Одной из важнейших проблем современного акушерства является профилактика осложненного течения беременности и репродуктивных потерь [1, 2].
По данным современных литературных источников, встречаемость аномалий расположения плаценты (АРП) в 1-м триместре беременности высока и составляет не менее 30,0%, ко времени родоразрешения частота предлежания плаценты значительно уменьшается и составляет 1,04% [3, 4]. Частота преждевременных родов в группе пациенток с АРП по разным данным варьирует от 38,0 до 82,0% [5–7].
Причины формирования АРП в настоящее время до конца не изучены. Выделены факторы риска массивного кровотечения при предлежании плаценты – полное предлежание плаценты, ранее перенесенные операции кесарева сечения, консервативные миомэктомии, крупный вес новорожденного [8–12].
Значительные различия в локализации плаценты в 1-м триместре и к сроку родов объясняются феноменом «миграции плаценты», который заключается в смещении плаценты вверх ввиду формирования нижнего сегмента матки путем прироста мышц и растяжения этой области [4]. Ряд авторов указывают на более «благоприятную» миграцию плаценты при локализации ее по передней стенке, а также при коррекции истмико-цервикальной недостаточности шейки матки акушерским пессарием или швом [13, 14].
Однако в литературе отсутствуют данные о функциональном состоянии плаценты в процессе ее миграции, механизме воздействия пессария на плаценту и шейку матки; достаточно дискутабельным остается вопрос об эффективности пессария при ведении беременных с предлежанием плаценты. В связи с этим наше исследование было направлено на оценку эффективности различных подходов к ведению беременных с АРП с целью снижения репродуктивных потерь.
Цель исследования: оценить эффективность применения акушерского пессария в сочетании с прогестероном в группе беременных высокого риска по невынашиванию с предлежанием плаценты.
Материал и методы исследования
Исследование проводилось на базе Омского перинатального центра БУЗОО Областная клиническая больница, с ежегодным количеством родов более 3500. Процент преждевременных родов в центре за последние три года (2014–16 гг.) стабильный – 8,0% (848/10607), количество родов с предлежанием плаценты – 1,7% (178/10607).
Под нашим наблюдением находилось 217 беременных группы высокого риска по развитию преждевременных родов с предлежанием плаценты. Пациентки были разделены на 2 группы. В основную группу (A, n=81) включены беременные, которым применялся комплексный подход с установкой акушерского пессария доктора Арабин в сочетании с микронизированным прогестероном; группу сравнения (B, n=136) составили пациентки, получавшие только микронизированный прогестерон. На первом этапе исследования в зависимости от вида предлежания плаценты были сформированы группы IA1 (n=13), IB1 (n=50) – с полным предлежанием плаценты, IA2 (n=25), IB2 (n=37) – с неполным предлежанием плаценты и IA3 (n=43), IB3 (n=49) – с низкой плацентацией (расстояние от внутреннего зева до края плаценты не более 3 см).
На втором этапе исследования для оценки роли акушерского пессария и прогестерона в феномене «миграции плаценты» из числа обследованных была выделена группа пациенток (II, n=61), из которых группа IIА (n=29) получала комбинированное лечение (акушерский пессарий и прогестерон), а группа IIВ (n=31) – только вагинальный прогестерон. Пациенткам данных групп проводилось динамическое ультразвуковое исследование (УЗИ) с определением индекса Пурсело в аркуатных артериях в области плацентации, а также измерение переднего маточно-цервикального угла в сроках 18–20 недель (до постановки пессария доктора Арабин), 23–24 недели и 32–33 недели (на фоне пессария); в группе IIВ данные исследования проводились в эти же сроки. Результатом исследования в данной группе (II) являлась регистрация миграции плаценты. В зависимости от полученного результата, пациентки были разделены на 2 подгруппы: IIА1 – группа беременных с комбинированным подходом ведения беременности и с зарегистрированной миграцией плаценты (n=20); IIВ1 – группа беременных, получавших только прогестерон, с зарегистрированной миграцией плаценты (n=21); IIА2 – группа беременных с комбинированным подходом ведения беременности, без миграции плаценты (n=9); и IIВ2 – группа беременных, получавших только прогестерон и без миграции плаценты (n=11).
Группы были сопоставимы по возрасту, анамнезу, паритету, гинекологической и соматической заболеваемости.
Во время исследования проводили оценку анамнеза, данных общепринятых лабораторных показателей, УЗИ. УЗИ выполнялось на аппарате «VolusonТМЕ8/Е8 Expert», при этом оценивалось состояние шейки матки, плода, измерялся передний маточно-цервикальный угол (образованный передней стенкой нижнего сегмента матки и осью цервикального канала), регистрировался индекс Пурсело в аркуатных артериях. За нормальное значение принимали показатель IR не более 0,75±0,03 [15]. Степень миграции плаценты в группах отслеживали в динамике в сроках 24, 28 и 32 недели с помощью УЗИ и допплерометрии. Объем кровопотери во время родов и в послеродовом периоде оценивался гравиметрическим методом.
Всем беременным основной группы вводили перфорированные силиконовые пессарии доктора Арабин. Пессарий был установлен беременным в следующих сроках: 11–15 недель – в 18,5% (15/81) случаев; 16–18 недель – в 50,6% (41/81); 19–22 недели – в 30,9% (25/81).
Перед введением акушерского пессария обязательно оценивали биоценоз влагалища беременной. С целью профилактики развития бактериального вагиноза всем беременным назначали вагинальные таблетки с аскорбиновой кислотой (по 250 мг 1 раз в неделю).
Во всех группах исследования с 7 недель беременности пациентки получали микронизированный прогестерон вагинально в суточной дозе 200 мг/сут до 32 недели беременности.
Статистическая обработка данных проводилась с применением интегральной системы для комплексного статистического анализа и обработки данных Statistica 10.0. Критический уровень значимости при проверке статистических гипотез принимался равным 0,05. Сравнение относительных величин проводили с помощью точного критерия Фишера или критерия χ2 с поправкой Йетса.
Результаты исследования
Большинство женщин находилось в среднем репродуктивном возрасте – 31,4±5,3 года. Анализ паритета показал, что среди женщин с предлежанием плаценты преобладали повторнородящие – 53,4% (116/217). Первобеременные составили 15,2% (33/217), повторнобеременные первородящие – 31,4% (68/217). Все пациентки, включенные в исследование, имели отягощенный акушерский и/или гинекологический анамнез. При этом бесплодие в анамнезе отмечено в 30,4% (66/217) случаев, миома матки больших размеров выявлена у 13,4% (29/217) беременных, самопроизвольные прерывания беременности во втором триместре в анамнезе отмечались у 12,4% (27/217) женщин. Преждевременные роды в анамнезе в исследуемой группе имели место у 16,6% (36/217), воспалительные заболевания женских половых органов – у 29,4% (64/217), рубец на матке от предыдущих оперативных вмешательств – у 23,5% (51/217).
Анализ осложнений течения беременности показал отсутствие значимых различий в исследуемых группах по частоте возникновения угрозы прерывания, плацентарных нарушений, преэклампсии и внутриутробной инфекции. Однако гемодинамические нарушения в плаценте в группе В диагностировали в 34,5% случаев (47/136), что на 12,3% выше по сравнению с группой А – 22,20% (18/81) (χ2=1,637, p=0,201). Процент пациенток с внутриутробным инфицированием плода практически не различался – 23,4% (19/81) и 23,50% (32/136) в группах А и В соответственно (χ2=0,023; p=0,880). Выявлены статистически значимые различия такого осложнения, как кровотечение во время беременности в исследуемых группах пациенток с предлежанием плаценты: 11,1% (9/81) и 33,1% (45/136) в группах А и В соответственно (χ2=7,416; p=0,006).
В структуре аномалий расположения плаценты наиболее часто встречалось низкое расположение плаценты – от 36,0% (49/136) в группе B до 53,2% (43/81) в группе A. Нами не выявлено значимых различий в исследуемых группах по частоте таких осложнений, как преждевременное излитие околоплодных вод и аномалии родовой деятельности. Их частота составила: преждевременное излитие околоплодных вод – 13,5% (11/81) в группе А и 16,1% (22/136) – в группе В (χ2=0,062; p=0,8023), аномалии родовой деятельности – 11,1% (9/81) и 10,3% (14/136) (χ2=0,003; p=0,955) соответственно. Однако выявлены статистически значимые различия по частоте возникновения кровотечений в родах в исследуемых группах: 22,2% (18/81) у рожениц группы А и у 72,0% (98/136) группы В (χ2=16,183; p=0,001). При этом массивные кровотечения более 1000 мл отмечены в 3 случаях (3/18) у пациенток основной и в 18 (18/98) – у пациенток группы сравнения; кровотечения более 1500 мл встречались только в группе В (13/98).
Выявлены значимые различия по причинам возникновения данных осложнений: так плацента accretа встречалась в 2,5% (2/81) случаев у пациенток основной группы, тогда как в группе сравнения – у 14,7% (20/136) (χ2=5,835; p=0,016), плацента increta – в 8,6% (7/81) и в 19,9% (27/136) соответственно (χ2=2,920; p=0,088), гипотонические кровотечения в родах или интраоперационно – у 4,9% и у 20,6% (28/136) соответственно (χ2=6,581; p=0,010).
Динамическое наблюдение за расположением плаценты во время беременности позволило выявить различную частоту миграции плаценты в исследуемых группах. Так, в группе с использованием пессариев доктора Арабин (А) миграция плаценты отмечена в 48,1% (39/81) случаев, тогда как в группе пациенток, получавших только прогестерон (В) – лишь у 26,4% (36/136) (χ2=4,369; p=0,037). Благодаря полученному результату (уменьшение доли пациенток с предлежанием плаценты) частота оперативных родов в группе А была существенно снижена и составила 51,8% (42/81) против 86% (117/136) – в группе B (χ2 = 4,461; p=0,034).
Беременность закончилась срочными родами у 77,8% (63/81) пациенток группы А и у 63,3% (86/136) группы В. Частота преждевременных родов была выше среднестатистической в популяции и составила 31,3% (68/217), из них: 22,2% (18/81) – в группе с использованием пессариев и 36,7% (50/136) – в группе беременных, получавших только прогестерон (χ2=2,234; p=0,135). Преждевременные роды в сроке 22–28 недели зарегистрированы у 1,4% (3/217) пациенток, из них в одном случае в группе А и в 2 случаях – в группе В. Выявлены значимые различия по частоте преждевременных родов при сроке гестации до 34 недель: так в группе А частота преждевременных родов составила 8,6% (7/81), тогда как в группе В данный показатель был значительно выше – 23,5% (32/136) (χ2=4,678; p=0,031). Частота преждевременных родов со сроком гестации после 34 недель не имела статистической разницы и составила 13,6% (11/81) и 13,2% (18/136) в группах соответственно (χ2=0,02; p=0,888).
Выявлены статистически значимые различия по частоте таких осложнений, как: кровотечения во время беременности в подгруппах IА2 и IВ2 – 8% (2/25) и 48,6% (18/37) соответственно (χ2=4,998; p=0,025), кровотечения в родах в подгруппах IА3 и IВ3 – 18,6% (8/43) и 67,3% (33/49) соответственно (χ2=7,778; p=0,005).
Наиболее высокая частота оперативных родов отмечена в подгруппах IВ1 – 94% (47/50), IВ2 – 86,5% (32/37) и IА2 – 80,0% (20/25). Выявлена различная частота миграции плаценты – значимые различия были только в подгруппах IА3 и IВ3 – в 65,1% (28/43) и 20,4% (10/49) случаях соответственно (χ2=6,827, p=0,009). В подгруппах с полным предлежанием плаценты (IА1 и IВ1) частота миграции плаценты была невысокой (23,1 и 22,0% соответственно).
На втором этапе исследования (II группа) получены следующие данные: в большинстве случаев (57/61) средние значения индекса резистентности (IR) в аркуатных артериях в исследуемых группах находились в пределах референсных значений (<75±0,03). Однако удалось выявить значимые различия данных показателей в группах с миграцией плаценты IIА1 и IIВ1 (средние значения IR в сроке 32–33 недели составили 0,53±0,04 и 0,63±0,06 в группах соответственно (р=0,001), а также в группах IIА1 и IIА2 и IIА1 и IIВ2. Наибольший размах по величине IR определен в группах IIА1 и IIВ2: 0,53±0,04 и 0,69±0,14 соответственно (р=0,001).
Данные по измерению индекса Пурсело в аркуатных артериях представлены в таблице.
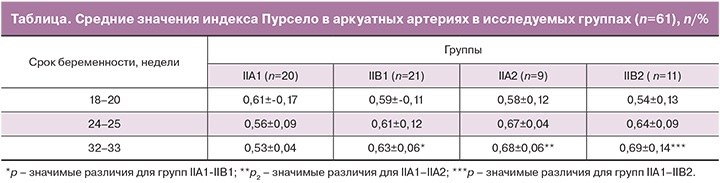
При анализе полученных данных выявлена закономерность: так, в группе с использованием пессариев с последующей миграцией плаценты отмечен градиент снижения IR к 32-й неделе (к низкорезистентному кровотоку), тогда как в группе без миграции плаценты отмечалось увеличение IR с тенденцией к высокорезистентному кровотоку. Патологический кровоток (IR в аркуатных артериях >0,75±0,03) зарегистрирован в 6,5 % случаев (4/61) в группах без миграции плаценты, из них в 3 случаях – группе IIВ2, в одном случае – в группе IIА2. При этом у пациенток с высоким индексом Пурсело в 100% случаев были зарегистрированы гемодинамические нарушения в плаценте, преждевременное созревание плаценты, патология околоплодных вод (маловодие, многоводие). Также в сроке 24 недели в группах без миграции (IIА2 и IIВ2) венозные кровотоки регистрировались в 50% случаев: (4/9) – в группе IIА2 и (6/11) – в группе IIВ2.
Анализ изменения переднего маточно-цервикального угла в течение беременности выявил: исходно у пациенток исследуемых групп в сроке 18–20 недель отмечались «тупые» углы в 68,8% (42/61), «острые» – в 31,62% (19/61).
Среднее значение переднего маточно-цервикального угла в группах IIА1 и IIА2 в сроке 20 недель (перед введением пессария) составило 106,3±10,8°, в сроке 32–33 недели (на фоне пессария) произошло изменение угла в сторону «более тупого» до 113,7±10,7° (изменение на 7,4°). В то время как в группах IIВ1 и IIВ2 значительного изменения угла не произошло: 108,1±11,9° (в 20 недель) и 107,9±10,4° (в 32–33 недели).
Срочные роды в подгруппах II группы (n=61) зарегистрированы у 85,3% (52/61) пациенток, преждевременные роды – у 14,7% (9/61), из них в подгруппах с пессарием – у 33,3% (3/9), в подгруппах без пессария – у 66,7% (6/9) (χ2=0,694; p=0,405). Преждевременных родов в сроке 22–27 недели зарегистрировано не было, преждевременные роды 28–34 недели были отмечены у 22,2% (2/9) пациенток в подгруппах без коррекции шейки матки. Среднее значение переднего маточно-цервикального угла у женщин с преждевременными родами по нашим данным составило 94,2±10,4°. В 31,0% (9/29) случаев под действием пессария доктора Арабин произошло изменение исходно «острого» угла (среднее значение 85,7±9,6°) в сторону «тупого» (среднее значение 113,4±3,7°) и беременность закончилась срочными родами (свыше 37 недель).
Обсуждение результатов
Комплексный подход к решению данной проблемы позволил снизить частоту кровотечений во время беременности на 22% в основной группе по сравнению с группой В (11,1% против 33,1% соответственно) (χ2=7,416; p=0,006). Однако анализ акушерских кровотечений в подгруппах позволил уточнить, что наибольшая частота их развития во время беременности составила у беременных с неполным предлежанием плаценты в подгруппе IВ2 – 43,2% (16/37) против 8% (2/25) в IА2 (χ2=4,097; p=0,043). Та же тенденция в развитии акушерских кровотечений была отмечена и в родах: в основной группе в 3,2 раза реже диагностировались кровотечения у рожениц и родильниц – 22,2% (18/81) против 72% (98/136) соответственно (χ2=16,183; p=0,001). Наибольший процент кровотечений в родах отмечен у пациенток группы сравнения (80,0% (40/50) и 67,5% (25/37) в IВ1 и IВ2 подгруппах соответственно). Полученные данные не противоречат результатам, представленным в других исследованиях [13].
По нашим данным, частота ранних преждевременных родов у беременных в группе высокого риска по невынашиванию с предлежанием плаценты составила 31,3% (68/217). Однако в группе с коррекцией на шейке матки пессарием доктора Арабин преждевременны роды встречались реже на 14,2% (А – 22,2% (18/81), В – 36,7% (50/136), χ2=2,234; p=0,135) и в 2,7 раза реже при сроке гестации до 34 недель – 8,6% (7/81) и 23,5% (32/136) в группах А и В соответственно (χ2=4,678; p=0,031). Отношение шансов (ОШ) рождения доношенного ребенка в основной группе на фоне пессария доктора Арабин в сочетании с прогестероном составляет 2,03 (95% ДИ: 1,085–3,818). Эти результаты аналогичны данным других исследователей [8, 16].
Динамическое наблюдение за расположением плаценты во время беременности позволило выявить различную частоту миграции плаценты в исследуемых группах. А именно, нами выявлено, что в группе с пессарием доктор Арабин миграция плаценты происходит в 1,8 раза чаще – в 48,1% (39/81) случаев в группе А и в 26,4% (36/136) – в группе В (χ2=4,369; p=0,037). Мы полагаем, что благоприятные условия для формирования нижнего сегмента на фоне пессария доктора Арабин улучшают показатели «миграции» плаценты, и в результате снижается количество кровотечений во время беременности в данной группе беременных. ОШ миграции плаценты у пациенток с предлежанием при использовании акушерского пессария составляет 2,5 (95% ДИ: 1,446–4,602).
По данным ряда авторов, пессарий механически воздействует на шейку, изменяя маточно-цервикальный угол [16–18]. В частности, исследование M. Cannie и соавт. (2013) показало, что маточно-цервикальный угол при размещении пессария изменяется в сторону более «острого» у 85,2% женщин, родивших после 34 недель, в то время как у 15,2% пациенток, родоразрешившихся до 34-недельного срока беременности, он оставался неизменным [17]. В нашем исследовании проводилось измерение переднего маточно-цервикального угла в группах пациенток с предлежанием плаценты и определение индекса Пурсело в аркуатных артериях в области плацентации. Выявлено, что в группе IIА (n=29), то есть с коррекцией пессарием шейки матки, произошло изменение угла в сторону более «тупого» на 7,4° (106,3±10,8° до постановки и 113,7±10,7° в сроке 32–33 недели на фоне пессария). По нашему мнению, данный диапазон значений угла можно считать прогностически неблагоприятным по риску преждевременных родов.
В доступной литературе мы не нашли работ, посвященных измерению IR в аркуатных артериях у беременных при предлежании плаценты. Ранее проведенное исследование K. Czajkowski (2007) позволило выявить положительное влияние микронизированного прогестерона на индексы резистентности и пульсационные индексы в спиральных артериях на малых сроках беременности [19].
В проводимом нами исследовании удалось выявить значимые различия IR в аркуатных артериях в группах с пессарием и без. А именно, в сроке 32–33 недели в группе с пессарием и исходом «миграция плаценты», выявлены наименьшие значения IR – 0,53±0,04, тогда как в группе без пессария и с исходом «без миграции плаценты» этот показатель зарегистрирован значимо выше – 0,69±0,14 (р=0,001). По нашему мнению, более низкие IR в аркуатных артериях в месте плацентации на фоне комбинированной терапии (пессарий доктора Арабин в сочетании с прогестероном) способствуют лучшему кровоснабжению нижнего сегмента матки и, как следствие, более «благоприятной» миграции плаценты в группе с предлежанием.
Заключение
Профилактическое использование акушерского пессария доктора Арабин в сочетании с прогестероном в сроках от 11 до 22 недель гестации в группе беременных высокого риска по невынашиванию с предлежанием плаценты позволяет в 2,7 раза снизить частоту преждевременных родов в сроке гестации до 34 недель.
Наибольший процент осложнений в виде кровотечений выявлен в группе сравнения: во время беременности у пациенток с неполным предлежанием (48,6%), в родах – у рожениц с полным предлежанием плаценты (80,0%). Применение акушерского пессария доктора Арабин у беременных с предлежанием плаценты в 3 раза снижает риск развития кровотечений во время беременности в родах.
В 48,1% случаев у беременных с предлежанием плаценты, на фоне пессария доктора Арабин и приема микронизированного прогестерона, происходит миграция плаценты за счет снижения IR в аркуатных артериях и изменения переднего маточно-цервикального угла в сторону более «тупого».
Таким образом, применение акушерского пессария доктора Арабин в сочетании с прогестероном в группе беременных высокого риска с предлежанием плаценты как метод профилактики ранних преждевременных родов должно найти широкое использование в практическом здравоохранении.