Autologous platelet rich plasma in complex therapy of women with refractory ‘‘thin’’ endometrium
Objective. To assess the effectiveness of autologous platelet rich plasma (PRP) in complex pretreatment of the women with refractory ''thin'' endometrium prior to assisted reproductive technology (ART) programs. Materials and methods. The research enrolled 68 patients of reproductive age with ''thin'' endometrium, refractory to e standard therapy, implantation failures and the history of ET cycle cancellation. Patients from the main group (n=38) first received physical therapy starting from day 5–7 of the menstrual cycle within 10 days. During the next menstrual cycle they received 35–40 ml of autologous PRP injections to the endometrium by hysteroscopy with use of endoscopic needle. Patients from the control group (n=30) were treated using only physical therapy. During the possible ‘‘implantation window’’ prior to and after the therapy endometrium thickness and hemodynamics of the uterine arteries were assessed. Results. Control ultrasound scan documented statistically significant endometrium thickness enlargement during the ‘‘implantation window’’ (p<0,001) in the patients of the main group comparing to those from the control group. According to Doppler velocimetry, this finding was associated with the improvement of uterine hemodynamics measurements. No adverse and allergic reactions, as well as infectious complications were registered after the interventions. Conclusion. The study demonstrated the effectiveness of a new approach to the complex therapy of women suffering from infertility associated with refractory ‘‘thin’’ endometrium and decreased of uterine arteries hemodynamics.Apolikhina I.A., Efendieva Z.N., Fedorova T.A., Belousov D.M., Vishnyakova P.A., Artemova D.A., Fatkhudinov T.Kh.
Keywords
One of the most essential criterion for the success of assisted reproductive technology (ART) programs is morphologically normal endometrium. Insufficient endometrium thickness and low receptivity are associated with reproductive failures and ART programs cancellation due to the absence of proper conditions for embryo implantation [1].
Recent studies regard ''thin'' endometrium as an independent prognostic factor in ART programs [2]. Other researchers recommend considering it as a criterion for embryo cryoconservation for later tramsfer, when the endometrium gains its maximum thickness [3]. Besides it is necessary to take into account that the pregnancy which occurred on the background of ''thin'' endometrium is associated with the risk of spontaneous abortion at early stages, preterm delivery and low birth weight children [4].
It should be noted that uterine arteries hemodynamics disorder is among the leading factors negatively affecting endometrium thickness and receptivity. Angiogenesis plays a key role in the development of endometrium structure and functions necessaryfor embryo implantation. The researchers who study endometrium thickness dynamics in patients with ovarian stimulation cycles and with natural cycles note correlation between endometrium thickness and uterine blood flow [5]. There is also scientific data on predictive potential of subendometrial blood flow in patients undergoing ART programs [6]. Major factors defining the assessment of uterine hemodynamics are myometrium vascularization degree, visualization of vessels of various calibers (uterine, arcuate, radial, basal, spiral arteries), systolic and diastolic pressures, blood flow velocity curve: pulsatility index, resistance index, systolic/diastolic ratio [7].
Today the most common therapy for infertility associated with thin endometrium are aimed at its growth stimulation and uterine blood supply improvement. Apart from traditional hormone therapy cycles, in Russia physiotherapeutic methods of treatment are widely applied [8]. There is data on uterine artery perfusion restoration, endometrium thickness enlargement and increase of pregnancy onset rates after in-vitro fertilization (IVF) resulting from electropulse therapy in complex treatment of women with reproductive failure and ''thin'' endometrium [9]. Other researchers report the use of low-frequency magnetotherapy, acupuncture and neuromuscular electrostimulation in biofeedback to stimulate endometrium growth and effectiveness of ART programs [10].
The use of autologous platelet rich plasma (PRP) is considered a new and prospective trend in modern regenerative and reproductive medicine [11]. Therapeutic effect of PRP is based on the ability of growth factors, cyto- and chemokines contained mainly in platelet α-granules to launch tissue biosynthesis. It was demonstrated that autologous PRP not only stimulates cell proliferation through the growth factors, but also has anti-inflammatory and antimicrobial effect [12]. Autologous PRP stimulates the processes of cell proliferation and regeneration as well as promotes angiogenesis [13, 14].
According to Tandulwadkar S. et al. (2017), autologous PRP in frozen embryo transfer cycles improves endometrium thickness and uterine artery hemodynamics [15]. The 2020 meta-analysis demonstrated that intrauterine administration of autologous PRP led to significant enlargement of endometrium thickness, improvement of implantation and pregnancy rates [16].
Given the fact that the patients included in this study and treated only with physiotherapeutic methods did not have any positive effect, we decided to supplement the regimen with PRP injections into endometrium under hysteroscopic control and using the methods we have developed and described earlier [17].
The aim of this study is to assess the effectiveness of autologous platelet rich plasma (PRP) in complex pretreatment of the women with refractory ''thin'' endometrium prior to entering assisted reproductive technology (ART) programs.
Materials and methods
68 patients of reproductive age with IVF implantation failures and frozen embryo cycle cancellation due to endometrium poor thickness were enrolled in the srudy. The endometrium thickness among the patients during the ''implantation window'' in previous cycles in association with hormone therapy was ≤ 7 mm. Moreover, previous hormone and vitamin therapy as well as treatment with drugs that improve blood circulation did not have any significant impact on pregnancy rates.
All patients were divided into 2 groups. Patients from the main group (n=38) were prepared for embryo transfer in two steps: physical treatment course (the first cycle), autologous PRP injections into endometrium using endoscopic needle under hysteroscopic control (the next cycle). Patients from the control group (n=30) were treated using only physiotherapeutic methods. Physical treatment course was the same for all the patients and comprised electropulse therapy with abdominal and vaginal placement of electrodes on ''BTL-4000 Premium G'' unit. Exposure of physical factors started from day 5–7 of the cycle and was continued daily for 10–12 days. At the second step the patients from the main group (n=38) had PRP injections into endometrium during proliferative phase under the control of hysteroscopy and according to the methods previously described [17]. During the whole period of treatment the patients from both groups did not use barrier contraception.
Inclusion criteria: age 18–39, normal karyotype of the patient and her partner, regular ovulatory menstrual cycle, endometrium thickness no more than 7 mm during ''implantation window''. Exclusion criteria: marked pathospermia in a partner, use of donor gametes, preterm ovarian insufficiency, internal genitalia anomalies, contraindications for physical factors treatment, systemic blood diseases and coagulopathy, Hb level less than 100 g/l, platelet level less than 100х109/l, antiplatelet and anticoagulant therapy during the research.
Patients who were included into the research obtained complete clinical laboratory diagnosis. During the expected ''implantation window'' all of them had pelvic ultrasound scan using Toshiba-Canon Aplio 500 ultrasound machine. To assess endometrium structure and thickness as well as to provide hemodynamic Doppler velocimetry of the uterine arteries intracavitary single-crystal high-density transducer before and after the treatment taking into account the aftereffect of the physical therapy. Doppler velocimetry included colour Doppler imaging and spectral Doppler velocimetry. The results of uterine artery Doppler velocimetry in the mid-luteal phase in fertile women were reported to be normal, as systemized and verified by D. Belousov [18]. Doppler velocimetry provided information on uterine artery branches visualization (uterine, arcuate, radial, basal and spiral), vascularization symmetry, systolic and diastolic pressures, blood flow velocity curve.
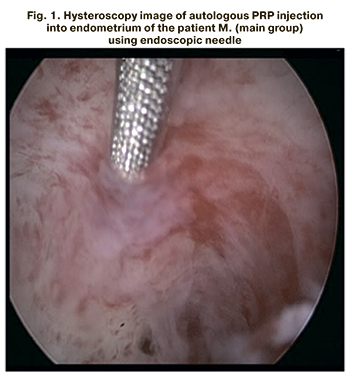 Having signed the informed consent, the patients from the main group (n=38) were treated with 35–40 ml of autologous PRP injections into endometrium at a depth of 2–3 mm on the day 6–8 under intravenous anesthesia and hysteroscopic control. 6–8 targeted PRP injections were made into the most defective areas of the uterine mucosa (Fig. 1).
Having signed the informed consent, the patients from the main group (n=38) were treated with 35–40 ml of autologous PRP injections into endometrium at a depth of 2–3 mm on the day 6–8 under intravenous anesthesia and hysteroscopic control. 6–8 targeted PRP injections were made into the most defective areas of the uterine mucosa (Fig. 1).
During the next menstrual cycle the patients received hormone therapy starting from the 3–4 day. Estrogen (estradiol valerate pill) was given with the starting dose 4 mg a day with further adjustment according to endometrium growth dynamics. Maximum daily estrogen dose was 12 mg. During the second phase the patients got 400 mg of micronized progesterone vaginally. In the mid-luteal phase the patients had control pelvic ultrasound scan and uterine artery Doppler velocimetry to assess endometrium thickness and structure as well as uterine hemodynamics after the therapy. All the patients had their ultrasound scan performed by the same specialist prior to and after the intervention.
Statistical analysis
Statistical analysis of the data was conducted by means of Statistica 10 (USA) software suite and R 3.6.2 (USA) problem-solving environment. To compare quantitative variables between the control and the main groups Mann–Whitney U-test was applied, for qualitative variables Fischer's Exact test was applied. In case of pair observations of qualitative variables McNemar test was employed with exact p-values in binomial probability. Qualitative parameters are demonstrated as absolute numbers and percentage (%), quantitative – as Ме and IQR (Ме (Q1;Q3)), where Ме is a median, Q1 and Q3 – the first and third quartiles. The differences between qualitative parameters were assessed using odds ratio (OR), and for quantitative parameters Hodges-Lehmann estimator and their 95% confidence interval (95% CI) were used. The differences between the variables were considered statistically significant at р<0.05.
Results
The age of the patients enrolled in the research did not statistically significant between the groups, and on average it was 37.5 (32;39) years в in the main group and 34.5 (31;37) years – in the control group (р=0,076). The studied groups were similar and their BMI, E2 level, LH and FSH serum levels, somatic disease rates and infertility duration did not significantly vary. The majority of the patients, included in the study, were previously treated with ART. In this context among the patients from the main group, 89% (34/38) had a history of embryo transfer cancellation (ET) in cryocycles due to poor endometrium growth and despite the therapy carried out. In the control group 83% of the patients had the same history of ET cancellation (25/30) (р=0.5). There is interesting data on a long-term (more than 3 years) use of combined oral contraceptives (COC) among patients enrolled in the study. These included 24% in the main group (9/38), and 27% (8/30) in the control group (р=0.079). Primary infertility was diagnosed in 21% (8/38) of patients from the main group and in 50% (15/30) – from the control group; secondary infertility was, respectively, diagnosed in 79% (30/38) of patients from the main group and in 50% (15/30) from the control group (р=0.02). Besides, the patients from the main group had more burdened gynecologic history: missed abortion in 63% (24/38) of women, compared to 33% (10/30) of the control group (р=0.027). Clinical and history features of the patients are shown in Table 1.
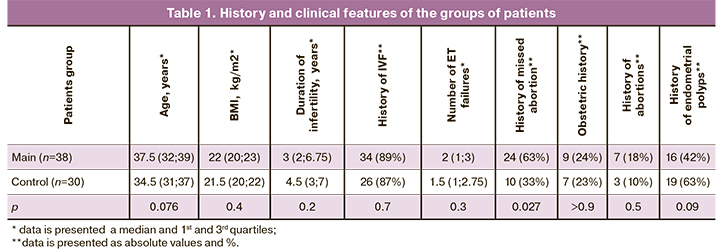
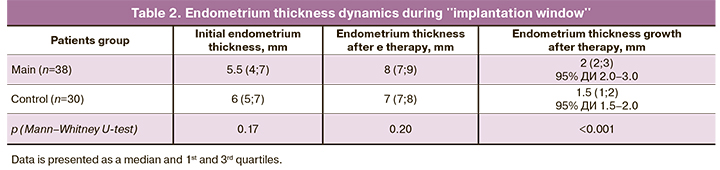
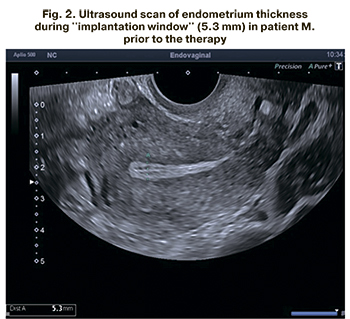 Initial endometrium thickness during ''implantation window'' according to ultrasound scan in the patients, included in the study, did not significantly vary and averaged 5.5 (4;7) mm in the main group and 6 (5;7) mm in the control group (р=0.17) (Fig. 2).
Initial endometrium thickness during ''implantation window'' according to ultrasound scan in the patients, included in the study, did not significantly vary and averaged 5.5 (4;7) mm in the main group and 6 (5;7) mm in the control group (р=0.17) (Fig. 2).
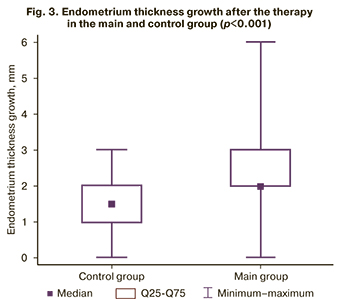
The results of the control ultrasound scan during ''implantation window'' demonstrated no endometrium thinning. Endometrium thickness growth was statistically greater in the main group (95% CI for Hodges–Lehmann estimator 2.0–3.0), than in the control group (95% CI for Hodges–Lehmann estimator 1.5–2.0) after therapy (р<0.001) (Table 2, Fig. 3).
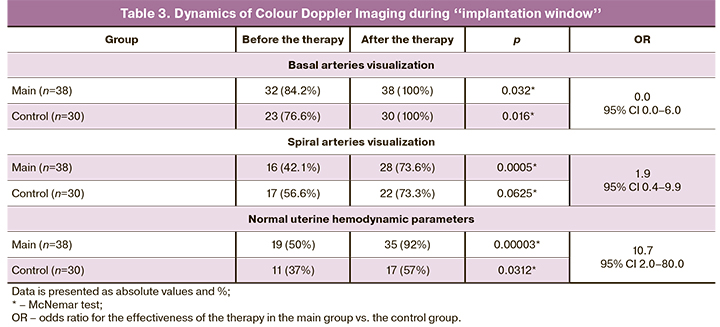
 Except for endometrium thickness dynamics special attention has been given to the assessment of uterine artery hemodynamics (Table 3). Taking into account the initial hemodynamics evaluation, it was noted that basal uterine arteries were visualized in 84.2% (32/38) of the patients from the main group and in 76.6% (23/30) of the patients from the control group (р=0.54); the spiral uterine arteries were seen in 42.1% (16/38) patients in the main group and in 56.6% (17/30) in the control group (р=0.33). After the therapy, in some patients of both groups the end arteries which could not be visualized by Doppler velocimetry initially, appeared visible. Moreover, this finding sustained long after treatment in all patients. Two-step therapy using autologous PRP in the main group caused statistically significant increase in visualization of not only basal, but also spiral uterine arteries. Physical therapy that was used in the control group did not lead to the improvement of spiral arteries visualization rate (р=0.0625 for McNemar test with exact p-values in binomial probability). Among the patients whose basal uterine arteries were not visualized prior to the therapy, they became noticeable in 75% (6/8; 95% CI 35–97%) in the main group and in 100% (7/7; 95% CI 35–97%) in the control group (р=0.47 for Fischer's Exact test). Among the patients whose spiral uterine arteries were not visualized prior to the therapy, visualization became noticeable in 55% (12/22; 95% CI 32–76%) in the main group and in 39% (5/13; 95% CI 14–68%) in the control group (р=0.49 for Fischer's Exact test). As a result, no statistically significant differences were noticed in basal and spiral uterine arteries visualization by the two methods.
Except for endometrium thickness dynamics special attention has been given to the assessment of uterine artery hemodynamics (Table 3). Taking into account the initial hemodynamics evaluation, it was noted that basal uterine arteries were visualized in 84.2% (32/38) of the patients from the main group and in 76.6% (23/30) of the patients from the control group (р=0.54); the spiral uterine arteries were seen in 42.1% (16/38) patients in the main group and in 56.6% (17/30) in the control group (р=0.33). After the therapy, in some patients of both groups the end arteries which could not be visualized by Doppler velocimetry initially, appeared visible. Moreover, this finding sustained long after treatment in all patients. Two-step therapy using autologous PRP in the main group caused statistically significant increase in visualization of not only basal, but also spiral uterine arteries. Physical therapy that was used in the control group did not lead to the improvement of spiral arteries visualization rate (р=0.0625 for McNemar test with exact p-values in binomial probability). Among the patients whose basal uterine arteries were not visualized prior to the therapy, they became noticeable in 75% (6/8; 95% CI 35–97%) in the main group and in 100% (7/7; 95% CI 35–97%) in the control group (р=0.47 for Fischer's Exact test). Among the patients whose spiral uterine arteries were not visualized prior to the therapy, visualization became noticeable in 55% (12/22; 95% CI 32–76%) in the main group and in 39% (5/13; 95% CI 14–68%) in the control group (р=0.49 for Fischer's Exact test). As a result, no statistically significant differences were noticed in basal and spiral uterine arteries visualization by the two methods.
After the therapy, abnormal uterine hemodynamic parameters in some of the patients became reassuring; besides none of the patients had any deterioration of hemodynamics. According to the control Doppler velocimetry the proportion of women with normal uterine artery hemodynamics increased and became statistically significant (р=0.00003 in the main group and р=0.0312 in the control group). In particular, normalization of hemodynamic parameters happened more often in the main group than in the control one (р=0.0026 for Fischer's Exact test, OR 10.7, 95% CI 2.0–80.0) (Table 3).
The treatment was well tolerated by all patients. At the time of physical therapy and afterwards no adverse reactions were noted. Among the patients from the main group no allergy response or infectious complications were noted after autologous PRP injections into endometrium using endoscopic needle under the control of hysteroscopy.
Discussion
Women with refractory ''thin'' endometrium comprise a challenging group of patients of ART clinics, since traditional methods of preparing of the endometrium for ET cycles do not provide desired effect, and insufficient endometrium growth causes ET cancellation as well as implantation failures [1]. Together with hormone therapy, physical therapy is widely used in Russia to prepare endometrium for ART programs. However, in some patients even numerous courses appear to be ineffective. Often, the only possibility of reproduction in patients with refractory ''thin'' endometrium is surrogacy, which is associated with financial, ethical and emotional challenges.
It is necessary to emphasize, that patients enrolled in the study had a number of confounding factors: long-term infertility, reproductive failures and multiple intrauterine interventions. Besides, the proportion of patients in the main group with a history of missed abortions and relevant surgical intrauterine interventions was much higher than in the control group.
The effectiveness of a new comprehensive approach to the treatment of women with infertility caused by refractory ''thin'' endometrium was demonstrated in this study. A targeted injection of autologous PRP into endometrium using endoscopic needle under the control of hysteroscopy promoted statistically significant endometrium thickness growth and improved uterine artery hemodynamics which was demonstrated by the control ultrasound scan, compared to the patients from the control group who underwent only a physiotherapeutic intervention.
Research data on correlation between uterine artery hemodynamic parameters and endometrium thickness is presented in a scientific literature [5, 9]. Our study reports worse visualization of uterine end arteries in patients with ''thin'' endometrium at the stage of enrollment comparing to hemodynamic parameters in healthy women. Standard criteria for healthy women was 100% visualization of basal arteries, and 71% – of spiral arteries using Doppler velocimetry [18].
Today one may find research publications on the intrauterine autologous PRP irrigation in addition to hormone therapy in patients with ''thin'' endometrium being prepared for ART cycles [15, 16]. However, this method has some constrictions associated with the absence of a unified protocol describing the use of various methods of autologous PRP production with no platelet concentration control. Apart from it, the infusion of autologous PRP (intrauterine irrigation) is mostly conducted without any visual control. Moreover, the doctor who proceeds with manipulations can use only 2–3 ml of PRP. As a result, there is a need in repeated blood sampling, PRP preparation and another intrauterine intervention in order to inject PRP and reach therapeutic effect. Our technology enables to use only 1 procedure of autologous PRP injections directly to disrupted endometrium areas of a patient under hysteroscopic control.
Conclusion
The absence of a universal effective approach to the therapy of patients with refractory ''thin'' endometrium determines the need for the search of new methods in the treatment of uterine factor infertility. The benefits of the new technology (PRP injection) makes it possible to visualize and evaluate uterine mucosa. It also helps to provide targeted manipulation with the most hypotrophic tissue areas and to administer sufficient volume of PRP cancelling the need of repeated interventions. Therefore, the results of this research allow us to recommend this new comprehensive approach to the therapy of patients with refractory ''thin'' endometrium before entering ART programs.
References
- Maekawa R., Taketani T., Mihara Y., Sato S., Okada M., Tamura I. et al. Thin endometrium transcriptome analysis reveals a potential mechanism of implantation failure. Reprod. Med. Biol. 2017; 16(2): 206-27. https://dx.doi.org/10.1002/rmb2.12030.
- Von Wolff M., Fäh M., Roumet M., Mitter V., Stute P., Griesinger G., Schwartz. A.K. Thin endometrium is also associated with lower clinical pregnancy rate in unstimulated menstrual cycles: A study based on natural cycle IVF. Front. Endocrinol. 2018; 9: 776. https://dx.doi.org/10.3389/fendo.2018.00776.
- Check J.H., Cohen R. Live fetus following embryo transfer in a woman with diminished egg reserve whose maximal endometrial thickness was less than 4 mm. Clin. Exp. Obstet. Gynecol. 2011; 38(4): 330-2.
- Mouhayar Y., Franasiak J.M., Sharara F.I. Obstetrical complications of thin endometrium in assisted reproductive technologies: a systematic review. J. Assist. Reprod. Genet. 2019; 36(4): 607-11. https://dx.doi.org/10.1007/s10815-019-01407-y.
- Basir G.S., Lam T.P., O W.S., Chau M.T., Ng E.H., Ho P.C. Cycle-to-cycle variation in utero-ovarian hemodynamic indices in ovarian stimulation cycles of the same women and its effects on the outcome of assisted reproduction treatment. Fertil. Steril. 2002; 78(5): 1055-60. https://dx.doi.org/10.1016/s0015-0282(02)03376-9.
- Kim A., Han J.E., Yoon T.K., Lyu S.W., Seok H.H., Won H.J. Relationship between endometrial and subendometrial blood flow measured by three-dimensional power Doppler ultrasound and pregnancy after intrauterine insemination. Fertil. Steril. 2010; 94(2): 747-52. https://dx.doi.org/10.1016/j.fertnstert.2009.03.084.
- Белоусов Д.М., Побединский Н.М. Значение нарушений гемодинамики в матке в генезе привычного невынашивания беременности I триместра. Акушерство и гинекология. 2006; 4: 27-30. [Belousov D.M., Pobedinskii N.M. The significance of hemodynamic disorders in the uterus in the genesis of habitual miscarriage of pregnancy in the first trimester. Obstetrics and gynecology/Akusherstvo i ginekologia. 2006; 4: 27-30. (in Russian)].
- Богданова А.М., Глухов Е.Ю., Дикке Г.Б. Применение низкочастотного ультразвука в комплексном лечении гипопластического варианта хронического эндометрита. Акушерство и гинекология. 2017; 2: 90-6. [Bogdanova A.M., Gluhov E.Yu., Dikke G.B. The use of low-frequency ultrasound in the complex treatment of hypoplastic variant of chronic endometritis. Akusherstvo i ginekologia/ Obstetrics and gynecology. 2017; 2: 90-6. (in Russian)]. http://dx.doi.org/10.18565/aig.2017.2.90-6.
- Волкова Е.Ю., Силантьева Е.С, Серов В.Н., Корнеева И.Е., Соколова Ю.Ю. Влияние физиотерапии на гемодинамику матки у женщин с нарушением репродуктивной функции и «тонким» эндометрием. Российский вестник акушера-гинеколога. 2012; 12(3): 50-4. [Volkova E.Yu., Silantieva E.S., Serov V.N., Korneeva I.E., Sokolova Yu.Yu. The effect of physiotherapy on uterine hemodynamics in women with impaired reproductive function and "thin" endometrium. Rossiiskii vestnik akushera-ginecologa/ Russian Bulletin of the obstetrician-gynecologist. 2012; 3: 50-4. (in Russian)]
- Mouhayar Y., Sharara F. Modern management of thin lining. Middle East Fertil. Soc. J. 2017; 22(1): 1-12. https://dx.doi.org/10.1016/j.mefs.2016.09.001.
- Urman B., Boza A., Balaban B. Platelet-rich plasma another add-on treatment getting out of hand? How can clinicians preserve the best interest of their patients? Hum. Reprod. 2019; 34(11): 2099-103. https://dx.doi.org/10.1093/humrep/dez190.
- Bendinelli P., Matteucci E., Dogliotti G., Corsi M.M., Banfi G., Maroni P., Desiderio M.A. Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: mechanisms of NF-κB inhibition via HGF. J. Cell. Physiol. 2010; 225(3): 757-66. https://dx.doi.org/10.1002/jcp.22274.
- Vishnyakova P., Artemova D., Elchaninov A., Efendieva Z., Apolikhina I., Sukhikh G., Fatkhudinov T. Effects of platelet-rich plasma on mesenchymal stem cells isolated from rat uterus. PeerJ. 2020; 8(5): e10415. https://dx.doi.org/10.7717/peerj.10415.
- Aghajanova L., Houshdaran S., Balayan S., Manvelyan E., Irwin J.C., Huddleston H.G., Giudice L.C. In vitro evidence that platelet-rich plasma stimulates cellular processes involved in endometrial regeneration. J. Assist. Reprod. Genet. 2018; 35(5): 757-70. https://dx.doi.org/10.1007/s10815-018-1130-8.
- Tandulwadkar S.R., Naralkar M.V., Surana A.D., Selvakarthick M., Kharat A.H. Autologous intrauterine platelet-rich plasma instillation for suboptimal endometrium in frozen embryo transfer cycles: A pilot study. J. Hum. Reprod. Sci. 2017; 10(3): 208-12. https://dx.doi.org/10.4103/jhrs.JHRS_28_17.
- Maleki-Hajiagha A., Razavi M., Rouholamin S., Rezaeinejad M., Maroufizadeh S., Sepidarkish M. Intrauterine infusion of autologous platelet-rich plasma in women undergoing assisted reproduction: A systematic review and meta-analysis. J. Reprod. Immunol. 2020; 137: 103078. https://dx.doi.org/10.1016/j.jri.2019.103078.
- Эфендиева З.Н., Аполихина И.А., Калинина Е.А., Федорова Т.А., Бакуридзе Э.М., Белоусов Д.М., Фатхудинов Т.Х., Сухих Г.Т. Первый опыт инъекционного введения аутологичной плазмы, обогащенной тромбоцитами, в эндометрий пациенток с маточным фактором бесплодия. Акушерство и гинекология. 2020; 4: 82-9. [Efendieva Z.N., Apolikhina I.A., Kalinina E.A., Fedorova T.A., Bakuridze E.M., Belousov D.M., Fatkhudinov T. Kh., Sukhikh G.T. The first experience of injecting autologous platelet-rich plasma into the endometrium of patients with uterine factor infertility. Akusherstvo i ginekologia / Obstetrics and gynecology. 2020; 4: 82-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.4.82-89.
- Кирющенков П.А., Белоусов Д.М. Ультразвуковая оценка роли «маточного фактора» и особенности предгестационной подготовки женщин с привычным невынашиванием беременности I триместра. Проблемы беременности. 2007; 13(5): 19-25. [Kiryushenkov P.A., Belousov D.M. Ultrasound assessment of the role of the "uterine factor" and the features of pre-gestational preparation of women with habitual miscarriage of pregnancy in the first trimester. Pregnancy problems. 2007; 13(5): 19-25 (in Russian)].
Received 14.01.2021
Accepted 31.03.2021
About the Authors
Inna A. Apolikhina, MD, Professor, Head of the Department of Aesthetic Gynecology and Rehabilitation, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia; Professor of the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Institute of Professional Education, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). E-mail: i_apolikhina@oparina4.ru.117997, Russia, Moscow, Ac. Oparina str., 4.
Zulfiya N. Efendieva, postgraduate fellow at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Institute of Professional Education, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). E-mail: efendievaz@yandex.ru. 119991, Russia, Moscow, Bolshaya Pirogovskaya str., 2/4.
Tatiana A. Fedorova, MD, Professor, Head of the Department of Transfusiology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. E-mail: t_fyodorova@oparina4.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Dmitrii M. Belousov, PhD, Clinical Head of Ultrasound and Functional Diagnostics Department, echography expert, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. E-mail: slides@narod.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Polina A. Vishnyakova, PhD, senior researcher, Laboratory of Regenerative Medicine, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. E-mail: p_vishnyakova@oparina4.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Daria A. Artemova, junior researcher, Laboratory of Growth and Decision, Scientific Research Institute of Human Morphology.
E-mail: artiomova.darya@yandex.ru. 117418, Russia, Moscow, Tsyurupy str., 3.
Timur Kh. Fatkhudinov, PhD, MD, leading researcher, Laboratory of Regenerative Medicine, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia; Deputy Director for scientific development, Scientific Research Institute of Human Morphology.
E-mail: tfat@yandex.ru. 117997, Russia, Moscow, Ac. Oparina str. 4.
For citation: Apolikhina I.A., Efendieva Z.N., Fedorova T.A., Belousov D.M., Vishnyakova P.A., Artemova D.A., Fatkhudinov T.Kh. Autologous platelet rich plasma
in complex therapy of women with refractory ‘‘thin’’ endometrium.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2021; 4: 112-119 (in Russian)
https://dx.doi.org/10.18565/aig.2021.4.112-119



