Waterjet dissection in the surgical treatment of invasive cervical cancer: functional results
Relevance: Despite the accumulated experience in nerve-sparing pelvic surgery, the rate offunctional postoperative complications remains unsatisfactory. Therefore, developing and implementing new surgical approaches may facilitate the surgeon's work and reduce the complication rate. One of these technologies is waterjet surgery. The main advantage of this technique is the selective isolation and preservation of nerve fibers and blood vessels with minimal deformation of the surrounding tissues in the absence of thermal exposure. Objective: To evaluate the functional outcomes in patients with stages IB1—IIB cervical cancer undergoing type C1 radical hysterectomy (nerve-sparing radical hysterectomy) using a waterjet dissector. Materials and methods: The study group included 30 patients who underwent extended type C1 radical hysterectomy using a waterjet dissector. Fifty-two patients of the control group underwent extended type C2 radical hysterectomy. Results: The use of the waterjet dissection in the study group resulted in reduced duration of the postoperative catheterization (2 [2;3] days versus 16 [11.5;20] days) and a shorter time to a postvoid residual volume of urine less than 100 ml (3 [3;4] days versus 21 [20; 25] days) (p<0.001). In the study group, no patient in the postoperative period showed clinical signs of neurogenic bladder dysfunction. Conclusion: Using the waterjet dissection in patients undergoing type C1 radical hysterectomy results in restoration of lower urinary tract functions in a shorter time.Meshkova M.A., Mukhtarulina S.V., Maltsagova Kh.R., Novikova E.G., Kaprin A.D.
Keywords
Aiming to minimize postoperative functional complications, the Japanese school of gynecological oncologists first developed the concept of a nerve-sparing approach in radical surgery for invasive cervical cancer. For example, Kobayashi T. modified the original Okabayashi's radical hysterectomy (1921) and in 1961 described the technique of nerve-sparing hysterectomy based on preserving the inferior hypogastric nerves and pelvic plexus branches by dissecting the lateral parametrium [1]. The surgical technique of systematic preservation of pelvic autonomic nervous system (ANS) elements was further improved and described in detail in the works of Japanese onco-gynecologists such as S. Takizawa (1988) [2], N. Sakuragi et al. (2005) [3].
Over the last decade, more than 100 studies have been published in the international literature confirming that preserving pelvic ANS elements can significantly reduce the number of postoperative functional urogenital system disorders while maintaining a high level of long-term oncological outcomes [5, 6-8].
Despite the accumulated experience in pelvic neurosurgery, the rate of functional postoperative complications remains unsatisfactory (9). Therefore, the development and introduction of new surgical approaches can simplify the surgeon's work and reduce complication rates. One such technique is waterjet tissue dissection. The main advantage of this method is selective dissection and preservation of nerve fibers and vessels with minimal deformation of the surrounding tissue in the absence of thermal effects.
This study aimed to evaluate the functional outcomes in patients with stages IB1–IIB cervical cancer undergoing type C1 radical hysterectomy (nerve-sparing radical hysterectomy) using a waterjet dissector. This article presents the first Russian experience of waterjet dissection in extended C1-type radical hysterectomy in patients with invasive cervical cancer.
Materials and methods
The study included 82 patients with morphologically verified stage IB1-IIB cervical cancer who underwent extended radical hysterectomy for invasive cervical cancer in 2017–2021 at the Department of Gynecologic Oncology of P.A. Hertsen Moscow Oncology Research Center and the Department of Gynecology with Chemotherapy, N.A. Lopatkin Research Institute of Urology and Interventional Radiology – branches of the NMRRC, Ministry of Health of Russia.
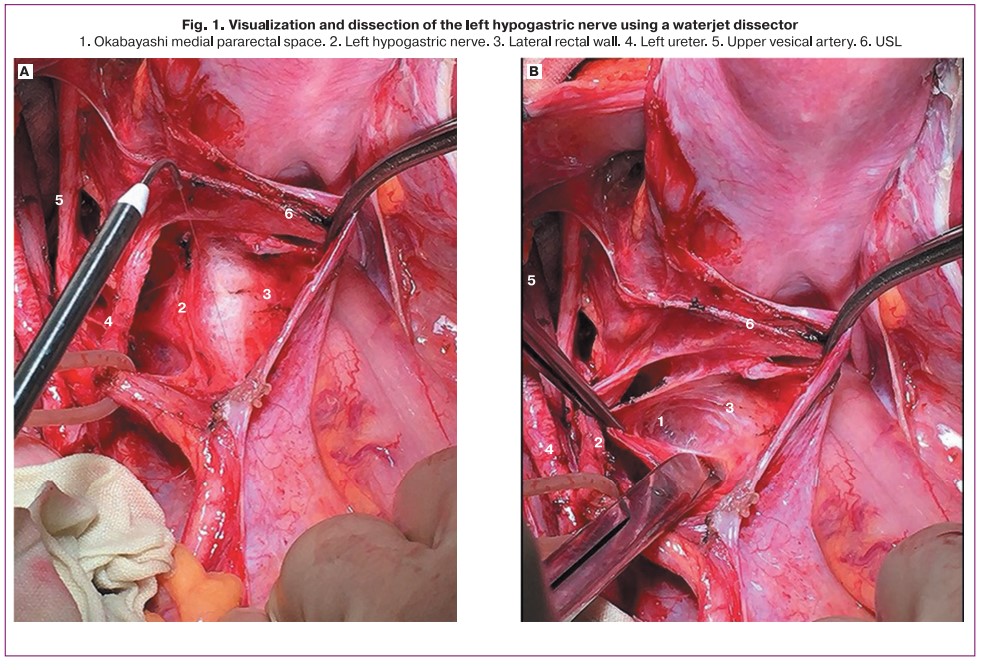
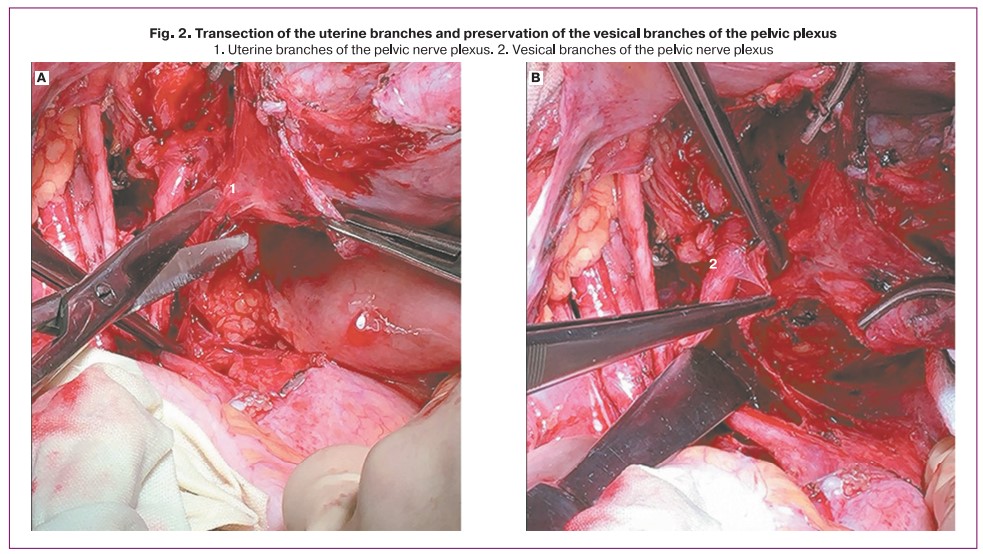
The study group consisted of 30 patients who underwent extended C1-type radical hysterectomy with pelvic and para-aortic lymphadenectomy with a waterjet dissection using the ERBEJET2 unit. The application of the water jet dissector was started at the opening of the medial pararectal space (Okabayashi space). The proximal part of the inferior hypogastric plexus was visualized on the lateral surface of the sacroiliac ligament (SIL). A jet of 0.1 mm water with a 20–35 bar pressure was directed parallel to the SIL plane, 3–5 mm from the visualized nerve plexus. The hypogastric nerve was exposed from the sacral promontory to the point of intersection with the uterine vessels, after which the SIL was excised. After the deep uterine vein transection, waterjet dissection of the pelvic or inferior hypogastric plexus located on the lateral vaginal fornix in the paravaginal tissue was performed (Fig. 1). The vesicular branches of the pelvic plexus were then isolated from the vesicouterine ligament (V.L.) using a waterjet dissector; then, the V.L. was transected under visual control of the pelvic plexus vesicular branches. The pelvic plexus was displaced laterally after transecting the uterine branches (Fig. 2).
The control group included 52 patients who underwent type 2 radical hysterectomy with pelvic and para-aortic lymphadenectomy. The study inclusion criteria were stages IB1–IIB cervical cancer, general overall ECOG PS 0–1, absence of preoperative radiation and/or chemotherapy, marked urodynamic abnormalities, and urinary tract pathology. The exclusion criteria were distant metastases at the preoperative examination, gross functional disorders or malformations of the urinary system, and previous urinary system surgical interventions.
The main parameters to be assessed were intraoperative findings, the mean duration of the postoperative catheterization, the postvoid residual urine volume (PVR) <100 ml, and the neurogenic bladder dysfunction in the postoperative period.
Statistical analysis
Statistical analysis was performed using R (version 3.2, R Foundation for Statistical Computing, Vienna, Austria). The distribution of continuous variables was tested for normality using the Shapiro–Wilk test. Descriptive statistics included mean ± standard deviation [(M (S.D.)], median and quartiles [Me (Q1; Q3)], and minimum and maximum values. Group medians were compared by the Mann-Whitney test; frequencies were compared by the Fisher exact test. Differences between the groups were considered statistically significant at p<0.05.
Results
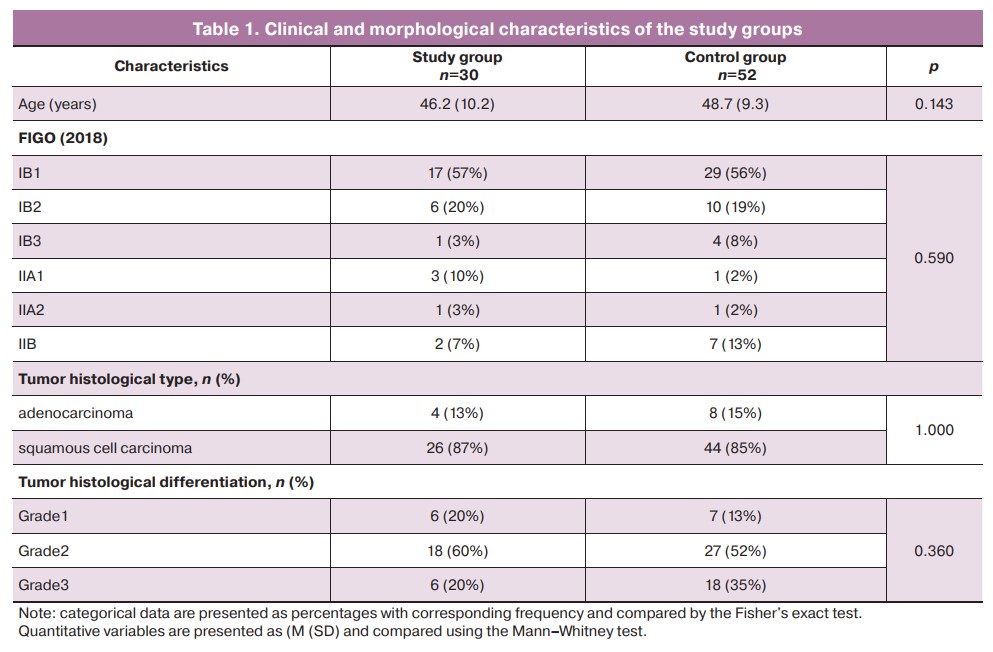
The mean age of patients in the study and control groups was 46.7(11.8) and 48.7(9.3) years, respectively. In the study group, 24/30 (80%), 4/30 (13%), and 2/30 (7%) patients had FIGO (2018) stages IB, IIA, and IIB, respectively. In the control group, 43/52 (83%), 2/52 (4%), and 7/52 (13%) patients had FIGO stages IB, IIA, and IIB, respectively.
Morphological examination of the material in the study group showed squamous cell carcinoma in 26/30 (87%) and adenocarcinoma in 4/30 (13%) patients. The squamous cell tumor type also prevailed in the morphological structure in 44/52 (85%) cases in the control group. There were no significant differences in clinical and morphological characteristics between the study and control groups (Table 1).
As for the main intraoperative findings, waterjet dissection in the study group resulted in a statistically significant reduction in operation time (180 [160; 200] min vs. 300 [225; 345] min), (p<0.001). Mean blood loss was 100 [100; 140] ml in the study group compared to 712 [525; 875] ml in the control group (p<0.001). Mean intraoperative hemoglobin was 115 [105; 125] g/l in the study group and 103 [98; 108] g/l in the control group, (p<0.001) (Table 2).
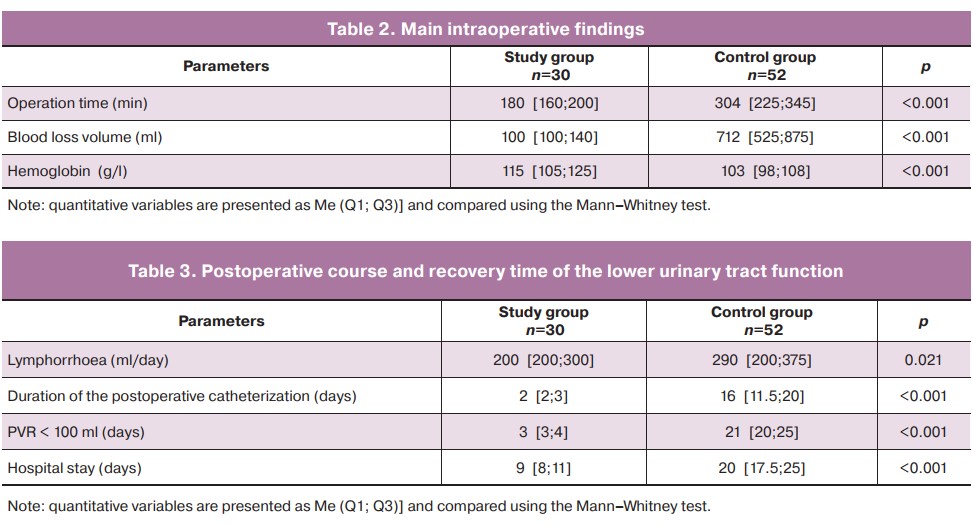
Use of waterjet dissection in the study group the reduced duration of the postoperative catheterization (2 [2; 3] days versus 16 [11.5; 20] days) (p<0.001) and a shorter time to PVR of less than 100 ml (3 [3; 4] days versus 21 [20; 25] days) (p<0.001). In the study group, no patient showed clinical signs of neurogenic bladder dysfunction in the postoperative period. In contrast, in the control group, 26.2% of the patients had manifestations of neurogenic bladder dysfunction (p<0.001) (Table 3).
Hospital length of stay was 9 [8; 11] and 20 [17.5; 25] days in the study and control group, respectively (p<0.001).
Discussion
To date, no standardized technique for nerve-sparing radical hysterectomy has been described in the guidelines for the treatment of cervical cancer [10]. There is also no standardized approach for visualizing and identifying nerve fibers, and all techniques are authored and used in the same clinic [11]. Original methods of neurosurgical hysterectomy are presented in the works of many Japanese gynecological oncologists based on a detailed study of the anatomical elements of the pelvic nerve plexuses [3, 4, 12, 13].
The proposed techniques varied concerning the different classification systems. For example, in the Piver type III nerve plexus, it is difficult for the surgeon to identify the inferior hypogastric plexus. And the Querleu-Morrow classification (2008) and the TMMR (Total mesometrial resection) method proposed by Höckel M. et al. do not specify a role for the vesicovaginal ligament, which has been criticized by several authors [14–16].
The cornerstone of pelvic nerve plexus preservation is a clear definition of the boundaries of parametrial resection [17]. The surgical anatomy of the retroperitoneal nerve plexuses has been demonstrated in most detail by D. Cibula et al. in a new classification system for radical hysterectomy. The boundaries of the parametrial resection were defined in horizontal and vertical sections for the ventral, lateral, and dorsal parametrium to form a distinctive three-dimensional anatomical picture. Most of the authors' techniques of nerve-sparing hysterectomy describe the anatomical landmarks presented in this classification. Thus, according to the C1 type classification by D. Cibula et al. (2011), when the ureter is exposed, the «roof of the tunnel» is transected. It is exposed from the lateral and partially from the ventral parametrium (1–2 cm). The vertical border of the ventral parametrium resection is the vesicular branches of the inferior hypogastric plexus. The horizontal excision line of the lateral parametrium runs along the medial edge of the internal iliac artery and vein. The vertical border of the lateral parametrium dissection is at the level of the deep uterine vein. At this site, the underlying layers of the lateral parametrium contain the branches of the pelvic ANS. As for the ventral parametrium, the horizontal excision line is at the site of RUL attachment to the rectum, and the vertical boundary is the pelvic plexus and hypogastric nerve. This classification, therefore, details the parametrial resection's boundaries to allow precise isolation and preservation of the pelvic ANS [18].
In 2007, Fujii et al. presented their experience with the Okabayashi modification of neurosurgery, detailing the technical aspects to preserve the pelvic autonomic nervous system elements. The authors identified vascular landmarks allowing visualization of nerve plexuses. For example, precise exposure of the deep uterine vein at the border of the cervix and the lateral arch of the upper third of the vagina enables the preservation of the inferior hypogastric plexus fibers, and identification of the inferior vesical vein and artery helps to visualize the pelvic plexus branches running to the posterior wall of the bladder [4]. In a study by Possover et al. of the University of Jena, Germany, the authors describe a vascular landmark such as the middle rectal artery at the level of the origin of the internal iliac artery, which divides the plane of the cardinal ligament into vascular and neural parts [19].
In this article, we describe an original technique of C1-type radical hysterectomy using waterjet dissection, which significantly reduces the incidence of postoperative urinary tract functional complications. The domestic literature describes the experience of successful application of waterjet dissection as a new method of anatomical tissue dissection in oncourology by D.Y. Pushkar et al. [20] and coloproctology by D.V. Sidorov et al. [21].
However, there are no domestic studies devoted to applying this technology in the surgery of female reproductive system tumors. To date, the only randomized study of the use of waterjet dissection in nerve-sparing extended radical hysterectomy has been described in the world literature [22]. The authors compared urodynamic findings after laparoscopic nerve-sparing extended radical hysterectomy using a waterjet dissector (treatment group) and standard laparoscopic nerve-sparing extended radical hysterectomy (control group). Neurogenic bladder dysfunction was observed in 7 patients (8.8%) in the control group and 4 (3.8%) in the study group (p=0.349). No statistically significant differences were found between the control and treatment groups' overall and recurrence-free survival rates. This study allowed the authors to conclude that using waterjet dissection in nerve-sparing extended hysterectomy leads to a more rapid recovery of urinary function in the postoperative period without affecting patients' survival rate.
Thus, further study of the promising technique with the waterjet dissector is necessary to optimize the functional results in patients with invasive cervical cancer.
Conclusion
The analysis of the initial findings suggests that the use of waterjet in tissue dissection contributes to a simplified visualization of nerve fibers and, consequently, the most atraumatic exposure of pelvic autonomic nerve plexuses. Therefore, waterjet dissection in patients undergoing type C1 radical hysterectomy results in restoration of lower urinary tract functions in a shorter time.
References
- Kobayashi T. Abdominal radical hysterectomy with pelvic lymphadenectomy for cancer of cervix. Tokyo, Japan: Nanzando; 1961: 178-87.
- Sakamoto S., Takizawa K. An improved radical hysterectomy with fewer urological complications and with no loss of therapeutic results for invasive cervical cancer. Baillieres Clin. Obstet. Gynaecol. 1988; 2(4): 953-62. https://dx.doi.org/10.1016/s0950-3552(98)80022-9.
- Sakuragi N., Todo Y., Kudo M., Yamamoto R., Sato T. A systematic nerve-sparing radical hysterectomy technique in invasive cervical cancer for preserving postsurgical bladder function. Int. J. Gynecol. Cancer. 2005; 15(2): 389-97. https://dx.doi.org/10.1111/j.1525-1438.2005.15236.x.
-
Fujii S., Takakura K., Matsumura N., Higuchi T., Yura S., Mandai M. et al.
Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol. Oncol. 2007; 107(1): 4-13.
https://dx.doi.org/10.1016/j.ygyno.2007.08.076.
- Cao T.T., Wen H.W., Gao Y.N., Lyu Q.B., Liu H.X., Wang S. et al. Urodynamic assessment of bladder storage function after radical hysterectomy for cervical cancer. Chin. Med. J. (Engl). 2020; 133(19): 2274-80. https://dx.doi.org/10.1097/CM9.0000000000001014.
- Muallem M.Z., Armbrust R., Neymeyer J., Miranda A., Muallem J. Nerve sparing radical hysterectomy: short-term oncologic, surgical, and functional outcomes. Cancers (Basel). 2020; 12(2): 483. https://dx.doi.org/10.3390/cancers12020483.
- Li L., Ma S., Tan X., Zhong S., Wu M. Surgical, urinary, and survival outcomes of nerve-sparing versus traditional radical hysterectomy: A Retrospective Cohort Study in China. Am. J. Clin. Oncol. 2019; 42(10): 783-8. https://dx.doi.org/10.1097/COC.0000000000000593.
- Tsunetoh S., Terai Y., Takai M., Fujiwara S., Tanaka Y., Tanaka T. et al. Urodynamic outcomes after pelvic nerve-sparing radical hysterectomy with or without neoadjuvant chemotherapy. 2019; 10(50): 5207-16. https://dx.doi.org/10.18632/oncotarget.27147.
- Suvorova V.A., Dobrokhotova Yu.E., Ilyina I.Yu., Venediktova M.G., Sarantsev A.N., Morozova K.V. Genitourinary Disorders after Combined and Complex Treatment of the Female Genital Organs Cancer. Obstetrics and Gynecology. 2016; 11: 28-33. (in Russian). https://dx.doi.org/10.18565/aig.2016.11.28-33.
- Kietpeerakool C., Aue-Aungkul A., Galaal K., Ngamjarus C., Lumbiganon P. Nerve-sparing radical hysterectomy compared to standard radical hysterectomy for women with earle stage cervical cancer (stage Ia2 to IIa). Cochrane Database Syst. Rev. 2019; (2): CD012828. https://dx.doi.org/10.1002/14651858.CD012828.pub2.
- Nagai T., Niikura H., Kurosawa H., Tanaka S., Otsuki T., Utunomiya H. et al. Individualized radical hysterectomy procedure using intraoperative electrical stimulation for patients with cervical cancer. Int. J. Gynecol. Cancer. 2012; 22(9): 1591-6. https://dx.doi.org/10.1097/IGC.0b013e31826fd684.
-
Kuwabara Y., Suzuki M., Hashimoto M., Furugen Y., Yoshida K., Mitsuhashi N. New method to prevent bladder dysfunction after radical hysterectomy for uterine cervical cancer. J. Obstet. Gynaecol. Res. 2000; 26(1): 1-8.
https://dx.doi.org/10.1111/j.1447-0756.2000.tb01192.x.
- Sato K., Sato T. The vascular and neuronal composition of the lateral ligament of the rectum and the rectosacral fascia. Surg. Radiol. Anat. 1991; 13: 17-22. https://dx.doi.org/10.1007/BF01623135.
-
Höckel M. Total mesometrial resection: nerve-sparing extended radical abdominal hysterectomy. Zentralbl. Gynakol. 2001; 123(5): 245-9.
https://dx.doi.org/10.1055/s-2001-14786.
- Querleu D., Morrow C.P. Classification of radical hysterectomy. Lancet Oncol. 2008; 9(3): 297-303. https://dx.doi.org/10.1016/S1470-2045(08)70074-3.
- Sakuragi N., Murakami G., Konno Y., Kaneuchi M., Watari H. Nerve-sparing radical hysterectomy in the precision surgery for cervical cancer. J. Gynecol. Oncol. 2020; 31(3): e49. https://dx.doi.org/10.3802/jgo.2020.31.e49.
-
Kaprin A.D., Novikova E.G., Mukhtarulina S.V. Comparison of different classifications of radical hysterectomies: complication or help in understanding? P.A. Herzen Journal of Oncology. 2016; 5(4): 63-71. (in Russian).
https://dx.doi.org/10.17116/onkolog20165463-71.
-
Cibula D., Abu-Rustum N.R., Benedetti-Panici P., Köhler C., Raspagliesi F., Querleu D., Morrow C.P. New classification system of radical hysterectomy: emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol. Oncol. 2011; 122(2): 264-8. https://dx.doi.org/10.1016/
ygyno.2011.04.029.
- Possover M., Stöber S., Plaul K., Schneider A. Identification and preservation of the motoric innervation of the bladder in radical hysterectomy type III. Oncol. 2000; 79: 154-7. https://dx.doi.org/10.1006/gyno.2000.5919.
- Puchkar D.Yu., Kolontarev K.B., Govorov A.V., Rasner P.I., Diakov V.V., Bernikov A.N., Bormotin A.V. Experience of hydrodissection for preservation of neurovascular bundle during robot-assisted radical prostatectomy. In: Materials of the XII Congress of the Russian Society of Urologists. Moscow, September 18–21, 2012. M.; 2012: 75-6. (in Russian).
- Sidorov D.V., Lozhkin M.V., Petrov L.O., Grishin N.A., Troitskiy A.A., Isaeva A.G. Surgical and pathomorphological results of total mesorectumectomy by using water-jet dissection technique in patients with rectal cancer. Oncological Coloproctology. 2016; 6: 17-22. (in Russian).
- Li L., Ma S., Tan X., Zhong S., Wu M. The urodynamics and survival outcomes of different methods of dissecting the inferior hypogastric plexus in laparoscopic nerve-sparing radical hysterectomy of type C: A randomized controlled study. Ann. Surg. Oncol. 2019; 26(5): 1560-8. https://dx.doi.org/10.1245/s10434-019-07228-8.
Received 31.08.2021
Accepted 20.12.2021
About the Authors
Maria A. Meshkova, Ph.D. Student, P.A. Hertsen Moscow Oncology Research Center - branch of the NMRRC, Ministry of Health of Russia, +7(937)065-81-20, mari.meshkova.95@mail.ru, 125284, Russia, Moscow, 2nd Botkinsky str., 3.Svetlana V. Mukhtarulina, Dr. Med. Sci., Head of the Oncogynecology Department, N.A. Lopatkin Research Institute of Urology and Interventional Radiology - branch of the NMRRC, Ministry of Health of Russia, +7(916)148-27-13, svmukhtarulina@yandex.ru, 105425, Russia, Moscow, 3rd Parkovaya str., 51.
Heda R. Maltsagova, Oncologist at the Department of Gynecology with Chemotherapy, N.A. Lopatkin Research Institute of Urology and Interventional Radiology - branch of the NMRRC, Ministry of Health of Russia, +7(925)157-67-40, heda16@inbox.ru, 105425, Russia, Moscow, 3rd Parkovaya str., 51.
Elena G. Novikova, Dr. Med. Sci., Professor, Merited Scholar of the Russian Federation, Head of the Department of Reproductive and Urinary Tract Tumors, P.A. Hertsen Moscow Oncology Research Center - branch of the NMRRC, Ministry of Health of Russia, 125284, Russia, Moscow, 2nd Botkinsky str., 3.
Andrei D. Kaprin, Director General of the NMRRC of Ministry of Health of Russia, Director of P.A. Hertsen Moscow Oncology Research Center, Chief Non-staff Oncologist of Ministry of Health of Russia, 125284, Russia, Moscow, 2nd Botkinsky str., 3.
Authors' contributions: Kaprin A.D., Mukhtarulina S.V., Novikova E.G. - conception and design of the study; Mukhtarulina S.V., Meshkova M.A. - review of the relevant literature, statistical analysis; Maltsagova Kh.R. - material collection and processing. Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Meshkova M.A., Mukhtarulina S.V., Maltsagova Kh.R., Novikova E.G., Kaprin A.D. Waterjet dissection in the surgical treatment of invasive cervical cancer: functional results.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 1:122-128 (in Russian)
https://dx.doi.org/10.18565/aig.2022.1.122-128