Complications in the surgical treatment of patients with colorectal endometriosis
Objective: To determine the prevalence and types of complications after surgical treatment of patients with colorectal endometriosis using the data of the Department of Surgery, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia.Melnikov M.V., Khilkevich E.G., Chuprynin V.D., Chursin V.V.
Materials and methods: The results of the examination of 692 reproductive-aged women with colorectal endometriosis were analyzed. All patients attended the Department of General Surgery of the above-mentioned Centre for planned surgical treatment in the period from 2010 to 2020. The patients included in the study were operated on by experienced surgeons when there were standard indications for the operation. Various surgical approaches were performed according to clinical recommendations. Depending on the presence or absence of complications in the postoperative period, the patients were divided into two groups: the study group included the patients with complications (n=78) and the control group included the patients without complications (n=614).
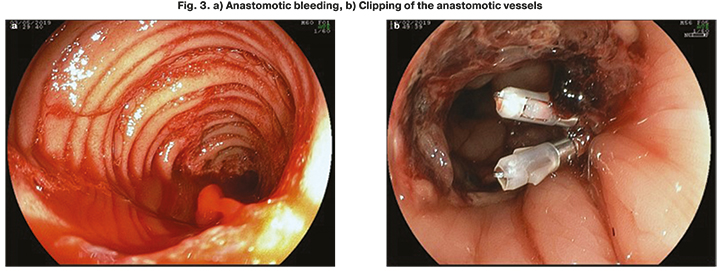
Results: The median age was 33.1 years (Q1–Q3: 27.0–47.0 years). Anastomosis failure after low and ultra-low resections of the rectum developed in 29/692 (4.1%) cases and manifested as pelvic abscess, diffuse peritonitis, or symptoms of endogenous intoxication. The complication always required repeated surgical intervention, suturing of the site of anastomosis failure or dissociation of anastomosis and the formation of a protective colostomy, drainage of the abdominal cavity, intensive therapy, and combined antibacterial treatment. Enteroanastomosis bleeding developed in 17/692 (2.4%) patients and was intensive with a total volume of 500 to 1500 ml. In all cases, endoscopic method with the use of argon plasma coagulation and clipping of the artery (vein) was used to stop the bleeding. Anastomosis stricture was diagnosed in 32/692 (4.6%) women. The endoscopic method for treating cicatricial strictures of colonic anastomoses is preferable.
Conclusion: The treatment of complications which occur after surgery for colorectal endometriosis proves to be challenging and requires the involvement of experts from surgical centers and a multidisciplinary approach.
Keywords
Deep infiltrating endometriosis requires surgical treatment. As a rule, the extent of surgery is significant and it includes not only the excision of endometrioid heteropias, but also the resection of the colon, bladder, vagina, ureterolysis and ureteral implantation. And, what is especially important, there is a high frequency of repeated operations. This is partly due to the non-optimal extent of the first surgical intervention. The patients undergoing repeated operations have gross anatomical changes in the pelvic organs and abdominal cavity, therefore operations are performed in difficult conditions. This significantly increases the risk of iatrogenic complications.
The psychological state of the patient is also important. Repeated operations and ineffective treatment lead to patient’s despair and distrust.
Thus, it is possible to identify the main characteristics of endometriosis in modern conditions. This is a neglected disease that requires major surgery, often repeated surgical interventions in high-risk anatomical areas.
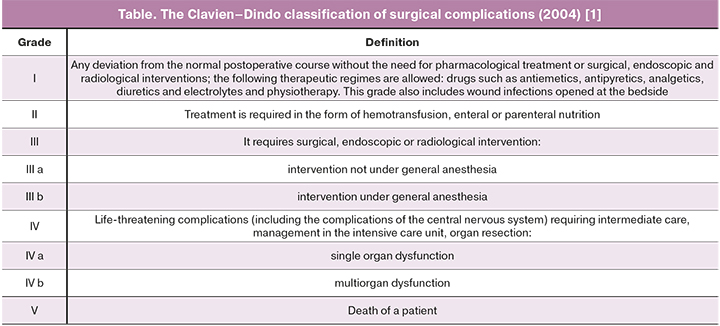
The Clavien-Dindo classification of surgical complications (2004) is presented in the Table [1].
After surgery followed by colon resection, there can be any complications associated with a great extent of surgical intervention on the organs of the abdominal cavity. But pathological changes in the area of the anastomosis, in particular, failed colon anastomosis, are specific for this type of surgery. The total incidence of anastomosis failure is approximately 4% [2].
The aim of the study is to determine the prevalence and types of complications after surgical treatment of patients with colorectal endometriosis using the data of the Department of Surgery, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia.
Materials and methods
A total of 1573 patients were operated on for extragenital endometriosis in the Department of General Surgery from 2010 to 2020.
The results of the examination of 692 reproductive-aged women with colorectal endometriosis were analyzed. All patients attended the Department of Surgery in the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology for planned surgical treatment in the period from 2010 to 2020. The patients included in the study were operated on by experienced surgeons when there were standard indications for the operation. Various surgical approaches were performed according to clinical recommendations.
The patients were included in the clinical study after receiving their informed consent; they were registered according to the standards of the Russian Healthcare Ministry’s ethics committee. The study was approved by the institutional review board of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology.
The clinical and instrumental evaluation of the patients was followed by therapeutic and diagnostic laparoscopy.
There were the following criteria for inclusion in the study: informed consent of the patients to participate in the study, histologically verified endometriosis, reproductive age, absence of hormonal preparations in the treatment during the last 6 months, absence of hyperplastic processes of the endometrium and oncological diseases, absence of acute inflammatory diseases of the pelvic organs, urgent gynecological pathology.
All patients underwent general clinical examination, gynecological examination, rectovaginal examination, ultrasound assessment of the pelvic organs, magnetic resonance imaging of the pelvis, colonoscopy. Surgical treatment was provided to all patients laparoscopically.
The operations were performed under endotracheal anesthesia using the standard method. The extent of surgical treatment in patients with colorectal endometriosis included complete excision of endometrioid foci which was followed by pathomorphological examination of the removed material. The patients were performed colonic segmental exploration in case of invasion of the rectal mucosa and intestinal bleeding, narrowing of the intestinal lumen by 2/3 or more, the presence of an infiltrate on the intestinal wall, a deserosed section of the intestine of 5 cm or more. Such a clinical situation was considered as an absolute indication for colon resection.
There were the following indications for performing colostomy:
1. Simultaneous resection of one of the organs: the vagina or bladder, or ureter, regardless of the level of anastomosis;
2. The distance of the place of anastomosis is less than 8 cm from the anus.
It should be noted that the patients underwent standard preoperative preparation and optimal perioperative management which are provided in the department. The characteristics of the management were described in a previous article [3].
Namely, on the 1st day after the operation, the infusions were minimized, the patients were allowed to drink liquids and take oral medications. The patients were discharged from hospital if they had no symptoms, if they could tolerate at least three meals a day, and if they had stools.
The patients were followed up for a short period of time on days 5 and 30 after their discharge. All adverse events that occurred within 90 days after the operation were considered as complications.
The term ‘anastomosis failure’ refers to all conditions with clinical or radiological signs of anastomosis leakage, with or without the necessity of surgical intervention.
The bleeding was stopped endoscopically (colonoscopy) using argon plasma coagulation and/or vascular clipping. When necessary, relaparoscopy and stitching of the bleeding zone were performed under intraluminal control.
The problems with frequency, constancy and/or ability to control bowel movements that occurred in the postoperative period were considered as intestinal dysfunction.
During the last decade we performed 692 operations for colorectal endometriosis, including 357 circular (anterior) and 99 segmental resections, 236 excisions of endometrioid infiltrates (shaving) of the colon.
Depending on the presence or absence of complications in the postoperative period, the patients were divided into two groups: the study group included the patients with complications (n=78) and the control group included the patients without complications (n=614).
Results
The age of the patients ranged from 27 to 47 years. The median age was 33.1 years (Q1–Q3: 27.0–47.0 years).
The patients with colorectal endometriosis who had complications were compared to ones who did not have any complications in the postoperative period. The comparative analysis included such parameters as duration of the disease, number of concomitant diseases, presence or absence of surgical interventions for endometriosis, duration of surgery, volume of blood loss, length of stay in the hospital and postoperative bed-day.
The duration of the disease ranged from 2 to 12 years; its average duration was 6.7 (6.2–7.2) years. Concomitant somatic pathology was detected in 60/78 (76.9%) patients of the study group and in 442/614 (71.9%) patients of the control group. There were no statistically significant differences in the incidence of concomitant pathology in the groups (p=0.75). However, it should be noted that diabetes mellitus and obesity were more often detected in the study group, namely in 17/78 (21.8%) and 28/78 (35.9%) cases, respectively. Diabetes mellitus was found in 20/614 (3.25%) patients and obesity occurred in 35/614 (5.7%) patients of the control group.
The analysis of anamnestic data showed that the patients of the study group had a previous history of up to 9 surgical interventions for endometriosis, while the patients of the control group underwent no more than 3 operations. The analysis of the average indicators of the number of operations in the patients’ past history revealed a certain pattern: the median of surgical interventions in the patients of the study group was 3 (Q1–Q3: 1–3), while the median in the control group was 1 (Q1–Q3: 0–2); these differences were statistically significant (p<0.001).
The analysis of the operations for endometriosis in the past history of the patients in the study group revealed that surgical procedures were performed laparoscopically in the most cases, namely, in 67/78 (86.7%) patients. More frequently the patients underwent resection of one ovary due to endometrioid cyst (32/78 (41%)), coagulation of endometriosis foci (12/78 (15.4%)), adhesiolysis (11/78 (14.1%)) and excision of endometriosis foci (9/78 (11.5%)). It should be noted that 3/78 (3.8%) patients had a previous history of colon resection due to colorectal endometriosis.
The average postoperative bed-day of patients in the control group was 3.9 (3.0; 5.8) and it was 8.8 (6.0;10.0) in the study group. The average duration of the operation was the shortest in the control group and it was 59 minutes, while the longest one was in the study group (197 minutes). Similarly, the patients of the control group had the lowest average intraoperative blood loss (300 ml) and the patients of the study group had the most excessive intraoperative blood loss (500 ml).
The duration of operations was 3.5–4.5 hours in the period 2010–2015, and it was 1.5–2.5 hours in the period 2016–2020. The decrease in time was due to the advanced training of the surgical team, which included a general surgeon and a gynecologist.
Anastomosis failure after low and ultra-low resections of the rectum developed in 29/692 (4.1%) cases and manifested as pelvic abscess, diffuse peritonitis, or symptoms of endogenous intoxication (video presentation is available at https://aig-journal.ru/archive).
 The complication always required repeated surgical intervention, suturing of the site of anastomosis failure or dissociation of anastomosis and the formation of a protective colostomy, drainage of the abdominal cavity, intensive therapy, and combined antibacterial treatment.
The complication always required repeated surgical intervention, suturing of the site of anastomosis failure or dissociation of anastomosis and the formation of a protective colostomy, drainage of the abdominal cavity, intensive therapy, and combined antibacterial treatment.
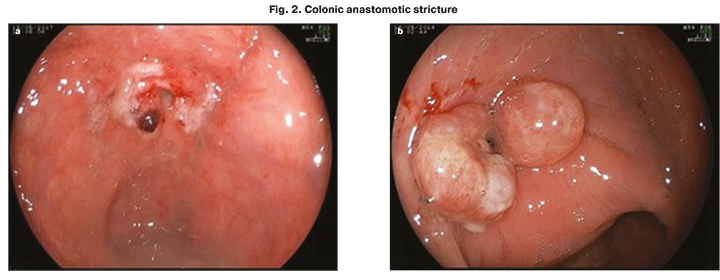
Anastomotic stricture developed during operations for colorectal endometriosis due to inadequate blood supply which was caused by devascularization occurring in mobilization and isolation of the intestine from the infiltrate and its spread to the mesorectal tissue.
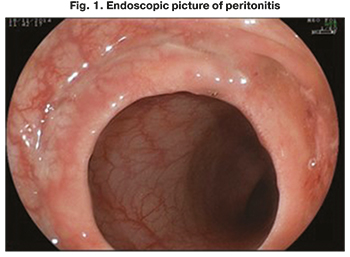
According to the literature data, cicatricial narrowing occurs in 5–17% of cases when apparatus is used in colon anastomosis [4]. The normal view of anastomosis is shown in Figure 1.
The manifestation of anastomotic stricture is an impairment of the evacuation function of the large intestine, and there is an acute intestinal obstruction in advanced cases.
According to the results of our study, anastomotic stricture was diagnosed in 32/692 (4.6%) women (Figure 2). It is preferable to apply the endoscopic method of treating cicatricial strictures of colonic anastomoses due to the technical difficulties of repeated reconstructive surgery and the high risk of complications. The dissection of the connective tissue membrane is performed with the help of Fuginon EC-590 WI video colonoscope using KLS MARTIN surgical unit, an end-type and/or cannulation papillotome (depending on the type of anastomosis: end-to-end, end-to–side) in a mixed mode (cutting – 40–50 Watts and coagulation – 50–60 Watts); the edges of anastomosis are cleaned with argon plasma coagulation in the spray mode for preventing the recurrence of stricture.
Enteroanastomosis bleeding occurred in 17/692 (2.4%) patients, it was profuse with a total volume of 500 to 1500 ml and with signs of posthemorrhagic anemia. In one case, this complication was diagnosed and eliminated during surgery, in most cases it was in the early (first hours) postoperative period.
In all cases, endoscopic method with the use of argon plasma coagulation and clipping of the artery (vein) was used to stop the bleeding (Fig. 3).
Discussion
A number of authors propose to classify the risk factors for the development of complications of colorectal surgery and preventive measures to eliminate or reduce them, taking into account the patient’s condition, the conditions of the operation and surgical technique. The recommendations include such risk factors as the use of anastomosis apparatus or manual stitching; intraoperative air leakage test to check the integrity of anastomosis; systematic use of pelvic and transanal drainage; the use of protective ileostomy for low rectal resections; closing of the vagina before intestinal resection; administration of oral antibiotics the day before surgery and performing partial mesorectal resection of the intestinal wall. According to these authors, diverting stoma formation can reduce the incidence and clinical consequences of anastomosis failure in more than 65% of rectal resections, however, it can cause serious side effects [5].
We agree with the authors of the article [5] that checking the tightness of anastomosis makes it possible to minimize the number of protective stomas in surgery for endometriosis. In our study, we applied only mechanical anastomosis and checked the tightness of anastomosis, the formation of a sigmostoma in case of low intestinal resections; we did not use simultaneous resection of the vagina and intestines, antibiotic prevention or therapy. Surgical intervention was performed by experienced surgeons according to the existing clinical protocols.
According to some authors [2], the most common surgical complications are rectovaginal fistulas, anastomosis failure and abscesses. Postoperative bleeding is rare, but it has been reported to require a blood transfusion without surgery. Multidisciplinary approach and complete preoperative imaging examination by an experienced doctor are necessary when selecting patients for surgery. The surgical procedure is complex as it includes resection of all extrarectal lesions of deep infiltrating endometriosis. It often occurs in patients with previous surgeries. Taking into account the main possible complications, three most frequent risk factors can be identified. First, it is the opening of the vagina during the operation on the intestines. However, this is a matter of debate, and experts usually open the vagina during the procedure when it is necessary without increasing the frequency of complications. Secondly, it is the excessive use of electrocoagulation, which increases the risk of rectovaginal fistulas and abscesses due to the risk of necrosis of the posterior part of the vaginal cuff. And the third factor is the increased risk of anastomosis failure due to rectal resection performed in the presence of an endometrioid infiltrate at a distance of 5–8 cm from the anal margin. In order to prevent and treat such complications, it is necessary to conduct further research [2].
We support the opinion of these researchers [2] regarding the frequency and types of postoperative complications of colorectal endometriosis. And we also agree that it is impractical to perform simultaneous resection of the intestine and vagina due to the high risk of anastomosis failure; in case of extreme necessity, it is recommended to perform colostomy. We support the opinion of the researchers that low colon resections also increase the risk of anastomosis failure.
As for functional disorders of the gastrointestinal and genital tract, we consider them important. Their impact on a woman’s quality of life is significant. This should be taken into account when choosing the perioperative management of such patients.
A number of researchers have conducted studies on the assessment of the safety of discoid and segmental resection of the colon in colorectal endometriosis. The authors conclude that discoid resection is probably the best option for minor lesions due to the possibility of its implementation and low frequency of complications [6].
Some authors carried out a comparative assessment of complications and relapses after three types of surgical treatment of colorectal endometriosis, namely: segmental resection, discoid resection and shaving. The authors concluded that segmental resection is associated with a high frequency of postoperative complications and a low frequency of relapses, and it should be performed mainly in young women. Discoid resection and shaving showed a higher frequency of relapses and may be more suitable for women approaching menopause due to a lower probability of relapse [7]. However, we do not agree with the last statement regarding women of premenopausal age, because the risk of oncological pathology, in particular, endometrial sarcoma, increases at this age.
We support the tactics of reasonable radicalism and consider it justified to perform resection of the colon when there is the invasion of the rectal mucosa and the presence of intestinal bleeding, narrowing of the intestinal lumen by 2/3 or more, the presence of an infiltrate on the intestinal wall and deserosed part of the intestine for 5 cm or more.
Interesting data were obtained by the authors of the article [8], who evaluated the frequency, risk factors and treatment of colorectal anastomosis stenosis in patients who underwent rectosigmoid resection for colorectal endometriosis. A total of 1643 patients underwent laparoscopic rectosigmoid resection. Symptomatic stenosis of anastomosis was revealed in 104 (6.3%) patients, among them 90 (86.5%) patients underwent endoscopic dilation three times. In conclusion, the researchers determined that anastomotic stricture is a recognized complication in patients after intestinal resection for deep infiltrating endometriosis and protective ileostomy is the only variable factor associated with anastomotic stenosis. Endoscopic dilation is a good treatment option for this complication.
We cannot disagree with the authors’ conclusions about symptomatic stenosis. However, in our study, we considered anastomotic strictures that required surgical intervention.
There are some studies devoted to the analysis of complications developed during the formation of stomas in colorectal surgery [4]. According to these data, the complications are non-specific. Most of the complications of the Clavien–Dindo classification were wound or urinary infections after the closure of the stoma. The Clavien–Dindo complications of grade III occurred in 14 patients (8.6%) and were associated with leakage, hemoperitoneum, abdominal wall hernia, subcutaneous abscess and intestinal obstruction syndrome. The authors suggest taking into account the risk of these complications and providing complete preoperative information to patients and their families.
It is worth noting that we did not analyze complications of the Clavien–Dindo classification of grades I–II in this article.
According to some authors [9], colorectal surgery of endometriosis has a significant impact on the function of the urinary tract, regardless of the technique. However, shaving causes less postoperative urination dysfunction than discoid or segmental resection. Unfortunately, such an analysis was not carried out in our study, but we consider this information useful for further work.
Conclusion
Late diagnosis and an increase in the number of palliative interventions for advanced endometriosis lead to an increase in the number of complex, traumatic, potentially dangerous operations.
The treatment of complications which occur after surgery for colorectal endometriosis proves to be challenging and requires the involvement of experts from surgical centers and a multidisciplinary approach.
On the one hand, it is necessary for the surgeons who are able to operate on the patients with common forms of deep infiltrating endometriosis and ready for the treatment of complications to take systematic training in difficult clinical situations such as the described cases of complications; on the other hand, the surgeons should not refuse to perform radical and organ-saving operations due to these difficulties.
References
- Dindo D., Demartines N., Clavien P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004; 240(2): 205-13. https://dx.doi.org/10.1097/01.sla.0000133083.54934.ae.
- Bouaziz J., Soriano D. Complications of colorectal resection for endometriosis. Rev. Minerva Ginecol. 2017; 69(5): 477-87. https://dx.doi.org/10.23736/S0026-4784.17.04052-7.
- Лисовская Е.В., Хилькевич Е.Г., Чупрынин В.Д., Мельников М.В., Яроцкая Е.Л. Оценка качества жизни пациенток после хирургического лечения глубокого инфильтративного эндометриоза в раннем послеоперационном периоде. Акушерство и гинекология. 2019; 11: 197-200. [Lisovskaya E.V., Khilkevich E.G., Chuprynin V.D., Melnikov M.V., Yarotskaya E.L. Assessment of the quality of life of patients after surgical treatment of deep infiltrative endometriosis in the early postoperative period. Obstetrics and gynecology. 2019; 11:197-200. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.11.197-200.
- Bonin E., Bridoux V., Chati R., Kermiche S., Coget J., Tuech J.J., Roman H. Diverting stoma-related complications following colorectal endometriosis surgery: a 163-patient cohort. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019; 232: 46-53. https://dx.doi.org/10.1016/j.ejogrb.2018.11.008.
- Smith A.V., Sumak R., Cabrera R., Kondo W., Ferreira H. Bowel anastomosis leakage following endometriosis surgery: an evidence based analysis of risk factors and prevention techniques. Facts Views Vis Obgynv. 2020; 12(3): 207-25.
- Jayot A., Bendifallah S., Abo C., Arfi A., Owen C., Darai E. Feasibility, complications, and recurrence after discoid resection for colorectal endometriosis: A Series of 93 cases. J. Minim. Invasive Gynecol. 2020; 27(1): 212-9. https://dx.doi.org/10.1016/j.jmig.2019.07.011.
- Gutiérrez A.H., Spagnolo E., Zapardiel I., Seivane R.G.-A., Carrasco A.L., Bolívar P.S., Miguelañez I.P. Post-operative complications and recurrence rate after treatment of bowel endometriosis: Comparison of three techniques. Eur. J. Obstet. Gynecol. Reprod. Biol. X. 2019; 4: 100083. https://dx.doi.org/10.1016/j.eurox.2019.100083.
- Bertocchi E., Barugola G., Benini M., Bocus P., Rossini R., Ceccaroni M., Ruffo G. Colorectal anastomotic stenosis: lessons learned after 1643 colorectal resections for deep infiltrating endometriosis. J. Minim. Invasive Gynecol. 2019; 26(1): 100-4. https://dx.doi.org/10.1016/j.jmig.2018.03.033.
- Vesale E., Roman H., Moawad G., Benoit L., Touboul C., Darai E., Bendifallah S. Voiding dysfunction after colorectal surgery for endometriosis: A systematic review and meta-analysis. J. Minim. Invasive Gynecol. 2020; 27(7): 1490-502. e3. https://dx.doi.org/10.1016/j.jmig.2020.07.019.
Received 28.04.2021
Accepted 17.06.2021
About the Authors
Mikhail V. Melnikov, PhD, Head in Clinical Work, Department of Surgery, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-78-33, m_melnikov@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.Elena G. Khilkevich, MD, obstetrician-gynecologist of the Surgery Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics,
Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-77-83, e_khilkevich@oparina4.ru, https://orcid.org/0000-0001-8826-8439, 117997, Russia,
Moscow, Ac. Oparina str., 4.
Vladimir D. Chuprynin, PhD, Head of the Surgery Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-35-75, v_chuprynin@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Vyacheslav V. Chursin, doctor surgeon of General Surgery, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,
Ministry of Health of Russia, +7(495)438-78-33, v_chursen@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Authors’ contributions: Chuprynin V.D., Melnikov M.V., Khilkevich E.G. – developing the idea and design of the study; Chuprynin V.D., Melnikov M.V., Chursin V.V. – collecting clinical material; Khilkevich E.G. – writing and editing the text.
Conflicts of interest: The authors declare that there are no conflicts of interest.
Funding: The investigation has not been sponsored.
Acknowledgment: The authors appreciate the support of the doctors of the Department of Surgery of the V.I. Kulakov National Medical Research Centre for Obstetrics, Gynecology and Perinatology for providing the clinical material.
Patient Consent for Publication: All patients provided informed consent for the publication of their data and associated images.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Melnikov M.V., Khilkevich E.G., Chuprynin V.D., Chursin V.V. Complications in the surgical treatment of patients with colorectal endometriosis.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2021; 9: 100-106 (in Russian)
https://dx.doi.org/10.18565/aig.2021.9.100-106