Гиперпролактинемия – это стойкое избыточное содержание пролактина в сыворотке крови. Синдром гиперпролактинемии – симптомокомплекс, возникающий на фоне гиперпролактинемии, наиболее характерным проявлением которого является нарушение функции репродуктивной системы [1]. Гиперпролактинемия – распространенная эндокринопатия у женщин. Распространенность патологической гиперпролактинемии колеблется от 10 до 30 случаев на 100 тыс. человек, встречается у 5% женщин репродуктивного возраста [2]. Треть женщин на приеме у акушера-гинеколога предъявляют жалобы на различные нарушения менструального цикла, что может быть связано в том числе и с повышением уровня пролактина. Согласно статистике, среди женщин репродуктивного возраста с аменореей гиперпролактинемия встречается у 9%, среди женщин с синдромом поликистозных яичников – у 17%. Репродуктологи в РФ должны оценивать уровень пролактина у женщин с бесплодием с целью уточнения генеза ненаступления беременности [3, 4].
В клиниках репродукции гиперпролактинемия встречается у 5% пациенток, среди пациенток с повторным выкидышем – у 36% [5, 6]. Идиопатическая гиперпролактинемия составляет 40% от общего числа случаев гиперпролактинемии [5].
Гиперпролактинемия может быть клиническим сочетанным проявлением различного числа патологических состояний органов репродуктивной системы у женщин [4, 7]. Например, около 70% нарушений менструального цикла у женщин репродуктивного возраста могут сочетаться с гиперпролактинемией вследствие стресса и дистресса, травм, хирургического лечения гинекологической и негинекологической патологий, приемом пероральной гормональной контрацепции и психотропных препаратов группы нейролептиков и антидепрессантов.
В данной статье мы рассмотрим наиболее частые вопросы, ошибки, трудности наблюдения пациенток с гиперпролактинемией, которые встречаются на гинекологическом приеме.
Пролактин – только лишь гормон для лактации?
Пролактин (ПРЛ):
- один из гормонов гипофиза, секретируется в лактотрофных клетках передней доли;
- по химическому строению – полипептидный гормон, состоящий из 199 аминокислотных остатков с молекулярной массой 23 кДа.
Гипоталамо-гипофизарная система оказывает как тормозящее, так и стимулирующее влияние на секрецию ПРЛ. Гипоталамус оказывает ингибирующее влияние на секрецию ПРЛ, так как дофамин, вырабатывающийся в гипоталамусе и поступающий в гипофиз по портальному кровеносному гипоталамо-гипофизарному тракту, тормозит секрецию ПРЛ путем стимуляции дофаминовых рецепторов, находящихся на лактотрофных клетках. Дофамин и его агонисты, стимулируя D2-рецепторы, ингибируют аденилатциклазу, снижая уровень внутриклеточного цАМФ, что вызывает уменьшение секреции и высвобождения ПРЛ. С другой стороны, ПРЛ способен активировать дофаминергические нейроны, тем самым обеспечивая гипоталамический контроль собственной продукцией (короткая петля механизма обратной связи) [8].
Секреция ПРЛ находится под сложным нейроэндокринным контролем, в ней участвуют различные факторы, в том числе нейромедиаторы, гормоны периферических эндокринных желез.
ПРЛ обладает широким спектром биологического действия в организме человека, является полифункциональным гормоном, участвующим в инициации и поддержании лактации, функционировании желтого тела, продукции прогестерона. Вне зависимости от причины гиперпролактинемии избыточная секреция ПРЛ может приводить к нарушениям пульсаторного выброса лютеинизирующего (ЛГ), фолликулостимулирующего (ФСГ) гормонов и, как следствие, – к гипогонадизму и бесплодию. Со стороны репродуктивной системы у женщин наблюдаются галакторея, нарушения менструального цикла (аменорея, олиго-опсоменорея, ановуляторные циклы, недостаточность лютеиновой фазы), бесплодие, снижение полового влечения.
Помимо гипофиза, ПРЛ вырабатывается и экстрагипофизарно: в эндометрии, миометрии, децидуальной оболочке иммунных клетках, ткани головного мозга, молочной железе, простате, коже и жировой ткани [9].
Почему может повышаться пролактин и о чем не стоит забывать?
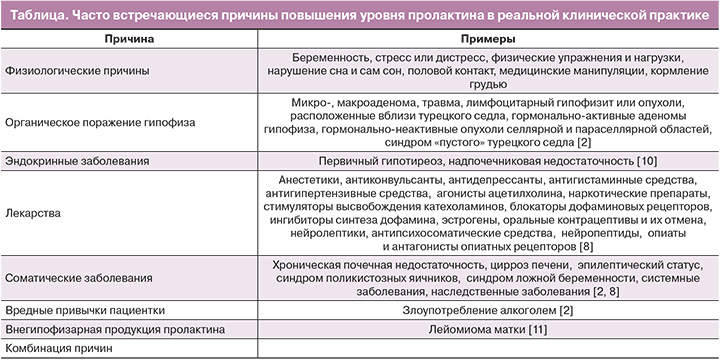
Часто встречающиеся причины гиперпролактинемии представлены в таблице.
Феномен макропролактинемии – лабораторный феномен, заключающийся в преобладании в образце сыворотки крови высокомолекулярной биологически неактивной фракции пролактина [2]. Макропролактин составляет до 25% гиперпролактинемических сывороток. Макропролактинемия является важной причиной неправильного диагноза, ненужных расследований и «неправильного» лечения. По данным Т.Р. Smith et al., среди пациентов с макропролактинемией 93% прошли МРТ гипофиза и 87% получали лечение [2, 12, 13].
Как, когда и при каких условиях пациентка должна сдать анализ на пролактин?
Ошибки в диагностике синдрома гиперпролактинемии, как правило, связаны с лабораторными исследованиями и недостаточно полно собранным анамнезом. Что касается пролактина, то чаще всего приходится сталкиваться с проблемой гипердиагностики, поскольку частота встречаемости гормонально-неактивных аденом гипофиза достаточно высокая и в общей популяции достигает 10%, а по данным аутопсий – 35% [14].
Согласно российскому протоколу по гиперпролактинемии, для постановки диагноза необходимо соблюдать следующие правила:
- забор крови следует проводить в утренние часы, поскольку секреция ПРЛ подчиняется циркадным суточным ритмам (максимальная выработка отмечается во время сна, минимальная – в утреннее время);
- как минимум двукратное проведение лабораторного исследования уровня пролактина;
- у женщин выработка ПРЛ может варьироваться в зависимости от фазы менструального цикла (повышение в пределах нормальных значений фиксируется в периовуляторный период и в лютеиновую фазу), поэтому проведение забора крови рекомендуется в первую фазу менструального цикла (3–7-й день);
- при оценке уровня ПРЛ следует ориентироваться на референсные значения нормы для лаборатории, в которой проводится исследование;
- проведение функциональных проб (с метоклопрамидом, тиролиберином) для дифференциальной диагностики причин гиперпролактинемии в настоящее время не используют [2, 14].
Женщинам репродуктивного возраста с нарушениями менструального цикла и повышением пролактина необходимо исключить беременность.
Пациенткам с гиперпролактинемией рекомендуется оценка функции почек, печени, приема ряда лекарственных средств. При подозрении на развитие фармакологической гиперпролактинемии рекомендуется повторное определение уровня пролактина через 72 ч после отмены препарата, если таковая не несет риск для пациента [2].
Для исключения симптоматических и смешанных форм гиперпролактинемии рекомендуется исследование функции щитовидной железы.
Противоречие между значительными размерами опухоли и умеренным повышением уровня пролактина может быть обусловлено сдавлением гипофизарной ножки объемным образованием селлярной области или несовершенством лабораторной диагностики – «HOOK»-эффектом (лабораторный артефакт в методике определения уровня пролактина и ряда пептидных гормонов, при котором определяемый уровень гормона оказывается ложно заниженным) [2, 15].
Повышение уровня пролактина выше физиологических норм (у женщин – более 550 мEД/л, у мужчин – более 400 мЕД/л) требует дальнейшей дифференциальной диагностики.
Когда направить пациентку на дополнительные методы исследования (МРТ гипофиза)?
Как правило, микроаденомы ассоциированы с уровнем более 5000 мЕД/л, макроаденомы – более 10 000 мЕД/л, при этом уровень пролактина менее 2000 мЕД/л более характерен для гиперпролактинемии неопухолевого генеза [1, 2].
Прибегнуть к дополнительному методу исследования (магнитно-резонансной томографии, МРТ) следует после исключения вторичных причин гиперпролактинемии или при первичном подозрении на имеющуюся опухоль (сопутствующая головная боль, нарушения полей зрения). МРТ головного мозга рекомендуется как наиболее информативный метод в диагностике опухолей гипоталамо-гипофизарной области [2].
Когда, кому и на сколько назначается лекарственная терапия?
При гиперпролактинемии лечение проводится не во всех случаях. При истинной стойкой гиперпролактинемии без клинических проявлений лечения не требуется. Активное лечение необходимо при сочетании гиперпролактинемии с клиническими симптомами (нарушение менструального цикла, галакторея и т.д.) или с наличием микро- и макропролактиномы гипофиза на МРТ. Метод лечения пациентов с гиперпролактинемией определяется характером заболевания. Приоритетным методом лечения пациентов с любой формой гиперпролактинемии является медикаментозный – лечение агонистами дофамина. Такая терапия патогенетически обоснована и имеет много преимуществ перед хирургическими методами лечения и лучевой терапией. Цель лечения синдрома гиперпролактинемии: нормализация уровня пролактина, уменьшение размеров опухоли, устранение симптомов гиперпролактинемического гипогонадизма и восстановление фертильности, предотвращение рецидива или возобновления роста опухоли.
Каберголин рекомендуется в качестве препарата первой линии как наиболее эффективный в отношении нормализации уровня пролактина и уменьшения размеров опухоли [2]. Данные по эффективности были получены в исследованиях, проведенных на оригинальном каберголине – препарате Достинекс. Снижение дозы применяемого препарата или его отмена рекомендуются не ранее чем через 2 года непрерывного лечения при условии длительной нормализации уровня пролактина и значительного уменьшения опухоли или отсутствия таковой по данным МРТ головного мозга.
Терапию препаратами каберголина следует начинать с 1/2 таблетки (0,25 мг) 2 раза в неделю под конт-ролем уровня ПРЛ, корректируя дозу в зависимости от его показателей до достижения стойкой нормопролактинемии. Терапевтическая доза препарата составляет 1–2 мг в неделю, коррекция дозы осуществляется не чаще 1 раза в месяц на 0,5 мг [16]. При первом назначении дофаминергической терапии женщины должны быть предупреждены, что восстановление овуляции и фертильности может произойти немедленно (даже до первой нормальной менструации у них). Также нецелесообразно назначение терапии на 4–6 недель с последующей отменой: как правило, терапия пациенток с гиперпролактинемией (в т.ч. идиопатической) требуется в пролонгированном режиме.
Согласно российским клиническим рекомендациям, основными критериями отмены медикаментозной терапии являются продолжительность лечения более 2 лет, нормализация уровня пролактина, отсутствие аденомы по данным МРТ, значительное уменьшение размеров опухоли (более 50% от исходного размера или уменьшение размера макроаденомы менее 10 мм), беременность, постменопауза, возможность дальнейшего медицинского наблюдения [2]. После отмены агонистов дофамина динамический контроль уровня пролактина проводится 1 раз в 3 месяца в течение 1 года, далее ежегодно в течение как минимум 5 лет.
Результаты наиболее масштабного и длительного исследования исходов беременностей, инициированных каберголином, были опубликованы в 2008 г. Авторы провели анализ 329 беременностей, возникших менее чем через 6 недель после отмены каберголина или на фоне его приема. В 92 случаях проводился анализ длительности влияния каберголина на плод, которая составляла менее 1 месяца приблизительно в 1/3 случаев, 1–2 месяца – в 47%, более 2 месяцев – менее чем в 15%. Среди 329 беременностей, для которых известны исходы, 258 (78%) завершились родами и 71 (22%) – абортами. Из 71 сообщенного аборта 31 (44%) был добровольным, 30 (42%) – самопроизвольными, 9 (13%) – по медицинским показаниям, статус одного аборта неизвестен. Авторы в данном исследовании подчеркивали, что частота спонтанных абортов после применения каберголина при лечении гиперпролактинемии и инициации на фоне терапии беременности не только не превосходила таковую развития данного исхода для популяций США и Европы, но и являлась более низкой – 9,8% по сравнению с 11–15% на американском континенте и 11% для европейской популяции. Не было зарегистрировано повышенного риска рождения детей с низкой и экстремально низкой массой тела [17]. Результаты данного исследования показывают, что лечение каберголином в момент зачатия не повышает риска развития нежелательных явлений со стороны как матери, так и плода. В случае наступления беременности на фоне терапии каберголином прием препарата следует прекратить после подтверждения беременности [18].
В настоящее время мы много говорим о необходимости работать в рамках персонализированной медицины*, а это не только эффективность выбранной схемы терапии, но и в первую очередь безопасность, особенно если это касается женщин репродуктивного возраста, которые потенциально могут стать беременными. В систематическом обзоре и метаанализе 2021 г. были проанализированы эффективность и безопасность дофаминергических агонистов (бромокриптин, каберголин, хинаголид). Семнадцать РКИ были включены в систематический обзор и 17 – в метаанализ. Лекарственные средства имели аналогичную эффективность по снижению пролактина с учетом уровней ПРЛ. Анализ SUCRA показал, что хинаголид более эффективен в коррекции нарушений менструального цикла, тогда как бромокриптин был лучшим для купирования галактореи. Самым безопасным лекарственным препаратом оказался каберголин [19].
Гиперпролактинемия часто заканчивается лечением «анализа», а не болезни
Основные направления диагностического поиска при установлении этиологии гиперпролактинемии определяются исходя из классификации гиперпролактинемического синдрома. Тщательный сбор анамнеза может позволить выявить ятрогенные и симптоматические формы заболевания. Клинические протоколы подчеркивают, что ошибки в диагностике синдрома гиперпролактинемии, как правило, связаны с лабораторными исследованиями.
Комбинированные оральные контрацептивы и гиперпролактинемия
Среди женщин, принимающих оральные контрацептивы с высокими дозами эстрогенов, у 12–30% отмечалось повышение уровня сывороточного пролактина, что, как правило, не требует отмены гормональной контрацепции [20]. Исследования в отношении возможности приема КОК пациентками с микроаденомами гипофиза (пролактиномами) показали, что нет влияния на рост опухоли [20, 21]. Подобные результаты были получены от пациенток с макропролактиномой, которые принимали дофаминергические агонисты и КОК [22]. Стоит отметить, что на данный момент крайне мало исследований с высоким уровнем значимости данных в изучении этого вопроса.
Пролактин, гинекология, будущее
За последние годы появились работы, в которых обсуждается пролактин как прогностический маркер, например, более тяжелых форм эндометриоза, ассоциированного с бесплодием [23, 24]. Р. Mirabi et al. в исследовании показали: более высокие уровни пролактина наблюдались у бесплодных женщин с более тяжелым эндометриозом по сравнению с бесплодными женщинами без эндометриоза. Уровень пролактина может быть в будущем прогностическим биомаркером для выявления III и IV стадий эндометриоза по сравнению с I и II и прогнозирования бесплодия у женщин с эндометриозом [23].
Одновременно выявленное у женщины с нарушениями менструального цикла повышение пролактина и синдрома поликистозных яичников (СПЯ) не редкость. Связь между гиперпролактинемией и СПЯ была описана с 1980-х гг. и предполагала существование патофизиологической связи между этими двумя патологиями; четких данных в литературе пока нет [25].
Авторами исследований выдвигались следующие гипотезы общности этих заболеваний:
- единая гипоталамо-гипофизарная аномалия, которая может объяснить как СПЯ, так и гиперпролактинемию (высокие уровни ЛГ, обнаруженные у женщин с СПЯ, будут вторичными по отношению к снижению дофаминергического тонуса, что также будет отвечать за повышение пролактина) [26, 27];
- СПЯ вызывает гиперпролактинемию за счет относительной гиперэстрогении (различные экспериментальные исследования показали увеличение секреции пролактина под действием эстрогена) [28–31];
- ускорение пульсации гонадолиберина у женщин с СПЯ (что способствует повышению уровня ЛГ и снижению дофаминергического тонуса (что вызывает гиперпролактинемию) [31].
Hayashida и другие авторы в исследованиях показали, что часто у женщин с СПЯ выявляется макропролактинемия [32], не требующая проведения визуализационных методов диагностики и назначения лечения агонистами допаминовых D2-рецепторов.
Диагностика синдрома гиперпролактинемии у женщин с СПЯ и повышением уровня пролактина должна быть проведена согласно клиническому протоколу ведения гиперпролактинемии.
Появились работы, которые показали высокие уровни сывороточного пролактина и высокую экспрессию рецептора пролактина (PRLR) в раковых клетках у женщин с раком эндометрия и раком яичника [9, 33]. Рак эндометрия патогенетически подразделяется на 2 типа: тип I связан со стойкими гиперэстрогенией и прогестероновой недостаточностью, а также к факторам риска возникновения I типа относят ановуляцию и бесплодие [34]. Гиперпролактинемия может приводить к бесплодию вследствие ановуляции. Авторы исследований предполагают, что пролактин связан с I типом рака тела матки.
Исследователи анализируют негативное влияние гиперпролактинемии на костный метаболизм. Экспериментальные данные показали, что при высоком уровне ПРЛ резорбция кости увеличивалась, а костеообразование подавлялось. Повышенный уровень ПРЛ вызывает снижение уровня половых гормонов, что, в свою очередь, может оказывать негативное воздействие на костную ткань. У пациентов с гиперпролактинемией часто наблюдаются снижение минеральной плотности костной ткани, а также повышенный риск переломов [35]. Рецептор пролактина экспрессируется остеобластами. С одной стороны, ПРЛ может косвенно контролировать активность остеокластов за счет дозозависимой активации в остеобластах нескольких цитокинов (RANKL, TNF-a, IL-1 и циклооксигеназа-2). С другой стороны, ПРЛ может подавлять дифференцировку клеток – предшественников зрелых остеобластов, а также снижать их секреторную функцию [36–40].
Заключение
Практика гинеколога неотрывно связана с эндокринологией, поэтому и патологию щитовидной железы, и нарушения углеводного обмена, и синдром гиперпролактинемии часто первично диагностирует именно гинеколог. Гиперпролактинемия часто выявляется на приеме акушером-гинекологом у женщин репродуктивного возраста с жалобами на нарушения менструального цикла. Неоднократно было показано, что избыточная секреция ПРЛ, которому ранее отводилась скромная роль в регуляции лактации, довольно часто служит причиной нарушений менструальной и репродуктивной функций. На долю гиперпролактинемии приходится до 25–40% всех случаев женского бесплодия. Гиперпролактинемия также встречается в 10% случаев у женщин с аменореей, в 20–30% – с галактореей. В последние годы дискутируется вопрос о генезе гиперпролактинемии у пациенток с СПЯ. Особенности диагностики и лечения гиперпролактинемии и ведение пациентки могут осуществляться гинекологом, а в половине случаев, как правило, совместно с эндокринологом с учетом индивидуального подхода к каждой женщине. Необходимо следовать всем обязательным рекомендациям международных и федеральных клинических рекомендаций, что позволит практическому врачу повысить эффективность оказания медицинской помощи.