follicle was greater than or equal to 17 mm. Human chorionic gonadotropin was used for ovulation triggering. One good quality blastocyst (according to the classification of D. Gardner and W.B. Schoolcraft) was transferred on the 5th day after performing the transvaginal puncture of the ovary. If the level of human chorionic gonadotropin in the blood serum increased in 14 days after embryo transfer to the uterine cavity, biological pregnancy was registered; visualization of gestation sac in the uterine cavity in 21 days after embryo transfer was evidence of clinical pregnancy.
Statistical analysis of the obtained data was performed using MS Office Excel and Statistica 10.0 software (USA). The Kolmogorov-Smirnov criterion was used to determine the normality of the distribution. The data with a normal distribution were presented as the average value (standard deviation), the data were compared using the Student’s t-test. Nominal data were described with absolute and percentage values. The nominal data were compared using the χ2 criterion. The differences were considered statistically significant at the level of p<0.05.
Results
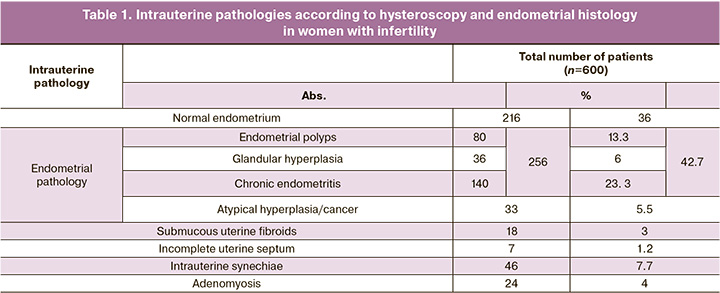
According to the histological study (Table 1), 36% of the examined women had a normal morphological structure of the endometrium, 42.7% of patients had a benign endometrial pathology, including 23.3% of cases of chronic endometritis, 18.3% of cases of endometrial hyperplastic processes: endometrial polyps and/or glandular hyperplasia (GH); 5.5% of women had atypical hyperplasia and endometrial cancer. Intrauterine pathology was detected in 15.9% (type 0 and I submucous uterine fibroids up to 1.5 cm, incomplete uterine septum occupying less than 1/3 of the uterine cavity, stage I–II synechiae, stage I–II focal or diffuse adenomyosis).
We conducted a comprehensive analysis of clinical characteristics, anamnestic data and treatment results in 351 patients with various intrauterine pathologies.
The average age was 32.0 (0.7) years, and it did not differ statistically in the groups: group 1 – 32.5 (0.7) years, group 2 – 31.4 (0.8) years, and group 3 – 32.1 (0.65) years. It should be noted that 58% of the patients were aged 30 years or older.
All the patients complained of infertility, and this was the only complaint in 22% of the patients. Changes in the character of menstruation were noted by most patients (41%): scanty menstruation or shortening of menstruation to 1–3 days was observed in 10% of patients, heavy menstruation was observed in 31% of patients. Painful menstruation was noted by 12% of women, pain in the lower abdomen not associated with menstruation was noted by 17% of patients, dyspareunia was noted by 14.1% of patients. Patients’ complaints in different groups were not statistically significant.
The groups did not show any differences in the incidence of previous and concomitant diseases.
On average, menarche occurred at 12.7 (0.2) years. The duration of the menstrual cycle is 29.2 (0.6) days, the duration of menstruation is 5.2 (0.1) days. The duration of menstruation less than 3 days was noted by 10% of patients, heavy menstruation was observed in 31% of women, and painful menstruation was noted by 12% of patients.
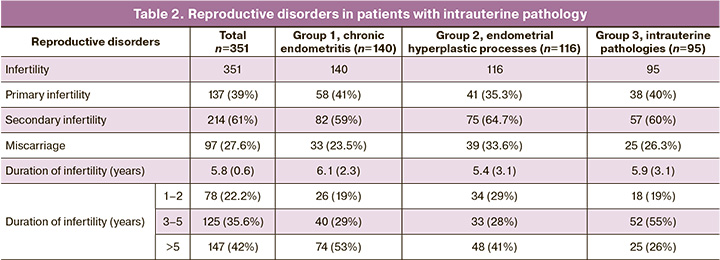
All patients included in the study had reproductive disorders (Table 2). The analysis of the data presented in Table 2 revealed a predominance of the incidence of secondary infertility (61%). Miscarriage at different gestational age was noted in the history of 27.6% of patients. The average duration of infertility was 5.8 (0.6) years, and 147 (42%) women had reproductive disorders for more than 5 years, more than half of them had chronic endometritis (53%).
Among 214 patients with secondary infertility, previous pregnancies resulted in artificial abortions in 15.2% of cases, ectopic pregnancies in 6.1% of cases, and there was a high percentage of spontaneous pregnancy losses at various stages (50.5%). Only 22% of pregnancies ended in childbirth. It should be noted that complications after abortion or childbirth were noted in 37.6% of women: endometritis (after abortion or childbirth) was observed in 23% of women, postpartum bleeding (manual examination, postpartum curettage) was noted in 14.2% of patients.
More than half of the patients (210 out of 351, which was 59.8%) had previously been treated for infertility using assisted reproductive technology (ART), which was ineffective. Only 18.8% of patients had one unsuccessful attempt of ART, while the remaining patients (41%) had two or more previous unsuccessful attempts. The average number of ART attempts was 2.9 (0.8), unsuccessful attempts 2.2 (0.5). It is worth noting that 35% of patients had losses of pregnancies following the ART program.
The analysis of data on sexually transmitted infections (STIs) and non-specific inflammatory diseases of the vagina showed that only about a third of the patients had no history of STIs. The presence of STIs was noted in 63% of women, and the most common were chlamydia (17.9%) and ureaplasmosis (24%).
Most of the patients (62%) had chronic salpingoophoritis.
External genital endometriosis was noted in 27.9% of patients, mainly stages I-II were revealed (12.5%).
Endometrial hyperplastic processes were in the history of 77.8% of patients, the greater number of these patients were in group 2. At the same time, some patients (14%) had both polyps and endometrial hyperplasia.
Uterine fibroids were detected in 132 (37.6%) women, but when this study was conducted, there were no indications for additional surgical interventions (small intramural or subserous uterine fibroids).
The analysis of the past gynecological operations, especially intrauterine interventions, was of critical importance in our opinion. Various surgeries on the reproductive organs were performed in 58.1% of women, and most of the patients underwent several surgeries which were performed using different approaches (168 patients out of 204, which was 82%). The main indications for surgery were infertility (tuboperitoneal factor), external genital endometriosis, uterine fibroids, ovarian cysts, intrauterine septum, intrauterine synechiae, ovarian cysts and hyperplastic processes of the endometrium and endocervix, as well as abortive pregnancy.
A total of 1,127 gynecological operations were performed: endoscopic (laparoscopic or hysteroscopic) approaches were used in 63.6% of cases, laparotomy was performed in 12.9% of cases, and intrauterine interventions without hysteroscopy were performed in 23.6%.
It should be noted that all patients (n=351) had a previous history of intrauterine interventions (the total number is 625): one intrauterine intervention was performed in 27.8% of cases, two intrauterine interventions were performed in 46.6%, and three or more intrauterine interventions were performed in 25.6% of cases. That is, most of intrauterine interventions (72.2%) were repeated, the average number of intrauterine interventions in the patient’s history was 2.5 (0.4).
All 351 patients underwent surgical treatment, its extent depended on the type of intrauterine pathology (Table 3).
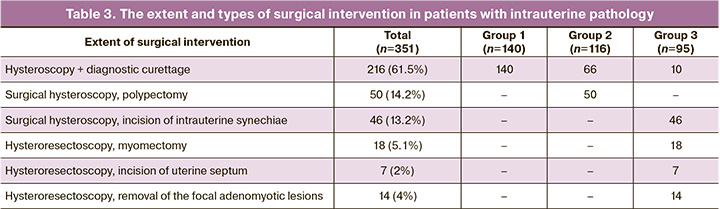
Hysteroscopy and diagnostic curettage/endometrial biopsy were performed in 61.5% of patients, surgical hysteroscopy or hysteroresectoscopy was performed in 38.5% of women. There were no complications during or after surgery.
In the postoperative period, patients underwent rehabilitation treatment depending on the detected intrauterine pathology. All patients received antibiotic preventive treatment during the operation and in the early postoperative period. Patients with endometrial hyperplasia received hormone therapy for 3–6 months (gestagens). Patients after hysteroresectoscopy and myomectomy were prescribed antibiotic preventive treatment in combination with early physiotherapy. Patients with chronic endometritis received cyclic antibiotic therapy in combination with delayed physiotherapy (3 months). Cyclic hormone therapy with delayed physiotherapy was prescribed to patients with intrauterine synechiae. In the presence of adenomyosis, therapy with agonist gonadotropin releasing hormone (3 months) was administered in combination with early physiotherapy.
At the end of the course of treatment, a control ultrasound assessment was performed on day 5–7 of the menstrual cycle.
The results of restoration of reproductive function were evaluated within one year after prescribing the complex treatment and using ART programs. The patients included in the study were treated for infertility using IVF program with ovarian function stimulation and transfer of native embryos to the uterine cavity or cryoprotocol. Embryo transfer in the stimulation cycle was made in 217 (62%) of 351 patients, in cryoprotocol – in 134 (38%).
Pregnancy occurred in 178 patients out of 351, which was 50.7%: in group 1, pregnancy occurred in 40.7%, in group 2 it was in 48.3%, and in group 3 it was in 68% of patients. Ectopic pregnancy was observed in 7.3% of patients. Childbirth resulted from 53.3% of pregnancies. Pregnancy losses were noted in 39.3% of cases. Caesarean section was the mode of delivery in 72% of cases, spontaneous delivery occurred in 28% of cases. Pregnancy outcomes in patients of different groups are shown in Table 4.
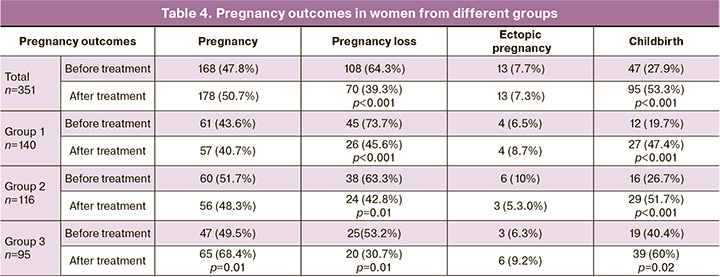
The analysis of pregnancy outcomes in patients with intrauterine pathology after treatment showed a statistically significant difference in the rate of pregnancy loss before and after treatment: there was a 1.5-fold decrease in the rate of pregnancy loss among 351 patients included in the study (64.3% and 39.3%, respectively, p<0.001) and a statistically significant 2-fold increase in the rate of childbirth compared to the same indicator before treatment (27.9% and 53.3%, respectively, p<0.001).
Thus, surgical and subsequent restorative treatment of intrauterine pathology in infertile patients contributed to a decrease in the rate of losses of pregnancy following the IVF program, and an increase in the rate of pregnancies that ended in childbirth.
Of particular interest, is the assessment of clinical characteristics, anamnestic data, and treatment results in a group of patients with two or more previous unsuccessful ART attempts, as well as the identification of risk factors for recurrent failures. According to our study, two or more unsuccessful ART attempts were noted in 41% of patients (144 out of 351). We considered it appropriate to divide these patients retrospectively into two groups depending on the results of the IVF program after surgical treatment. Group A included 87 patients who were not pregnant after ART program, and group B included 57 women who became pregnant after undergoing ART program; the pregnancy was confirmed by ultrasound.
The patients included in the study received infertility treatment in the IVF protocol (IVF+ICSI) with controlled ovarian stimulation and transfer of embryos to the uterine cavity, or in a cycle with transfer of cryopreserved embryos to the uterine cavity (cryoprotocol). IVF protocol (IVF+ICSI) was used in 57.4% of patients in group A and 52% of patients in group B; treatment with cryopreserved embryos was received by 43.7% of patients in group A and 47.4% of patients in group B.
The average age of women in group A was 34.4 (3.9) years, and average age of women in group B was 32.1 (4.7) years (p<0.001). When comparing groups A and B, there was a statistically significantly higher number of patients aged 35 years and older in the group of women with unsuccessful ART attempts after surgical treatment (56% and 31.6%, respectively, p<0.001).
There were no differences in the quantitative and qualitative characteristics of the menstrual cycle in the patients of the study groups: the age of menarche was 12.7 (1.2) years, the average duration of the menstrual cycle was 28.8 (0.8) days, and the duration of menstruation was 4.22 (1.2) days.
There were no statistically significant differences in the indicators of reproductive function in the patients of the study groups. There was only a statistically significant predominance of the share of women with primary infertility in the group with unsuccessful subsequent ART program (49% and 32%, respectively, p=0.02).
Patients with recurrent failures of IVF had a high prevalence of gynecological diseases. STIs and pelvic inflammatory diseases were more frequently diagnosed in patients with recurrent failures in IVF programs (52% and 66.6%). External genital endometriosis was the third most common gynecological disease in the examined patients (46.5%). There was a statistically significant predominance of the share of patients with chronic salpingoophoritis (73.6% and 36%, respectively, p<0.001) and endometriosis (53% and 36.8%, respectively, p=0.02) among patients in group A compared to patients in group B.
When a patient started receiving current ART treatment, each of them had a history of one or more intrauterine interventions that were performed for diagnostic or therapeutic purposes. There was a statistically significant predominance of the share of patients with previous three or more intrauterine interventions in group with unsuccessful IVF attempts (64.4% and 46%, respectively, p=0.01), as well as the average number of intrauterine interventions [3.05 (0.36) and 2.66 (0.26)], p<0.001). Therefore, the increase in the number (three or more) of different intrauterine interventions in the patient’s history increases the probability of repeated unsuccessful ART attempts.
Previous pelvic surgeries were noted in 64.12% of the patients, and did not differ in the groups.
The duration of infertility in the patients included in the study at the time of treatment averaged 5.04 (0.4) years for patients in group A and 5.25 (0.52) years for patients in group B. The pregnancy rate after IVF programs was 5.5% per one procedure for embryo transfer (5.38% for patients in group A and 5.71% for patients in group B), but none of the pregnancies resulted in childbirth.
According to the history of somatic diseases and surgical interventions, there were no differences among the patients.
When preparing for ART, all patients with previous IVF failures underwent hysteroscopy and endometrial biopsy. Chronic endometritis was detected in 25% of women, uterine fibroids – in 17.4%, endometrial hyperplasia – in 13.9%, endometrial polyps – in 31%, intrauterine synechiae – in 19.4%, adenomyosis – in 16%, uterine malformation (incomplete uterine septum) – in 4.2% of women. There was a statistically significant predominance of the number of patients with chronic endometritis detected during hysteroscopy and endometrial biopsy in group A compared to group B (32.2% and 14%, respectively, p=0.006).
Thus, various intrauterine pathologies that required hysteroscopic assessment and treatment were observed in 58.5% of infertile women. Surgical and subsequent restorative treatment of intrauterine pathology in infertile patients contributed to a decrease in the rate of loss of pregnancy following the IVF treatment, and an increase in the rate of pregnancies that ended in childbirth.
According to our study, two or more unsuccessful ART attempts were observed in 41% of patients. Factors associated with a high probability of repeated unsuccessful ART attempts in patients with intrauterine pathology are:
- age of women receiving ART treatment over 35 years;
- chronic salpingoophoritis, external genital endometritis, and chronic endometritis;
- a previous history of three or more different intrauterine interventions.
Discussion
The analysis of the detected intrauterine pathologies in infertile women preparing for IVF treatment showed a predominance of chronic endometritis, which was noted in 23.3% of cases, intrauterine pathology (submucous fibroids, intrauterine septum, synechiae and adenomyosis) revealed in 15.9% of patients, and endometrial polyps noted in 13.3% of cases. Our findings are consistent with the results of previous studies, which also confirmed the high rate of detection of various intrauterine and endometrial pathologies in infertile patients [12–16].
Hysteroscopy has a higher sensitivity and specificity in detecting intrauterine pathologies in comparison with transvaginal ultrasound. Moreover, the undeniable advantage of hysteroscopy is its ability not only to diagnose various intrauterine pathologies, but also to perform their treatment simultaneously (the «see-and-treat» principle). Our study confirmed an increase in the pregnancy rate after hysteroscopy in IVF cycles, since hysteroscopy (diagnostic and/or operative) and subsequent restorative treatment of intrauterine pathology contributed to a 1.5-fold decrease in the rate of pregnancy loss and an increase in the rate of pregnancies that ended in childbirth. The results of our study are consistent with the data provided in the meta-analysis of A. Di Spiezio Sardo et al. [15] and data from large foreign randomized controlled trials [17, 18]. In our opinion, hysteroscopy should be included in the examination of patients with infertility, especially of patients with previous unsuccessful IVF attempts. Thus, intrauterine pathology can be timely diagnosed and eliminated, and the effectiveness of infertility treatment can be improved.
Conclusion
Thus, pathological changes in the endometrium and various intrauterine pathologies can be detected due to hysteroscopic assessment of the uterine cavity, as well as histological and immunohistochemical studies of the endometrium; if necessary, surgical treatment can be performed. All these methods can increase pregnancy rate when using ART programs.
References
- Абубакиров А.Н., Адамян Л.В., Андреева Е.Н., Аншина М.Б., Веюкова М.А., Гависова А.А., Гзгзян А.М., Гусев Д.В., Долгушина Н.В., Исакова Э.В., Калинина Е.А., Калинина Е.А., Калугина А.С., Коган И.Ю., Кодылева Т.А., Козаченко И.Ф., Колода Ю.А., Корнеев И.А., Корнеева И.Е., Корсак В.С. и др. Женское бесплодие (современные подходы к диагностике и лечению). Клинические рекомендации (протокол лечения). Москва; 2019. [Abubakirov A.N., Adamyan L.V., Andreeva E.N., Anshina M.B., Veyukova M.A., Gavisova A.A., Gzgzyan A.M., Gusev D.V., Dolgushina N.V., Isakova E.V., Kalinina E.A., Kalinina E.A., Kalugina A.S., Kogan I.Yu., Kodyleva T.A., Kozachenko I.F., Koloda Yu.A., Korneev I.A., Korneeva I.E., Korsak V.S. et al. Female infertility (modern approaches to diagnosis and treatment). Clinical recommendations (treatment protocol). Moscow; 2019. (in Russian)].
- Сухих Г.Т., Назаренко Т.А. Бесплодный брак. Современные подходы к диагностике и лечению: руководство. М.: ГЭОТАР-Медиа; 2010; 21-52. [Sukhikh G.T., Nazarenko T.A. Infertile marriage. Current approaches to diagnosis and treatment: guidance. Moscow: GEOTAR-Media; 2010; 21-52. (in Russian)].
- Дюжева Е.В., Коган Е.А., Калинина Е.А., Кузьмичев Л.Н. Принципы индивидуальной гормональной подготовки эндометрия у пациенток с неэффективными попытками ЭКО. Акушерство и гинекология. 2011; 7(2):39-45. [Dyuzheva E.V., Kogan E.A., Kalinina E.A., Kuzmichev L.N. The principles of individual hormonal preparation of the endometrium in patients with ineffective attempts at IVF. Obstetrics and gynecology. 2011;7(2):39-45. (in Russian)].
- Fatemi H.M., Kasius J.C., Timmermans A. et al. Prevalence of unsuspected uterine cavity abnormalities diagnosed by office hysteroscopy prior to in vitro fertilization. Hum. Reprod. 2010;25:1959-65. https://doi.org/10.1093/humrep/deq150.
- Bosteels J., Weyers S., Puttemans P., Panayotidis C., Van Herendael B., Gomel V., Mol B.W.J., Mathieu C., D’Hooghe T. The effectiveness of hysteroscopy in improving pregnancy rates in subfertile women without other gynaecological symptoms: a systematic review. Human Reproduction Update. 2010;16 (1):1-11. https://doi.org/10.1093/humupd/dmp033.
- Parry J.P., Isaacson K.B. Hysteroscopy and why macroscopic uterine factors matter for fertility. Fertil Steril. 2019;112(2):203-10. https://doi.org/10.1016/j.fertnstert.2019.06.031.
- Cao H., You D., Yuan M., Xi M. Hysteroscopy after repeated implantation failure of assisted reproductive technology: A meta-analysis. J Obstet Gynaecol Res. 2018;44(3):365-73. https://doi.org/10.1111/jog.13571.
- Jayakrishnan K., Menon V., Nambiar D. Submucous fibroids and infertility: Effect of hysteroscopic myomectomy and factors influencing outcome. J Hum Reprod Sci. 2013;6:35-9. https://doi.org/10.4103/0974-1208.112379.
- Makled A.K., Farghali M.M., Shenouda D.S. Role of hysteroscopy and endometrial biopsy in women with unexplained infertility. Arch Gynecol Obstet. 2014; 289:187-92. https://doi.org/10.1007/s00404-013-2931-8.
- Bakas P., Hassiakos D., Grigoriadis C., Vlahos N., Liapis A., Gregoriou O. The role of hysteroscopy prior to assisted reproductive techniques. J Minim Invasive Gynecol. 2013; 1553- 4650. https://doi.org/10.1016/j.jmig.2013.07.023.
- Bettocchi S., Achilarre M.T., Ceci O., Luigi S. Fertility-enhancing hysteroscopic surgery. Semin Reprod Med. 2011;29(2):75-82. https://doi.org/10.1055/s-0031-1272469.
- Хириева П.М., Адамян Л.В. Клинико-анамнестические данные и исходы лечения женщин с внутриматочными синехиями. Проблемы репродукции. 2017;23(6):39-44. [Кhirieva P.M., Adamyan L.V. Clinical, anamnestic data and treatment results in women with intrauterine adhesions. Problems of Reproduction. 2017;23(6):39-44. (in Russian)]. https://doi.org/10.17116/repro201723639-44.
- Локшин В.Н., Валиев Р.К., Карибаева Ш.К., Карибаева К.Д., Сатбаева Э.Б., Соколенко Е.Г., Абдикаримова Р.Б., Лежебокова Э.А. Внутриматочная патология у пациенток с бесплодием. Проблемы репродукции. 2018;24(4):28-32. [Lokshin V.N., Valiyev R.K., Karibayeva Sh.K., Karibayeva K.D., Satbayeva E.B., Sokolenko Е.G., Abdikarimova R.B., Lezhebokova E.A. Intrauterine pathology in patients with infertility. Problems of Reproduction. 2018;24(4):28-32. (in Russian)]. https://doi.org/10.17116/repro20182404128.
- Bosteels J., van Wessel S., Weyers S. et al. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev. 2018;12(12):CD009461. Published 2018 Dec 5. https://doi.org/10.1002/14651858.cd009461.pub3.
- Di Spiezio S.A., Carlo C.D., Minozzi S. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and metaanalysis. Hum Reprod Update. 2016; 22(4):479-96. https://doi.org/10.1093/humupd/dmw008.
- Cela V., Litta P., Franchini M. et al. Fertility-enhancing hysteroscopic surgery. Minerva Ginecol. 2016;68(2):167-74.
- Pundir J., Pundir V., Omanwa K. Hysteroscopy prior to the first IVF cycle: a systematic review and metaanalysis. Reprod Biomed Online. 2014; 28(2):151-61. https://doi.org/10.1016/j.rbmo.2013.09.025.
- Smit J.G., Torrance T., Broekmans F.J. Hysteroscopy prior to a first IVF treatment cycle: the need for well-performed RCT. Reprod Biomed Online. 2014; 29(1):1-42. https://doi.org/10.1517/14712598.7.9.1311.
Received 08.09.2020
Accepted 14.09.2020
About the Authors
Irena F. Kozachenko, Ph. D., leading researcher of the Gynecological Department, V.I. Kulakov National Medical Research Center of Obstetrics,Gynecology and Perinatology, Ministry of Healthcare of Russia. E-mail: i_kozachenko@oparina4.ru. ORCID: 0000-0003-1822-9164.
117997, Russia, Moscow, Ac. Oparin str., 4.
Alek S. Arakelyan, Ph. D., doctor of the Gynecological Department, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology,
Ministry of Healthcare of Russia. E-mail: A_arakelyan@oparina4.ru. ORCID: 0000-0003-3655-7938. 117997, Russia, Moscow, Ac. Oparin str., 4.
Veronika Yu. Smolnikova, MD, leading researcher of the Department of assisted reproductive technologies in infertility treatment, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of Russia. E-mail: v_smolnikova@ oparina4.ru. ORCID: 0000-0002-8025-4849.
117997, Russia, Moscow, Ac. Oparin str., 4.
Leila V. Adamyan, MD, Professor, academician of the Russian Academy of Sciences, Head of the Gynecological Department, Deputy Scientific Director, V.I. Kulakov
National Medical Research Center of Obstetrics, Gynecology and Perinatologyr, Ministry of Healthcare of Russia.
E-mail: Adamyanleila@gmail.com. ORCID: 0000-0002-3253-4512. 117997, Russia, Moscow, Ac. Oparin str., 4.
For citation: Kozachenko I.F., Arakelyan A.S., Smolnikova V.Yu., Adamyan L.V. The role of minimally invasive intrauterine interventions in increasing the effectiveness of IVF programs.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 9: 97-104 (in Russian).
https://dx.doi.org/10.18565/aig.2020.9.97-104