Treatment of obstetric ruptures of pubic symphysis and dysfunctions of the pubic articulation
Objective. To conduct an analysis of clinical cases of dysfunction of the pannus joint and its traumatic ruptures with the definition of treatment tactics.Yavorskaya S.D., Plotnikov I.A., Bondarenko A.V., Olimova A.O., Plotnikova I.V.
Materials and methods. In KGBU, Maternity Hospital No. 2 between 2011 and 2016, DLD was registered in 123 women, which was 0.5% of all deliveries at the medical facility (22691) for the indicated period. For the diagnosis of DLS, in addition to assessing the pain syndrome on an analog scale and clinical data, ultrasound examination of the pinnate joint (ultrasound) was used. When suspicion of a traumatic rupture of the symphysis of the symphysis in labor, pelvic radiography was performed.
Results. The frequency of DLS in parturient women for 6 years averaged 0.5%. In 12 patients with I diastasis of the lobed branches, a pubic symphysis ruptured during childbirth. The magnitude of diastase between the branches of the bones, measured during a single study, did not always correspond to the severity of the pain syndrome in DLS.
Conclusion. The use of conservative treatments for rupture of the pubic joint allows restoring the integrity of the pelvic ring with a good functional result.
Keywords
It has been known since Hippocrates that during pregnancy moderate molaxation of pelvic joints and distension of pubic symphysis occur for favorable passage of the fetus through the birth canal. Sometimes these processes go beyond physiology and are accompanied by severe pain syndrome, gait disturbance, discomfort or even joint rupture in labour. In national literature this condition is named symphysitis or symphysiopathy, besides, there are no clear criteria to distinguish these terms [1]. Abroad this pathological condition is called symphysis pubis disfunction (SPD) [2-5].
SPD during pregnancy occurs in 0.12-56% of women [6-8]. Such huge frequency fluctuations can be explained by lack of single definition of this pathological condition and insufficient attention to this problem. We failed to detect in available literature objective criteria of indications for cesarean section in case of SPD and management tactics for patients with traumatic rupture of symphysis pubis in labour. The aim of this study was to analyze clinical cases of SPD and its traumatic ruptures to determine treatment tactics.
Materials and Methods
Retrospective open monocentric study was conducted and included 123 pregnant women with SPD diagnosed the day before labor. All patients were delivered in the second level maternity hospital (Regional State Budgetary Health Care Institution Maternity hospital №2 – clinical base of the Department of Obstetrics and Gynecology with additional professional education course, Altai State Medical University) in period of 2011-2016. The age of patients ranged from 18 to 42 years (mediana was 26 years), interquartile range was from 19 to 37 years.
Fifty-four women (43.9%) were primiparous, and sixty-nine women (56.1%) were multiparous. Three multiparous patients (4.3%) had symphysitis in previous delivery. The pregnant women had the following antropometric characteristics: height mediana - 167 cm, Solovyev index – 16 cm, size of large pelvis in 123 patients corresponded to physiological norms. Different variants of neurocirculatory dystonia (48.8%) and obesity (26.8%) were most common somatic diseases. Gestational complications such as arterial hypertension without proteinuria were diagnosed in every fourth woman (19.5%), placental dysfunction by doppler ultrasound was determined in 17.9% cases, cervical insufficiency and cervical cerclage in 1.6% of cases.
SPD was characterized by pain in the area of the pubic symphysis, nagging pain in the lower part of the abdomen and sacroiliac joint (most often on one side when changing body position), sleep disturbance due to pain syndrome. It is often noted waddling or “duck” gait while walking. Soreness in the area of the pubic symphysis, positive Larrey and Verneyl symptoms were determined by palpation. Sometimes the slit between the pubic bones was palpated.
In addition to pain syndrome evaluation using analogue scale [9] and clinical data, symphyseal ultrasonography was used to diagnose SPD. Suggesting traumatic rupture of the pubic symphysis during delivery, pelvic radiography was performed. SPD was detected when the interpubic distance in pregnancy or after delivery was widened by more than 10 mm at the narrowest point.
 Results and Discussion
Results and Discussion
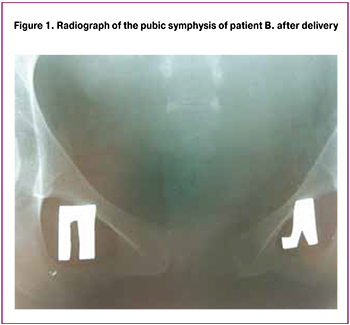
There were 22,691 deliveries in clinical maternity hospital from 2011 to 2016. The frequency of SPD was 0.5% (Table). It should be noted that SPD syndrome increases every year. In our opinion, it is mostly connected with diagnostic improvement and alertness of the obstetricians during examination. The most common clinical manifestation was pelvic pain which all patients experienced (100%), but pain syndrome had different intensity. Eighty-six patients (70%) complained of excruciating pain and decline in quality of life, but thirty-seven women (30%) felt moderate pain and discomfort in the area of the pubic symphysis. Most often pain syndrome appeared from 32 to 39 weeks of gestation and was progressive.
During the examination by orthopedist-traumatologist, gait disturbance was determined in 10.5% of cases, “duck-like gait” in 2.4% of cases. On palpation, tenderness of the pubic symphysis was revealed in every third patient (32.5%), “sticky heel” symptom – in five patients (4.1%), “compression and tension of pelvic ring” symptom – in twenty patients (16.2%).
All pregnant women underwent symphyseal ultrasonography. It should be noted that the separation gap between branches of the pubic bones measured by single study did not always correspond to the severity of pain syndrome in case of SPD. Most authors differ three stages of symphysis pubis diastasis. If the separation gap between branches of the pubic bones is from 5 to 10 mm, it refers to I stage, from 10 to 20 mm – II stage, more than 20 mm – III stage. In absence of pain syndrome it is physiological I stage, II and III stages are pathological [1,2].
Symphysis pubis diastasis that was less than 10 mm and revealed by ultrasound (I stage) with pain syndrome was observed in forty-six patients (37.4%) in case of SPD, from 11 to 20 mm (II stage) – in seventy-seven patients (62.6%). There were no cases with interpubic distance more than 20 mm during pregnancy.
Considering recommendations of National Guidelines of Obsterics [11], one of indications for cesarean section is severe pain syndrome. Therefore, all pregnant women with symphysis pubis diastasis more than 10 mm, II stage (62.6%) underwent cesarean section. Forty-six patients (37.4%) had vaginal delivery.
A total of 124 babies were born. All of them had Apgar score 8, average weight 3648 g and average height 52 cm. Macrosomic fetuses (more than 4 kg) were delivered in 12% by caesarean section. One pregnant woman with twins was also delivered by operation.
Twelve patients (26.1%) who had vaginal delivery had symphyseal rupture in the second stage of labor. All of them experienced a kind of click in the pubis area when the fetus was passaging through the birth canal. Sonograms and skiagrams showed significant widening of the pubic symphysis. In other cases physiological labor was without any peculiarities, and symptoms of SPD disappeared in 3-5 days.
In case of symphyseal rupture in labor all patients experienced cracking pain in the area of the pubic symphysis, they could not turn in bed and raise the heel of the unbent leg. The magnitude of separation does not always correlate well to the severity of clinical features during pregnancy. It should be noted that ten patients with traumatic rupture of the pubic symphysis felt minor pubic pain and moderate discomfort before delivery. Only two patients suffered from severe pain in pubic area and gait disturbance, but they refused cesarean section.
All cases of traumatic symphyseal rupture were treated conservatively. Patients were recommended bed rest during 3 weeks, pelvic girdle, analgesics and physiotherapy. All women noticed regress of pain syndrome on the second week of the treatment and active mobilization with gradual full load on the fourth week. As a rule all patients could move without any additional support tools by 6 week after labor, the pain syndrome was absent.
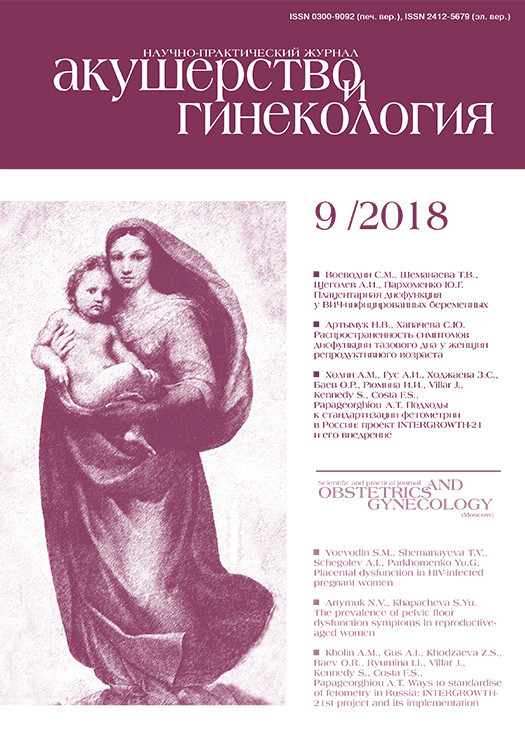
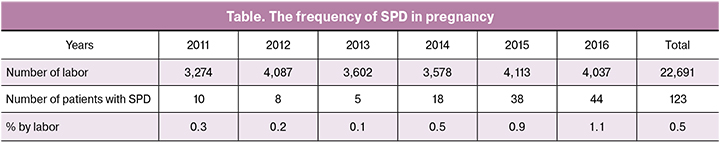
 Case report one. Patient B., a 28-year-old woman was referred to the hospital with gestational age 39 weeks 3 days. She had chronic compensated placental insufficiency, hypotonic type of neurocirculatory dystonia and thrombophilic gene polymorphism PAI-1 4G/5G. On admission to the hospital she complained of moderate pain and discomfort in the area of pubic symphysis. The patient had the following anthropometric data: height – 165 cm, weight – 78 kg, pelvic sizes - Ds.sp. – 25 cm, Ds.cr. – 28.5 cm, Ds.tr. – 31 cm, Conjugata externa – 21 cm, Solovyev index – 13.5 cm. Symphysis pubis diastasis was 8 mm by ultrasound. The symphyseal rupture with 28 mm separation of the pubic bones occurred during spontaneous delivery (Fig. 1). It should be noted that the labor lasted 8 hours. Anthropometric data of the neonate: height – 53 cm, weight – 3672 g. After delivery this patient was recommended bed rest during 3 weeks, analgesics and pelvic girdle. She was mobilized on the fourth week, in 5 weeks her gait restored, pain syndrome disappeared, there was no necessity of the girdle. During the control examination, pelvic ring displacement was not revealed. The skiagram showed separation between branches of the pubic bones less than 8 mm (Fig. 2).
Case report one. Patient B., a 28-year-old woman was referred to the hospital with gestational age 39 weeks 3 days. She had chronic compensated placental insufficiency, hypotonic type of neurocirculatory dystonia and thrombophilic gene polymorphism PAI-1 4G/5G. On admission to the hospital she complained of moderate pain and discomfort in the area of pubic symphysis. The patient had the following anthropometric data: height – 165 cm, weight – 78 kg, pelvic sizes - Ds.sp. – 25 cm, Ds.cr. – 28.5 cm, Ds.tr. – 31 cm, Conjugata externa – 21 cm, Solovyev index – 13.5 cm. Symphysis pubis diastasis was 8 mm by ultrasound. The symphyseal rupture with 28 mm separation of the pubic bones occurred during spontaneous delivery (Fig. 1). It should be noted that the labor lasted 8 hours. Anthropometric data of the neonate: height – 53 cm, weight – 3672 g. After delivery this patient was recommended bed rest during 3 weeks, analgesics and pelvic girdle. She was mobilized on the fourth week, in 5 weeks her gait restored, pain syndrome disappeared, there was no necessity of the girdle. During the control examination, pelvic ring displacement was not revealed. The skiagram showed separation between branches of the pubic bones less than 8 mm (Fig. 2).
Based on case report one, conservative treatment should be used in rotary displacement in one of the planes which takes place in symphyseal ruptures in labor. Such method may restore the pelvic ring structure and function in short term without high risk.
Ultrasound for evaluation of the pubic bones separation in case of SPD has great advantages over other objective methods. But single examination of the pubic symphysis does not reflect the pathological process in general. SPD requires physical examination of the patient and ultrasound evaluation of diastasis in the third trimester not less than once every three weeks.
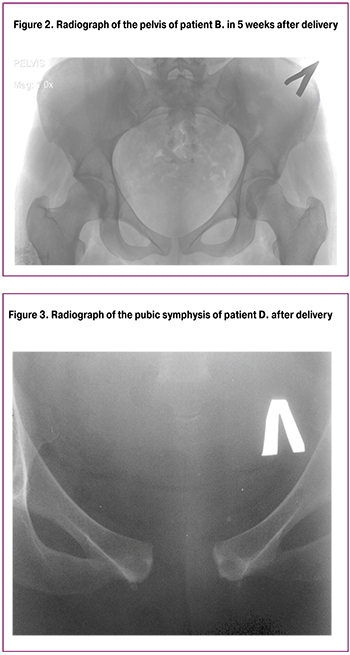
Case report two. A 25-year-old patient D. with aggravated obstetric history was admitted to the hospital with gestational age 39 weeks 5 days. She had compensated placental dysfunction without circulatory disorder, moderate polyhydramnios, gestational pyelonephritis in remission and mild anemia. Anthropometric data of the patient were height – 172 cm, weight – 76 kg, pelvic sizes - Ds.sp. – 24.5 cm, Ds.cr. – 28 cm, Ds.tr. – 30 cm, Conjugata externa – 20 cm, Solovyev index – 14 cm. In the beginning of the third trimester woman experienced pain in the area of pubic and left sacroiliac joints, gait disturbance. At 32 weeks she consulted orthopedist-traumatologist and symphysis pubis diastasis was not more than 7 mm by ultrasound. At 36 weeks pain syndrome increased and another sonogram showed 9 mm of diastasis. One week before delivery the separation gap between the pubic bones was 10 mm by ultrasound. The patient refused cesarean section categorically. Symphyseal rupture with 27 mm separation of the pubic bones occurred during delivery (Fig. 3). The labor lasted 9 hours 35 minutes. Anthropometric data of the neonate were height – 54 cm, weight – 3820 g. The woman was recommended bed rest during 3 weeks, analgesics and pelvic girdle. She was mobilized in four weeks, pain syndrome disappeared. After six-week postpartum her gait restored, she moved without the pelvic girdle. The symptoms of pelvic ring displacement were not revealed. The control skiagram showed a gap in the area of the pubic symphysis with the distance between the two bones of 8 mm.
The second case shows that despite the small symphysis pubis diastasis (10 mm), symphyseal rupture (its risk seemed to be low) still occurred in labor. However, according to the dynamic ultrasound the separation of the pubic symphysis increased and was accompanied by severe pain syndrome which cannot be underestimated. Therefore, all patients with dynamic increase of symphysis pubis diastasis and with progressive pain syndrome should be included in the risk group of symphyseal rupture. These patients need not single ultrasound visualization but dynamic pubic ultrasonography (once in 3-4 weeks).
All twelve patients with symphyseal rupture in labor were observed by the obstetrician-gynecologist and orthopedist-traumatologist from one to three years. Women did not complain of pain and pelvic ring displacement either in rest or on exertion, their gait was normal, palpation of the pubic area was painless, any signs of pelvic arthrosis and urine incontinence were not found. Conservative treatment used in all cases of symphyseal ruptures in labor allowed achieving positive results.
Conclusion
The frequency of SPD in pregnancy reaches 0.5% and it increased from 0.1-1.1% for six years.
Cesarean section should be performed for prevention of symphyseal rupture in all cases of pain syndrome even if symphysis pubis diastasis is less than 10 mm (I stage).
The dynamic ultrasonography of pubic symphysis in the third trimester of pregnancy is necessary for management tactics in labor.
Conservative treatment of symphyseal rupture allows restoring pelvic ring integrity with good functional result.
References
- Chernukha E.A. Normal and pathological postpartum period. Moscow: GEOTAR-Media; 2006. 272p. (in Russian)
- Allsop J.R. Symphysis pubis dysfunction. Br. J. Gen. Pract. 1997; 41(4): 115-8.
- Ewies A.A., Olah K.S. The sharp end of medical practice: the use of acupuncture in obstetrics and gynecology. Br. J. Obstet. Gynecol. 2002; 109(1): 1-4.
- Hagen R. Pelvic girdle relaxation from an orthopaedic point of view. Acta Orthop. Scand. 1974; 45(4): 550-63.
- Puhakka K.B., Jurik A.G., Egund N., Schiottz-Christensen B., Stengaard-Pedersen K., van Overeem Hansen G., Christiansen J.V. Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MRT in comparison with radiography and CT. Acta Radiol. 2003; 44(2): 218-29.
- Albert H.B., Godskesen M., Westergaard J.G. Evalution of clinical test used in classification procedures in pregnancy-related pelvic joint pain. Eur. Spine J. 2000; 9(2): 161-6.
- Snijders C., Vleeming A., Stoeckart R. Transfer of lumbosacral load to iliac bones and legs. Part 1: Biomechanics of self-bracing of the sacroiliac joints and its significance for treatment and exercise. Clin. Biomech. (Bristol, Avon). 1993; 8(6): 285-94.
- Rodríguez H.A., Ortega H.H., Ramos J.G., Muñoz-de-Toro M., Luque E.H. Guinea-pig interpubic joint (symphysis pubica) relaxation parturition: underlying cellular processes that resemble an inflammatory response. Reprod. Biol. Endocrinol. 2003; 1: l13.
- Snelling F.G. Relaxation of pelvic symphyses during pregnancy and parturition. Am. J. Obstet. Dis. Women Child. 1870; 2: 561-96.
- Huskisson E.S. Measurement of pain. Lancet. 1974; 2(7889): 1127-31.
- Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., ed. Obstetrics. National guideline. Moscow: GEOTAR-Media; 2015. (in Russian)
Received 19.07.2017
Accepted 22.09.2017
About the Authors
Yavorskaya, Svetlana D., MD, Professor of the Department of Obstetrics and Gynecology with a course of DPO FGBOU HPE ASMU.656038, Russia, Altai Territory, Barnaul, Lenin Avenue, 40. Tel.: +73852368587. E-mail: l2001@bk.ru
Plotnikov, Ivan A., Candidate of Medical Science, Assistant of the Department of Specialized Surgery in Urology, Traumatology and Ophthalmology.
656038, Russia, Altai Territory, Barnaul, Lenin Avenue, 40. Tel.: +73852245604. E-mail: Ivan_Plotnikov85@mail.ru
Bondarenko, Anatoliy V., MD, Professor of the Department of Specialized Surgery in Urology, Traumatology and Ophthalmology, ASMU.
656038, Russia, Altai Territory, Barnaul, Lenin Avenue, 40. Tel.: +73852246833. E-mail: Barnaul-mixa@mail.ru
Olimova, Aziza, post-graduate student of the Department of Obstetrics and Gynecology with a course of DPO of FSBMU HPE of ASMU.
656038, Russia, Altai Territory, Barnaul, Lenin Avenue, 40. Tel.: +73852368587. E-mail: l2001@bk.ru
Plotnikova, Irina V., obstetrician-gynecologist, KGBUK KKBSMP, Barnaul.
656038, Russia, Altai Territory, Barnaul, Lenin Avenue, 40. Tel.: +73852245604. E-mail: Ivan_Plotnikov85@mail.ru
For citations: Yavorskaya S.D., Plotnikov I.A., Bondarenko A.V., Olimova A.O., Plotnikova I.V. Treatment of obstetric ruptures of pubic symphysis and dysfunctions of the pubic articulation. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (9): 68-72. (in Russian)
https://dx.doi.org/10.18565/aig.2018.9.68-72