Prediction of the efficiency of surgical treatment for infertility in women with minor forms of genital endometriosis – from theory to practice
Objective. To identify immunological criteria for predicting the onset of spontaneous pregnancy after laparoscopy in women of active reproductive age with infertility and minor forms of genital endometriosis.Krasilnikova A.K., Malyshkina A.I., Sotnikova N.Yu., Abdullaeva L.Kh.
Subjects and methods. Peripheral venous blood samples were examined in 264 women of active reproductive age with infertility and minor forms of genital endometriosis. The levels of B-lymphocytes (CD20+), B1 cells (CD20+CD5+), CD86+ neutrophils, and IL-1β+ monocytes were measured by flow cytometry and the content of sRAGE was determined by ELISA.
Results. The women who got pregnant within a year after laparoscopy had differences in immunological parameters from those who did not. Pregnancy occurred in women who showed decreased values of CD20+, CD20+CD5+ lymphocytes, and CD86+ neutrophils and increased levels of IL-1β+ monocytes in the blood, while patients who had high blood serum sRAGE levels prior to treatment failed to get pregnant within one year after laparoscopy. ROC analysis of immunological parameters in order to use the latter in the future for predicting pregnancy after surgical treatment established that parameters, such as the peripheral blood levels of CD20+ lymphocytes and sRAGE had a low predictive value and sensitivity. Whereas the indicators of B-1 lymphocyte (CD20+CD5+), IL-1β+ monocyte, and CD86+ neutrophils levels were highly sensitive and specific; these indicators may suggest that humoral immunity is stimulated, and there are systemic inflammatory reactions and phagocyte hyperactivation. These processes can determine the mechanisms of the development of infertility in minor forms of genital endometriosis.
Conclusion. Thus, the triad of indicators: the levels of B-1 lymphocytes, IL-1β+ monocytes, and CD86+ neutrophils are pathogenetically significant predictors of the efficiency of surgical treatment for infertility in patients of active reproductive age with minor forms of genital endometriosis at the preoperative stage.
Keywords
Currently, endometriosis is still a relevant issue, since it significantly worsens quality of women’s life, necessitates surgical intervention leading to complications and functional impairment of adjacent organs, pronounced adhesion process, reduction of ovarian follicle reserve, and, as a result – the impairment of reproductive function in young women.
If in the presence of stage III–IV genital endometriosis infertility usually develops due to adhesions, follicle depletion, then the causes of infertility in women of active reproductive age in case of stage I–II of genital endometriosis, in the absence of pronounced anatomical changes, still remain unclear. It is assumed that infertility in patients with stage I–II endometriosis is associated with impaired folliculogenesis, implantation, endometrial abnormalities, luteal phase defects, as well as the changes in immune microenvironment in the peritoneal cavity. Clinical observations also support the hypothesis of relationship between "small" forms of endometriosis and impaired fertility [1].
Women with infertility due to genital endometriosis have to apply to medical centers to undergo various programs of assisted reproductive technologies (ART), including intrauterine insemination and IVF. However, many researchers note relatively low efficacy of these techniques, including in the presence of "small" forms of genital endometriosis of [2–5]. Some studies found no differences in IVF outcomes in women with infertility associated with "small" forms of genital endometriosis and infertility of unknown etiology. [6]. There is an opinion that diagnostic and therapeutic laparoscopy, which includes excision of endometrial foci of endometrioid heterotopies increases the effectiveness of infertility treatment in patients with “small forms” of genital endometriosis. In addition, it allows to establish the stage of the disease and helps to determine the subsequent treatment. However, until present, no approaches to effective management of these patients in the postoperative period have been developed, since there are no reliable laboratory predictors of successful surgical treatment that would help choosing the optimal management tactics. The issue has to be addressed, for whom it should be recommended to continue planning natural pregnancy within 1 year after therapeutic and diagnostic laparoscopy, and for whom – to make a choice in favor of IVF and abandon wait-and-see strategy. This would improve the chances of conception without losing valuable time. Considering the high cost of ART, the impact of hormones on the woman's body, it would be advisable to predict in advance the probability of pregnancy in such patients.
According to clinical recommendations on endometriosis (L.V. Adamyan et al., 2016), endometriosis fertility index (EFI) developed by G. Adamson (2010) is the first validated scoring system that has a predictive value for pregnancy. EFI score is calculated taking into account the woman's age, duration of infertility, obstetric history and data obtained during diagnostic laparoscopy (the state of the fallopian tubes, ovary, the prevalence of endometriosis according to the AFS endometriosis classification), while each sign is assessed using the 0–4 scale, and as a result, the total score is determined, which may vary from 0 to 10. In patients with an EFI score of 0, pregnancy occurrence is predicted within 1–3 years after excision of endometriotic lesions in 10% of cases, and with an EFI score of 10, pregnancy is predicted one year after surgery in 56% of cases, after 2 years – in 72%, after 3 years – in 75% [7]. According to EFI, the expected pregnancy rate within 1, 2 and 3 years after laparoscopy increases in proportion to the increase of the index itself [7]. However, according to the results reported by the authors/developers, the forecast accuracy is relatively low. So, even with the maximum scores of 9–10 points, the pregnancy rate within 12 months after excision of the lesions does not exceed 56%, since many of the used signs are assessed by the doctor subjectively. This reduces the diagnostic significance of the index, and the index calculation requires long time periods. Therefore, in women with infertility and “small" forms of genital endometriosis, it is necessary to carry out additional examination for a more effective prognosis. In our opinion, a woman’s immune system analysis is of great interest and according to publications, it is one of the important mechanisms underlying the development of endometriosis. [8].
Numerous studies in this field showed that the changes in adaptive immune responses manifested by an increase in the activity of autoimmune reactions with the production of autoantibodies have negative effect at various stages of reproductive processes. [9, 10]. In addition, in patients with endometriosis, the disorders in systemic reactions of innate immunity were found, leading to the development of local and systemic inflammatory responses, which determine the increased production of pro-inflammatory cytokines and have a negative effect on fertility in women with endometriosis [11]. Therefore, the indicators of activation of the humoral and innate immune responses may serve as effective predictors of reproductive function restoration in patients with endometriosis. However, it is very important to select among a variety of existing immune indicators and systematize the specific immune system malfunctions, which have the predictive value, and can be directly associated with infertility due to genital endometriosis, in particular, "small" forms. This fact can serve as a "point of application" for the development of preoperative prognostic criteria for assessment of pregnancy rates and management strategies in the early postoperative period depending on the obtained indicators. Thus, the development and implementation of such prognostic criteria into practice was the objective of our study.
The aim of the study was to identify a number of prognostic immunological criteria for predicting spontaneous pregnancy after surgical treatment in women with infertility and stage I – II endometriosis.
Materials and methods
The study included 264 patients aged 18–45 years with infertility and stage I–II endometriosis. During laparoscopy performed in the Endoscopy Department at V.N. Gorodkov Ivanovo Research Institute of Maternity and Childhood of the Ministry of Health of the Russian Federation, stage I–II genital endometriosis (ASF classification) was found in all women, and excision and destruction of endometriotic lesions was perfomed.
After surgery the women were followed-up for one year with purpose of assessment of surgical interventions. Venous blood taken from the cubital vein was examined before and 2 months after women had laparoscopic surgery.
The total level of B-lymphocytes (CD20+), B1-cells (CD20+ CD5+), CD86+ neutrophils, IL-1β+ monocytes was assessed with the use of monoclonal antibodies (Beckman Coulter, USA). and flow cytometry with BD FACSCanto II cytometer (Becton Dickinson, USA). The results were processed using CellQuest Pro software (Becton Dickinson, USA). Before evaluation of intracellular cytokine production by lymphocytes, the cell membrane was fixed and permeabilized with the use of FIX & PERM cell permeabilization kit (CALTAG Laboratories, Burlingame, CA, USA). Also, serum level of the soluble form of the receptor for advanced glycation end-products (sRAGE) was assessed by using ELISA kits (Quantikine R&D Systems, USA).
Statistical analysis
Mathematical and statistical data processing was carried out using licensed software package Microsoft Office 2013, Statistica for Windows 12.0, StatSoftInc. Normality of sampling distribution was determined by Shapiro–Wilk test and Kolmogorov–Smirnov test. Fisher’s test was used to compare the equality of variances in comparison groups. Student's t-test and Mann–Whitney U-test was used to compare the laboratory results between the groups (statistically significant differences were at p<0.05). When comparing these groups before and after treatment, Student's t-test and Wilcoxon test was used for the paired samples. In the tables, the data are shown as median (Me), first quartile (Q1), third quartile (Q3), mean (M) and standard deviation (SD).
Results
The average age of the women participating in the study was 29 (27; 32) years. According to the test results in conformity with the Order № 572 of the Ministry of Health of Russia dated November 12, 2012, there were no abnormalities in hormone profile, and the women had adequate ovarian follicular pool. The average duration of infertility was 3 (2; 5) years. Almost the same rate was for primary (57.6%) and secondary (42.3%) infertility. In addition to infertility, 28.4% of women had abnormal uterine bleeding (AUB) in the form of heavy bleeding and prolonged spotting before and after a menstrual period, 55.7% of women complained of dysmenorrhea, 12.5% of them had dyspareunia, 2.3% of women were with dyschezia, in 11.3% of women recurrence of genital endometriosis was noted.
For each woman in the study group, the EFI score was calculated. It reached 8.61 (0.27) points. The spontaneous pregnancy rate was 28.7% within 1 year. However, according to the EFI scoring system, spontaneous pregnancy rate in this category of women should have been 45%. This confirmed once again that predictive accuracy was not high, as was mentioned by the authors of the scoring system. Considering the results of researches of the immune mechanisms in genital endometriosis and associated infertility, which were obtained in our laboratory for the last 20 years [11], we focused on the most prognostically significant indicators of humoral and innate immunity: the total number of B-lymphocytes (CD20+), B1-cells (CD20+CD5+), CD86+ neutrophils, IL-1β+ monocytes, and serum levels of sRAGE.
It was found, that women who conceived within 1 year after laparoscopy had different immunological parameters compared to the patients who could not conceive. Pregnancy occurred in women who were characterized by decreased values of CD20+, CD20+CD5+ lymphocytes, CD86+ neutrophils and increased serum levels of IL-1β+ monocytes (Tables 1, 2). And the patients with high serum levels of sRAGE before treatment failed to conceive within 1 year after laparoscopy (Table 2).
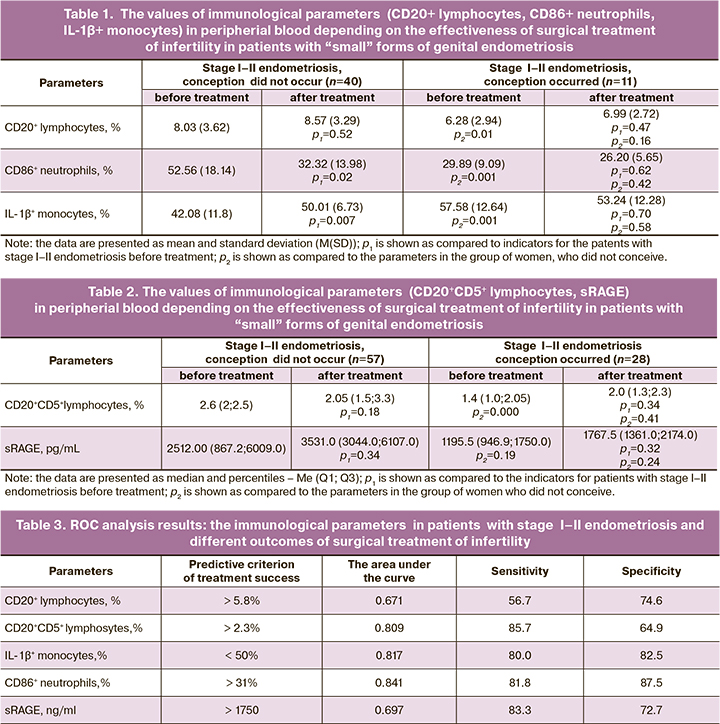
ROC analysis of the immunological parameters was carried out with the aim of their future use in prediction of conceiving after surgical treatment. The data characterizing the area under the curve, as well as sensitivity and specificity of the estimated parameters are presented in Table 3 and Figures 1–3.
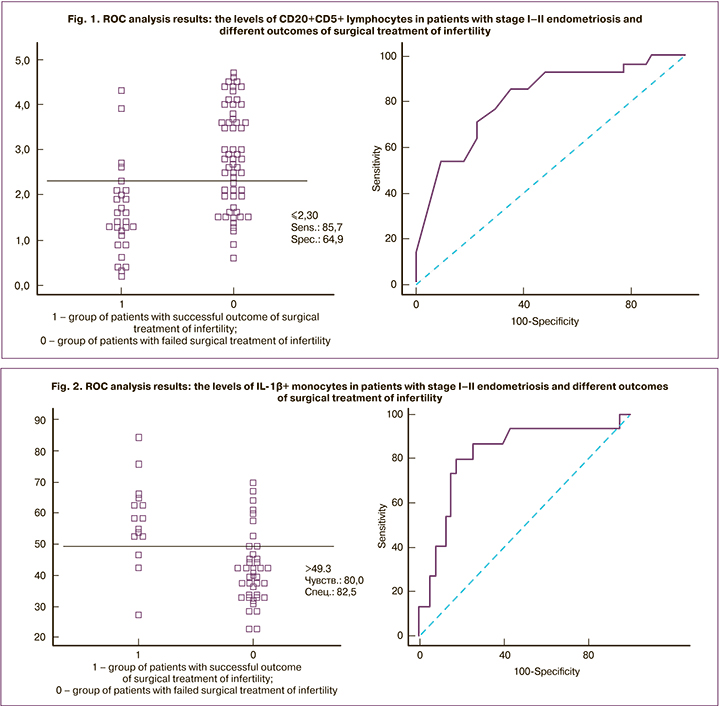
As can be seen from this Table, such parameters as the levels of CD20+ lymphocytes and sRAGE in the peripheral blood have low predictive value and rather low sensitivity (56.7%). However, the levels of B1-lymphocytes (CD20+CD5+), which are among the main autoantibody-producing cells, IL-1β+ monocytes and CD86+ neutrophils, indicating the presence of systemic inflammatory responses and hyperactivation of phagocytes, have high sensitivity and specificity.
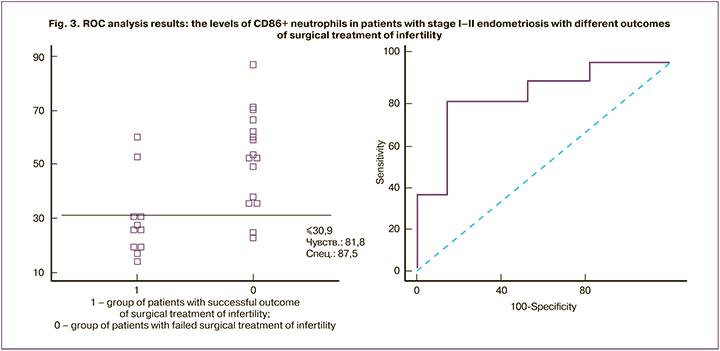
According to ROC analysis results, the prognostic threshold of 2.3% was chosen for the level of CD20+CD5+ lymphocytes (Patent No. 2291439 dated 10.01.2007), for CD86+ neutrophils – 31% (Patent No. 2613313 dated 15.03.2017) and for IL-1+ monocytes – 50% (Patent No.2557923 dated 30.06.2015). This triad of indicators formed the basis for predicting the effectiveness of surgical treatment of infertility in patients of active reproductive age with "small" forms of genital endometriosis at the preoperative stage.
The success of surgical treatment of genital endometriosis and spontaneous pregnancy within a year after laparoscopy was predicted, when in patients before laparoscopy the relative value of CD20+CD5+ lymphocytes was equal to or less than 2.3%, CD86+ neutrophils – equal to or less than 31% and IL-1+ monocytes – equal to or more than 50%. On the contrary, in case of deviation of at least one indicator from the prognostic values, the lack of success of surgical treatment of genital endometriosis and infertility was predicted with accuracy of 79.2%.
Discussion
The obtained data showed an increase in serum levels of sRAGE. This may serve as a marker of increased inflammatory response in "small" forms of genital endometriosis and infertility. [10]. It was proven that the adaptive immunity was activated in such patients, as indicated by an increase in the level of neutrophils expressing the costimulatory molecules CD86, which induce the development of T-helper Type 2 cells and the immune response with an increase in the intensity of humoral responses. Accordingly, the increased levels of B1-lymphocytes were due to an increase in autoantibodies production [12].
It is known that the interleukin-1β system plays an important role in regulation of the reproductive processes, in particular in ensuring endometrial receptivity [13], contributes to successful conception [14], including in patients participating in the IVF program [15]. Decreased intracellular production of IL-1β by blood monocytes in women with infertility associated with stage I–II of genital endometriosis may be the cause of impaired implantation processes [11]. Currently, it is believed that the main immunological components of genital endometriosis: increased systemic production of pro-inflammatory cytokines, abnormal monocyte function, activation of B-lymphocytes with excessive autoantibodies production are aimed at supporting chronic inflammation. These changes can directly affect fertility due to endometriosis. [11].
Conclusion
The success of surgical treatment aimed at restoring reproductive function in patients with "small" forms of genital endometriosis largely depends on baseline immune status.
The triad of indicators of the levels of B1-lymphocytes, IL-1β+ monocytes and CD86+ neutrophils in the peripheral blood makes it possible even at the preoperative stage to predict within 1 year the effectiveness of surgical treatment of infertility in patients of active reproductive age with this pathology.
Timely prediction of the effectiveness of surgical treatment based on immunological criteria allow choosing optimal management tactics for such patients without losing valuable time.
References
- Broi M.G.D., Ferriani R.A., Navarro P.A. Ethiopathogenic mechanisms of endometriosis-related infertility. JBRA Assist. Reprod. 2019; 23(3): 273-80. https://dx.doi.org/10.5935/1518-0557.20190029.
- Rizk B., Turki R., Lotfy H., Ranganathan S., Zahed H., Freeman A.R. et al. Surgery for endometriosis-associated infertility: do we exaggerate the magnitude of effect? Facts Views Vs. Obgyn. 2015; 7(2): 109-18.
- Leung A.S., Dahan M.H. Should we diagnose and treat minimal and mild endometriosis before medically assisted reproduction? Minerva Ginecol. 2016; 68(2): 211-8.
- Tanbo T., Fedorcsak P. Endometriosis-associated infertility: aspects of pathophysiological mechanisms and treatment options. Acta Obstet. Gynecol. Scand. 2017; 96(6): 659-67. https://dx.doi.org/10.1111/aogs.13082.
- Ekine A.A., Fülöp I., Tekse I., Rúcz Á., Jeges S., Koppán Á., Koppán M. The surgical benefit of hysterolaparoscopy in endometriosis-related infertility: a single centre retrospective study with a minimum 2-year follow-up. J. Clin. Med. 2020; 9(2): 507. https://dx.doi.org/10.3390/jcm9020507.
- Xing W., Lin H., Wu Z., Li Y., Zhang Q. Effect of pelvic endometriosis, endometriomas and recurrent endometriomas on ivf-et/icsi outcomes. Mater. Sociomed. 2016; 28(2): 91-4. https://dx.doi.org/10.5455/msm.2016.28.91-94.
- Adamson G.D., Pasta D.J. Endometriosis fertility index: the new, validated endometriosis staging system. Fertil. Steril. 2010; 94(5): 1609-15. https://dx.doi.org/10.1016/j.fertnstert.2009.09.035.
- Kokcu A. Possible effects of endometriosis-related immune events on reproductive function. Arch. Gynecol. Obstet. 2013; 287(6): 1225-33. https://dx.doi.org/10.1007/s00404-013-2767-2.
- Красильникова А.К., Малышкина А.И., Сотникова Н.Ю., Анциферова Ю.С. Прогнозирование эффективности хирургического лечения бесплодия у женщин с малыми формами наружного генитального эндометриоза. Акушерство и гинекология. 2013; 7: 36-9. [Krasilnikova A.K., Malyshkina A.I., Sotnikova N.Yu., Antsiferova Yu.S. Predicting the effectiveness of surgical treatment of infertility in women with small forms of external genital endometriosis. Obstetrics and gynecology. 2013; 7:36-9.(in Russian)].
- Riccio L.G.C., Baracat E.C., Chapron C., Batteux F., Abrao M.S. The role of the B lymphocytes in endometriosis: a systematic review. J. Reprod. Immunol. 2017; 123: 29-34. https://dx.doi.org/10.1016/j.jri.2017.09.001.
- Сотникова Н.Ю., Анциферова Ю.С., Малышкина А.И., Красильникова А.К. Нарушения системных реакций врожденного иммунитета у пациенток с бесплодием и эндометриозом I–II стадии и возможность их коррекции препаратом Ликопид. Иммунология. 2016; 37(1): 17-21. [Sotnikova N.Yu., Antsiferova Yu.S., Malyshkina A.I., Krasilnikova A.K. Violations of systemic reactions of innate immunity in patients with infertility and endometriosis of stage I–II and the possibility of their correction with Lycopid. Immunology. 2016; 37(1): 17-21. (in Russian)].
- Kageyama Y., Katayama N. Ontogeny of human B1 cells. Int. J. Hematol. 2020; 111(5): 628-33. https://dx.doi.org/10.1007/s12185-019-02775-y.
- Bulletti C., Flamigni C., de Ziegler D. Implantation markers and endometriosis. Reprod. Biomed. Online. 2005; 11(4): 464-8. https://dx.doi.org/10.1016/s1472-6483(10)61142-x.
- Geisert R., Fazleabas A., Lucy M., Mathew D. Interaction of the conceptus and endometrium to establish pregnancy in mammals: role of interleukin 1β. Cell Tissue Res. 2012; 349(3): 825-38. https://dx.doi.org/10.1007/s00441-012-1356-1.
- Bonetti T.C., Salomao R., Brunialti M., Braga D.P., Borges E. Jr., Silva I.D. Cytokine and hormonal profile in serum samples of patients undergoing controlled ovarian stimulation: interleukin-1beta predicts ongoing pregnancy. Hum. Reprod. 2010; 25(8): 2101-6. https://dx.doi.org/10.1093/humrep/deq171.
Received 07.10.2020
Accepted 02.11.2020
About the Authors
Angelina K. Krasilnikova, MD, senior researcher of the department of obstetrics and gynecology, V.N. Gorodkov Ivanovo Research Institute of Maternity and Childhood, Ministry of Health of Russia. Tel.: +7(920)345-68-09. E-mail: brasilia71@mail.ru. ORCID: 0000-0001-7839-3893.153045, Russia, Ivanovo, Pobedy str., 20.
Anna I. Malyshkina, MD, professor, director of V.N. Gorodkov Ivanovo Research Institute of Maternity and Childhood, Ministry of Health of Russia. Tel.: +7(910)982-24-19. E-mail: anna_im@mail.ru. ORCID: 0000-0002-1145-0563. 153045, Russia, Ivanovo, Pobedy str., 20.
Natalia Yu. Sotnikova, MD, professor, Head of the Department of clinical immunology, V.N. Gorodkov Ivanovo Research Institute of Maternity and Childhood,
Ministry of Health of Russia. Tel.: +7(906)619-36-53. E-mail: niimid.immune@mail.ru. ORCID: 0000-0002-0608-0692.
153045, Russia, Ivanovo, Pobedy str., 20.
Leyla Kh. Abdullaeva, PhD, assistant of the department of obstetrics and gynecology, neonatology, anesthesiology and reanimatology, V.N. Gorodkov Ivanovo Research Institute of Maternity and Childhood, Ministry of Health of Russia. Tel.: +7(920)343-64-11. E-mail: leyla.abdullaeva.88@mail.ru. ORCID: 0000-0001-9730-3355.
153045, Russia, Ivanovo, Pobedy str., 20.
For citation: Krasilnikova A.K., Malyshkina A.I., Sotnikova N.Yu., Abdullaeva L.Kh. Prediction of the efficiency of surgical treatment for infertility in women with minor forms of genital endometriosis – from theory to practice.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2020; 11: 100-106 (in Russian).
https://dx.doi.org/10.18565/aig.2020.11.100-106



