The features of sexual function in gynecologic patients
Aim. To investigate the features of sexual function in women with gynecological diseases undergoing screening in clinical settings.Stenyaeva N.N., Khritinin D.F., Chausov A.A., Grigor’ev V.Yu.
Materials and methods. This was a cross-sectional study of the sexual activity and sexual functioning of 1256 women who sought outpatient medical care at the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia from 2014 to 2018, of which 602 (group 1) due to infertility (ICD 10 - N97) and 654 made up the control group(group 2). Baseline evaluation included a detailed medical history, clinical examination, and sexual health testing.
Results. Compared with patients in group 2, patients in group 1 were more likely to have a history of salpingitis and oophoritis, uterine inflammatory diseases excluding the cervix, and endometriosis (p = 0.001). Decreased sexual functioning (FSFI ≤ 26.55) was observed in both groups in patients with inflammatory diseases of female pelvic organs (salpingitis, oophoritis, and uterine inflammatory diseases excluding the cervix) (p = 0.03), endometriosis (p = 0.01), and uterine fibroids (p = 0.02). Also, differences were found in the number of individuals with reduced sexual function in the study groups (p = 0.0001). Infertile women were found to have 1.54-fold higher odds of having sexual dysfunction (FSFI ≤26.55) than fertile women (OR = 1.54, 95%CI 1.19; 1.99). There were significant differences between women in groups 1 and 2 with normal sexual function (FSFI> 26.55) in domain scores for orgasm (p = 0.03), pain (p = 0.02), and satisfaction” (p = 0.06, at the level of the trend). Women in groups 1 and 2, who had sexual dysfunction (FSFI≤ 26.55) also had significant differences in domain scores for sexual desire (p = 0.01), lubrication (p = 0.04), and pain (p = 0.03).
Conclusion. The present study convincingly showed that infertile women with inflammatory diseases of pelvic organs, endometriosis, and uterine fibroids have a high risk of sexual dysfunction, including decreased libido, insufficient vaginal lubrication, and dyspareunia.
Keywords
One of the strongest contributors to the quality of life is sexual health, which comprises a wide range of biopsychosocial indicators characterizing the mental and somatic aspects of health [1]. Sexual functioning is ensured by the integrated interaction of biological, mental, and sociocultural factors and is realized due to a combination of psychophysiological and emotional reactions, experiences and actions of a person associated with sexual desire and satisfaction [2]. Currently, the relationship between gynecological diseases and sexual activities and function in couples has not been sufficiently explored.
The Consensus Statement from the 4th International Consultation on Sexual Medicine reported the incidence and prevalence of sexual dysfunction in women and men [3]. The studies investigating the incidence and prevalence of sexual dysfunctions in women and men demonstrated a high level of variability in their findings ranging from 8.5 to 80%. Substantial variability in the incidence, duration, and structure of sexual dysfunctions was associated primarily with differences in age, and the presence of somatic comorbidities and mental diseases in the studied populations.
In the current International Classification of Diseases (ICD-10), the most common disorders related to female sexual dysfunction include disorders of sexual desire and arousal, orgasmic dysfunction, as well as vaginismus and dyspareunia [4]. Criteria for sexual dysfunctions require the presence of specific symptoms, causing stress and lasting for at least six months [5].
The study aimed to investigate the features of sexual function in women with gynecological diseases undergoing screening in clinical settings.
Material and methods
This was a cross-sectional study of the sexual activity and sexual functioning of 1256 women who sought outpatient medical care at the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia from 2014 to 2018, of which 602 due to infertility (ICD 10 - N97). Baseline clinical evaluation included a detailed medical history, clinical examination, and sexual health testing using the Female Sexual Function Index (FSFI) questionnaire. In accordance with the recommendations, the criterion for clinically significant female sexual dysfunction was a total FSFI score of ≤26.55 [6, 7]. Women (21 patients) who did not complete the questionnaires were excluded from the study. In total, survey results of 1235 women were analyzed including 597 women with infertility (group 1) and 638 women undergoing an outpatient gynecological examination (group 2). Criteria for inclusion in the study were age from 18 to 49, having a permanent sex partner, the absence of pregnancy at the time of the study, and consent to participate in the study. The study protocol was approved by the local ethics committee.
Statistical analysis was performed using the IBM SPSS version 22 software. Quantitative variables were expressed as means (M) and standard deviation (SD) and qualitative variables were summarized as counts and percentages. Continuous variables showing normal distribution and equal sample variances were compared with Student’s t-test. Categorical variables were compared by the χ2 test. Odds ratios (ORs) with 95% confidence intervals (95% CI) were calculated to determine the effect of factors on outcomes. The critical level of significance when testing statistical hypothesis was considered at p <0.05.
Results
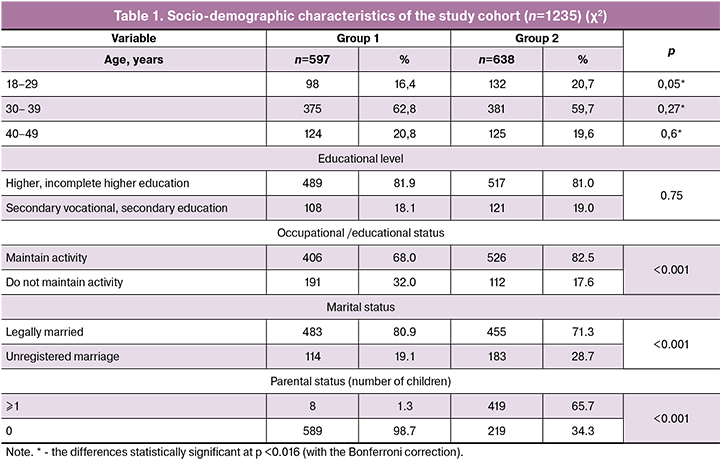
Most of the study participants were of reproductive age, including 230 (18.62%) women aged from 21 to 29 and 756 (61.22%) from 29 to 39. The study cohort was characterized by a high social and employment status and educational level. A total of 938 (75.95%) women were legally married (table. 1). A comparative analysis of the socio-demographic variables of the study participants showed that both groups were comparable in age and educational level. However, they statistically significantly differed in marital and parenting status (p <0.001). Legally married and single women constituted 80.90% (483) versus 19.10% (114) in group 1 and 71.32% (455) versus 28.68% (183) in group 2. At the same time, among the patients undergoing assisted reproductive technology (ART), the proportion of legally married women was higher than in group 2 (p < 0.001). It should be noted that, as a rule, infertility treatment was sought by childless women, and only eight women in group 1 had one child after the previous ART program (n=6) or from a previous marriage (n=2).
The most common morbidities experienced by the study participants according to the analysis of their anamnestic data are summarized in Table 2. No statistical differences were observed between both groups regarding the incidence of infectious diseases, childhood infections, acute respiratory viral infections, chronic sinusitis, diseases of stomach, liver, kidneys, lower extremities varicose veins, as well as impaired thyroid function and benign thyroid nodules. Patients in group 1 were more likely to have a history of herpetic infection (p <0.001), allergic reactions (p = 0.004), chronic tonsillitis (p = 0.04), and surgical interventions, including appendectomy (p = 0, 03) and tonsillectomy (p = 0.03). Also, patients in group 1 more often tended to be overweight (p = 0.07).

An analysis of the gynecological history of the study participants revealed that their gynecological and related morbidities were mainly represented by inflammatory diseases of female pelvic organs (N70-N77) (n=475; 38.46%), non-inflammatory diseases of female genital organs (n=415; 33.60%), sexually transmitted infections (STIs) (n=235; 19.03%) (Table 3). Compared with patients in group 2, patients in group 1 were more likely to have a history of inflammatory diseases of female pelvic organs, including salpingitis and oophoritis (p = 0.001), and uterine inflammatory diseases excluding the cervix (p = 0.001). However, no statistical differences were observed in the incidence of inflammatory diseases of the cervix, vagina, and vulva. Compared with patients in group 2, more patients in group 1 had endometriosis (p <0.001). Non-inflammatory disorders of the ovary, fallopian tube, and broad uterine ligament were also tended to be observed more often in group1 (p = 0.07). Both groups had a comparable incidence of uterine fibroids, polyps of female genital organs, cervical erosion, menometrorrhagia, and dysmenorrhea. Among STIs, patients in group 1 tended to more often report a history of past chlamydia infection (p = 0.06).
All study participants with gynecological diseases were more or less engaged in sexual activity. Sexual function in the study participants was assessed using the FSFI questionnaire. Patients of both groups reported a decrease in sexual functioning during the manifestation of the underlying disease. We analyzed the features of sexual functioning in the study groups depending on the presence of various gynecological diseases.
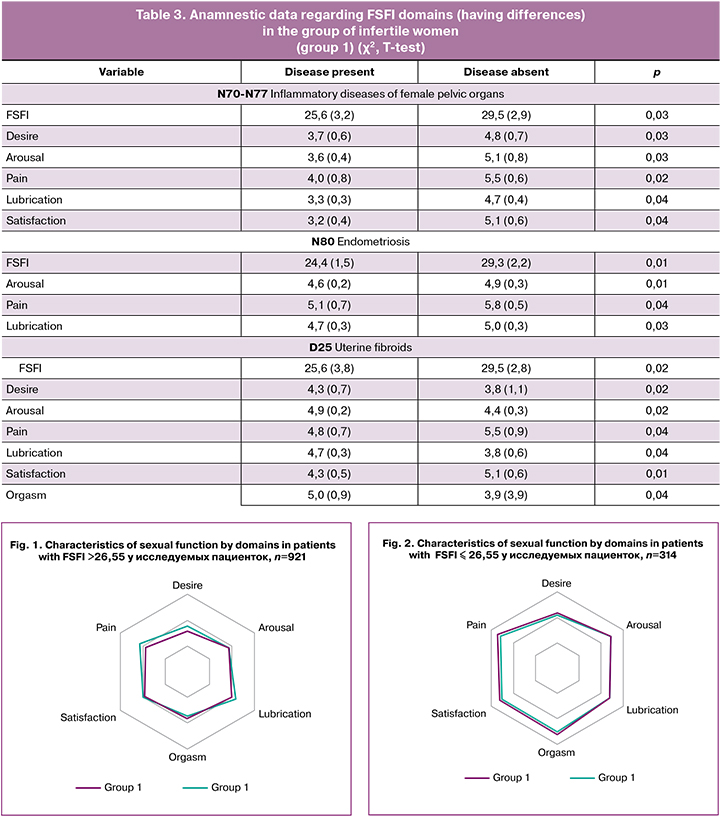
A decreased total FSFI score (FSFI ≤ 26.55) was observed in both groups in patients with inflammatory diseases of female pelvic organs (salpingitis, oophoritis, and uterine inflammatory diseases excluding the cervix) (p = 0.03), endometriosis (p = 0.01), and uterine fibroids (p = 0.02). A decrease in sexual functioning was noted during the manifestation of STIs (trichomoniasis, herpes viral infection of genitalia and urogenital tract), treatment of non-inflammatory disorders of the ovary, fallopian tube and broad uterine ligament, other non-inflammatory uterine diseases, polyps of female genital organs lasting less than three months, and was regarded as adaptive response.
There were differences in the number of individuals with reduced sexual functioning in the study groups (p <0.001). Infertile women had 1.54-fold higher odds of having sexual dysfunction (FSFI ≤ 26.55) than fertile women (OR = 1.54, 95%CI 1.19; 1.99).
A comparison of FSFI scores of women in groups 1 and 2, who had FSFI≥ 26.55showed significant differences in domain scores for orgasm (p = 0.03) and pain (p = 0.02) and differences on the level of a trend in scores for satisfaction (p = 0.06). At the same time, no differences were found in domain scores for sexual desire, arousal, and vaginal lubrication (Fig. 1).
These findings suggest that infertile women with normal sexual function have higher levels of orgasmic sensations and sexual satisfaction.
A comparison of FSFI scores of women in groups 1 and 2, who had FSFI≤ 26.55showed significant differences in domain scores for sexual desire (p = 0.01), lubrication (p = 0.04), and pain (p = 0.03). No differences were found in scores for sexual arousal, orgasm, and satisfaction (Fig. 2).
Therefore, compared with fertile women (group 2), infertile women with sexual dysfunction (FSFI≤ 26.55) in group 1 experienced a decrease in sexual desire and insufficient vaginal lubrication, which indirectly reflects the level of arousal and manifestations of dyspareunia in reproductive-aged women.
Discussion
Analysis of socio-demographic characteristics of infertile patients showed that they were comparable in age and educational level with the control group, but differed in marital and parental status. It was found that the overall morbidity of patients in both groups was comparable, however, in patients with infertility were more likely to have a history of herpetic infection (p = 0.001), allergic reactions (p = 0.004), chronic tonsillitis (p = 0.044), as well as surgical interventions, including appendectomy (p = 0.031) and tonsillectomy (p = 0.029). This observation may suggest that patients with infertility have a higher infectious index than women in the control group, which was also confirmed by other researchers [8–10].
An analysis of the gynecological history of the study patients showed that patients with infertility had higher incidence rates of salpingitis and oophoritis (p <0.001), uterine inflammatory diseases excluding the cervix (p <0.001), and endometriosis (p = 0.001), as in studies of other authors [11-13].
Sexual dysfunction (FSFI ≤ 26.55) was found in both groups in patients with inflammatory diseases of female pelvic organs (salpingitis and oophoritis, uterine inflammatory diseases excluding the cervix) (p = 0.03), endometriosis (p = 0.01), and uterine fibroids (p = 0.02). Also, differences were found in the number of individuals with reduced sexual function in the study groups (p = 0.0001). Infertile women had 1.54-fold higher odds of having sexual dysfunction (FSFI ≤ 26.55) than fertile women (OR = 1.54, 95%CI 1.19; 1.99).
Statistical analysis showed significant differences between women in groups 1 and 2 with normal sexual function (FSFI> 26.55) in domain scores for orgasm (p = 0.03) and pain (p = 0.02) and differences on the level of a trend in scores for satisfaction (p = 0.06). Women in groups 1 and 2, who had sexual dysfunction (FSFI≤ 26.55) had significant differences in domain scores for sexual desire (p = 0.01), lubrication (p = 0.04), and pain (p = 0.03).
Therefore, decreased sexual functioning was often associated with infertility, inflammatory diseases of female reproductive organs, and endometriosis. These findings may explain the result of a recent study investigating differences in the prevalence of sexual dysfunction between primary and secondary infertile women, which reported a higher prevalence of sexual dysfunction in secondary infertile women [14].
Conclusion
The study findings provided evidence that patients with infertility were more likely to have a history of a herpetic infection (p = 0.001), allergic reactions (p = 0.004), chronic tonsillitis (p = 0.044), as well as surgical interventions, including appendectomy (p = 0.031) and tonsillectomy (p = 0.029).
Compared with patients in group 2, patients in group 1 were more likely to have a history of inflammatory diseases of female pelvic organs (salpingitis, oophoritis, and uterine inflammatory diseases) (p = 0.03), endometriosis (p = 0.01), and uterine fibroids (p = 0.02).
The number of infertile women with sexual dysfunction (FSFI ≤ 26.55) (group 1) was greater than that among fertile women in the control group (group 2) (p = 0.0001). Patients in group 1 were found to have 1.54-fold higher odds of having sexual dysfunction (FSFI ≤ 26.55) than fertile women (OR = 1.54, 95%CI 1.19; 1.99).
Patients with infertility and normal sexual function (FSFI> 26.55) had higher scores for orgasm (p = 0.03) and sexual satisfaction (p = 0.06), and lower scores for pain (p = 0.02) in comparison with the control group.
Patients of group 1 with impaired sexual function (FSFI ≤ 26.55) had significantly lower scores for sexual desire (p = 0.01), lubrication (p = 0.04), and higher pain scores (p = 0.03) than patients in the control group.
The present study convincingly showed that infertile women with inflammatory diseases of pelvic organs, endometriosis, and uterine fibroids have a high risk of sexual dysfunction, thus confirming the need to include sexual health care in the management and rehabilitation of gynecologic patients.
References
- The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995; 41(10): 1403–9. doi: 10.1016/0277-9536(95)00112-k
- Васильченко Г.С., ред. Общая сексопатология. Руководство для врачей. М.: Медицина; 2005. 512 с. [Vasil’chenko G.S., red. Obshhaja seksopatologija. Rukovodstvo dlja vrachej. M.: Medicina; 2005. 512 s. (in Russ.)]
- McCabe M.P., Sharlip I.D., Lewis R., Atalla E., Balon R., Fisher A.D., et al. Incidence and Prevalence of Sexual Dysfunction in Women and Men: A Consensus Statement from the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016; 13(2): 144–52. doi: 10.1016/
- j.jsxm.2015.12.019.http://www.mkb10.ru
- McCabe M.P., Sharlip I.D., Atalla E., Balon R., Fisher A.D., Laumann E., et al. Definitions of sexual dysfunctions in women and men: a consensus statement from the fourth international consultation on sexual medicine 2015 J. Sex. Med. 2016: 13: 135–43. doi: 10.1016/j.jsxm.2015.12.019.
- Rosen R., Brown C., Heiman J., Leiblum S., Meston C., Shabsigh R., Ferguson D., D’Agostino R. Jr. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26(2): 191–208. doi: 10.1080/009262300278597
- Wiegel M., Meston C., Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005; 31(1):1–20. doi:10.1080/00926230590475206
- Bashiri A., Halper K.I., Orvieto R. Recurrent Implantation Failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol. 2018; 16(1): 121. doi: 10.1186/s12958-018-0414-2.
- Доронина О.К., Дейлидко Э.Н. Применение плазмы, обогащенной растворимыми факторами тромбоцитов, у женщин в циклах ЭКО. Медицинский журнал. 2018; 4: 53–7. [Doronina O.K., Daylidko E.N., Mordus O.N. The use of plasma enriched with soluble platelet factors in women in IVF cycles. Medical Journal. 2018; 4: 53–7. (In Russian)]
- Мурашко О.В., Доронина О.К., Ярец Ю.И., Шевченко Н.И. Анализ показателей цитокинов при лечении кистозных доброкачественных опухолей яичников. Медико-биологические проблемы жизнедеятельности. 2016; 2(16): 78–84. [Murashko O.V., Doronina O.K., Yarets Y.I., Shevchenko N.I. The analysis of cytokine indices in the treatment of benign cystic ovarian tumors. Mediko-biologicheskie problemy zhiznedejatel’nosti. 2016; 2(16): 78–84. (In Russian)]
- La Rosa V.L., Barra F., Chiofalo B., Platania A., Di Guardo F., Conway F., Di Angelo Antonio S., Lin LT.J An overview on the relationship between endometriosis and infertility: the impact on sexuality and psychological well-being. Psychosom Obstet Gynaecol. 2019; 30: 1–5. doi: 10.1080/0167482X.2019.1659775.
- Kimura F., Takebayashi A., Ishida M., Nakamura A., Kitazawa J., Morimune A., Hirata K., Takahashi A., Tsuji S., Takashima A., Amano T., Tsuji S., Ono T., Kaku S., Kasahara K., Moritani S., Kushima R., Murakami T. Review: Chronic endometritis and its effect on reproduction. J Obstet Gynaecol Res. 2019; 45(5): 951–60. doi: 10.1111/jog.13937
- Curry A., Williams T., Penny M.L. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019; 100(6): 357–64. PMID: 31524362
- Keskin U., Coksuer H., Gungor S., Ercan C.M., Karasahin K.E., Baser I. Differences in prevalence of sexual dysfunction between primary and secondary infertile women. Fertil Steril. 201; 96 (5):1213–7. doi: 10.1016/j.fertnstert.2011.08.007.
Received 20.02.2019
Accepted 22.02.2019
About the Authors
Natalya N. Stenyaeva, candidate of medical sciences, senior researcher of the Department of Andrology and Urology, Federal State Budgetary Institution National Medical Research Center for Obstetrics, Gynecology and Perinatology named after IN AND. Kulakova ”Ministry of Health of Russia. Tel.: +7 (903) 5380334. E-mail: nataliasten@mail.ruAddress: 117997, Russia, Moscow, ul. Oparina, 4.
Dmitry F. Khritinin, Corr. RAS, MD, professor of the Department of Psychiatry and Narcology, Faculty of Medicine, GBOU VPO First MGMU im. THEM. Sechenov of the Ministry of Health of Russia. Tel.: +7 (495) 609-14-00.
Address: 119991, Moscow, st. Trubetskaya, d. 8, p. 2
Andrey A. Chausov, Head of the Information and Analytical Center of the Department of Regional Cooperation and Integration of FSBI “NICC AGP named after
IN AND. Kulakova ”Ministry of Health of Russia. Tel.: +7 (910) 4808485. Email: andreaschausov@gmail.com
Address: 117997, Moscow, st. Oparina, 4.
Vyacheslav Yu. Grigoryev, Clinical Resident IN AND. Kulakova ”Ministry of Health of Russia.
Address: 117997, Moscow, st. Oparina, 4.
For citation: Stenyaeva N.N., Khritinin D.F., Chausov A.A., Grigor’ev V.Yu.. The features of sexual function in gynecologic patients.
Akusherstvo i Ginekologiya/Obstetrics and gynecology. 2020; 1: 128-34. (In Russian).
https://dx.doi.org/10.18565/aig.2020.1. 128-134