Бактериальный вагиноз (БВ) – распространенное, часто рецидивирующее заболевание, при котором микробное сообщество влагалища с преобладанием лактобацилл заменяется смесью грамположительных и грамотрицательных бактерий. На долю БВ приходится около 30% выделений из влагалища у женщин различных возрастных групп. Но более всего подвержены БВ женщины репродуктивного возраста, с частотой от 10 до 30% [1–4]. Данное патологическое состояние вызвано дисбалансом вагинальной микроэкологии, наличием Gardnerella vaginalis, Atopobium vaginae и других анаэробных бактерий. В числе многочисленных этиологических факторов БВ лидируют промискуитет, использование барьерных методов контрацепции, в частности презервативов, курение и что очень важно – низкий уровень эстрогенов [5, 6]. Симптомы БВ включают обильные выделения из влагалища, запах рыбной лейкореи, раздражение и жжение в области наружных половых органов [1]. Некоторые исследователи связывают БВ с преждевременными родами [7], воспалением органов малого таза, повышенным риском заражения инфекциями, передающимися половым путем (ИППП), включая синдром приобретенного иммунного дефицита (ВИЧ). Поскольку БВ вызывает дискомфорт в области вульвы и часто рецидивирует, это отрицательно сказывается на качестве жизни и психическом здоровье женщин [8]. Около половины пациентов с БВ имеют клинические симптомы, которые в первую очередь связаны с повышением рН влагалища и могут быть определены с помощью критериев Амселя или шкалы Ньюджента. Критерии Амселя – это простой и практичный подход, который используется в качестве золотого стандарта в клинической практике [9]. Система категорий Ньюджента предусматривает мониторинг вагинальных мазков, окрашенных по Граму. Шкала Ньюджента позволяет проводить более объективную оценку вагинальной флоры, меньше зависит от врача и показывает более высокую чувствительность, чем критерии Амселя [10, 11, 12]. Микробиота влагалища пациенток с БВ изменяется по мере того, как лактобациллы исчезают или резко уменьшаются, а начинают доминировать более разнообразные популяции факультативных и облигатных анаэробных бактерий.
Согласно актуальным российским клиническим рекомендациям и зарубежным гайдлайнам, терапией первой линии БВ является пероральный метронидазол 500 мг 2 раза в день в течение 7 дней; интравагинально гель метронидазола 5,0 г 2 раза в сутки 5 дней или крем клиндамицина 2% 5,0 г 1 раз в сутки в течение 7 дней (уровень убедительности рекомендаций C, уровень достоверности доказательств 5) [13, 14]. Важно отметить, что данное лечение не только высокоэффективно, но и быстро восстанавливает нормальную микрофлору влагалища. Однако эти современные методики не доказали свою достаточную эффективность в долгосрочной перспективе. Так, через 12 месяцев после лечения отмечается до 69% рецидивов [11]. На сегодняшний день доминирует гипотеза, что это связано с образованием биопленок [1, 14, 15]. Высокий процент рецидивов БВ диктует необходимость изучения эффективности, безопасности, продолжительности традиционных методов лечения, а также возможности применения альтернативных подходов как в виде самостоятельных, так и в сочетании с устоявшейся противомикробной терапией.
Несмотря на то что описано достаточно много рандомизированных контролируемых исследований, посвященных изучению различных схем лечения БВ, остается много белых пятен в этом вопросе. Не освещены в полной мере возможности терапии и снижения частоты рецидивов БВ локальными пребиотиками и молочной кислотой в сочетании с антимикробными препаратами. В связи с чем возникает необходимость расширения знаний в данном кластере с обеспечением их соответствия международным стандартам лечения.
Сказанное обусловливает проблему и цель данного исследования. Основная цель: провести сравнительную оценку эффективности молочной кислоты и пребиотика BIOECOLIA в виде вагинального геля «Флоражель» в сочетании с антимикробным средством метронидазол-гель 5,0 г в лечении и предупреждении рецидива БВ.
Материалы и методы
В соответствии с поставленной целью за период с 2023 по 2025 гг. было проведено исследование с участием 81 женщины, проживающей в Российской Федерации. После сбора анамнеза и обследования пациентки от 18 до 45 лет (37,3±7,5 года) с диагнозом БВ, установленным впервые, подтвержденным клинико-диагностическими обследованиями, были разделены на 2 группы в зависимости от терапии. Базовыми клиническими подразделениями явились ООО «Современные диагностические технологии», ООО «ЕкатеринодарЪ» (Краснодар). Все женщины проинформированы (как устно, так и письменно) о выборке, процедуре, рисках и преимуществах анализа, дали письменное информированное согласие и его подписали. Исследование одобрено корпоративным медицинским этическим советом (номер 033; дата 01.02.2023). Наблюдение проводилось динамично, с явками больных на контрольные осмотры и диагностику: перед включением в исследование; через 3 недели после прекращения лечения и через 3 месяца по окончании курации для исключения рецидива болезни. Патогенетическое лечение БВ реализовывалось на основании действующих клинических протоколов: стандартная топическая доза метронидазол-геля 5,0 г 2 раза в сутки 5 дней [3]. В группе I (n=37) применяли гель с метронидазолом 5,0 г 2 раза в сутки в сочетании с вагинальным гелем «Флоражель» 2 раза в день, тогда как в группе II (n=44) проводили терапию только локально гелем с метронидазолом 5,0 г 2 раза в сутки также 5 дней. Разделение на группы было слепым, так как все пациентки были сопоставимы по гинекологическому и соматическому анамнезу. Во время изучения проблемы БВ возникла необходимость в отборе пациенток из обеих групп после окончания курации через 3 недели, у которых не было достигнуто клинического и лабораторного излечения на первом этапе. Из данных пациенток была сформирована группа III (n=21). В этой группе терапия БВ была усилена гелем «Флоражель» до 3 раз в сутки с добавлением антисептического средства на основе деквалиния хлорида (Септофемин) по 1 вагинальной таблетке 1 раз в сутки 6 дней. Повторного использования местного геля с метронидазолом в данной группе пациентов не было.
Гель «Флоражель» – продукт фармацевтической фирмы «Алкой», Россия, в состав которого входят: Aqua, Propylen Glycol, Hydroxyethylcellulose (Natrosol 250 HR), Aloe Barbadensis Juice, Phenoxyethanol, Caprylyl Glycol (Optiphen 200), Panthenol, Chamomilla Recutita (Matricaria) Extract, Lactic Acid, Alpha-Glucan Oligosaccharide (BIOECOLIA). Среди растительных и биологически активных компонентов, входящих в состав геля, основную долю занимают натуральный пребиотик BIOECOLIA и молочная кислота, которые защищают микробиоту влагалища и поддерживают уровень лактобактерий. При этом молочная кислота является также и натуральным увлажняющим компонентом.
Септофемин (деквалиния хлорид, группа компаний «Алкой», Россия) – антисептическое средство с антибактериальным эффектом в отношении грамположительных и грамотрицательных микроорганизмов, обладающее противовирусным, противогрибковым, противовоспалительным, гемостатическим действиями [16].
Микроскопические, рН-метрические и молекулярно-биологические исследования для оценки микробиоценоза
Материалом для исследования служило отделяемое влагалища, которое получали с помощью тампона из полиэстера и универсального зонда. Содержимое одного тампона наносили на предметное стекло для микроскопического исследования.
Согласно критериям Амселя, должны были быть определены минимум 3 симптома БВ: серовато-белые выделения из влагалища, положительные результаты аминного теста, рН влагалища >4,5 и наличие «ключевых клеток» (>20%) во влажном мазке. Для определения рН вагинального содержимого материал наносился на индикаторную бумагу с эталонной шкалой. Для проведения аминного теста на выделения наносились несколько капель 10% КОН (гидроксид калия). Анализ интерпретировался положительным с появлением «рыбного» запаха.
Также для трактования БВ использовалась шкала Ньюджента, основанная на балльной системе после определения соотношения 3 основных морфотипов бактерий: Lactobacillus (крупные грамположительные бактерии), Gardnerella vaginalis, Atopobium vaginae и других небольших грамотрицательных и грамвариабельных бактерий. Ответ выдавался в виде баллов от 0 до 10: 0–3 балла – нормальный состав микрофлоры, преобладают лактобактерии (доминирует морфотип Lactobacillus spp.); 4–6 баллов – промежуточное состояние, возможны начальные изменения состава микрофлоры; 7–10 баллов – БВ, количество лактобактерий снижено, преобладают гарднереллы и/или другие микроорганизмы (доминируют морфотипы Gardnerella vaginalis, Atopobium vaginae и др.).
Для уточнения диагноза БВ и изучения видового состава микрофлоры проводилась полимеразная цепная реакция с детекцией в режиме реального времени (ПЦР-РВ). Молекулярно-генетическое исследование реализовывалось при помощи набора «АмплиПрайм ФЛОРОСКРИН – Бактериальный вагиноз» (ООО «НекстБио», Россия). Комплект реагентов «ПЦР-комплект» FRT-100 для амплификации фрагментов ДНК Gardnerella vaginalis, Atopobium vaginae, Lactobacillus spp. и Bacteria (общее количество бактерий) c гибридизационно-флуоресцентной детекцией позволяет проводить ПЦР в количественном формате. Транспортная среда – «Транспортная среда с муколитиком «АмплиПрайм ТСМ» (РУ № ФСР 2012/14205). Рабочая часть зонда опускалась в вагинальное отделяемое задненижнего свода, вращательными движениями проводился забор содержимого с поверхности эпителия с последующим переносом зонда с содержимым влагалища в транспортную среду.
Критерии включения: участники должны были иметь БВ, подтвержденный клинико-диагностическими критериями.
Критерии исключения: наличие истинных патогенов (Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Мycoplasma genitalium); беременность, кормление грудью; период менопаузы; кровотечение из половых путей неизвестной этиологии; злокачественные новообразования репродуктивной системы; соматические заболевания (заболевание щитовидной железы, сахарный диабет), психиатрические заболевания; прием перорального антимикробного препарата и пробиотика; аллергия на исследуемые препараты; участие в другом исследовании.
Статистический анализ
Статистическую обработку проводили с использованием компьютерных приложений MS Excel, Statistica 6.0 и медико-биологической программы BioStat Professional Prо (6.7.0.3).
Результаты
На первом этапе оценивали состояние микробиоценоза через 3 недели после окончания терапии. Пациентки сообщали о своих субъективных ощущениях, в результате чего оценка симптомов варьировалась от 0 до 7 и более согласно шкале Ньюджента. Результаты представлены в таблице 1.
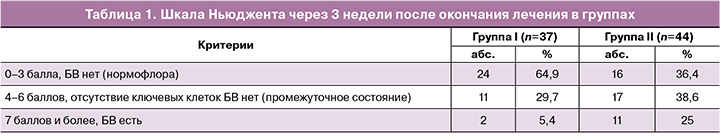
Из представленных данных следует, что концентрация компонентов влагалищного биотопа, соответствующего нормальной микрофлоре (0–3 балла), статистически значимо выше у пациенток группы I, получавших сочетанную топическую терапию метронидазолом 5,0 г и интравагинальным гелем «Флоражель» в отличие от группы II. При этом оценка промежуточного состояния микрофлоры (4–6 баллов) различий в показателях не обнаружила, в то время как сравнение признаков БВ (7 баллов и более) показывало более частую встречаемость недолеченного БВ в группе II в сравнении с группой I
Анализ критериев Амселя выявил феноменальную особенность клинического течения БВ в группах (табл. 2).
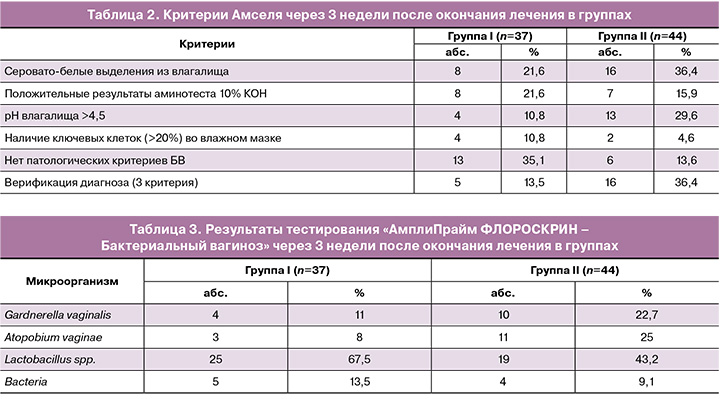
Сравнение относительных показателей по параметру «нет патологических критериев БВ» обнаружило улучшение клинических проявлений в группе I. При этом сравнение данных по группам I и II не фиксировало значимых различий по показателю «положительный аминотест 10% КOH», тогда как по параметру «рН влагалища >4,5» значимо снизилось количество женщин в группе I с высоким рН. Снижение количества «ключевых клеток» в мазках наблюдалось в равных долях в обеих группах, что не повлекло за собой клинически значимых различий между ними. Важно отметить, что после первого этапа лечения в группе II оказалось больше пациенток с диагнозом «недолеченный БВ», выставляемым на основании трех критериев («верификация диагноза (3 критерия»)): 16/44 (36,4%) против 5/37 (13,5%) в группе I. Отмеченное явление свидетельствовало о более благоприятном течении и исходе заболевания в группе I. Однако имело место некоторое несоответствие диагностических критериев БВ согласно шкале Ньюджента и категорий Амселя. В частности, дифференцированный анализ с применением шкалы Ньюджента позволил отметить, что в группе I только у 2/37 (5,4%) пациенток диагностировался неизлеченный БВ, тогда как по системе Амселя этот показатель достигал 5/37 (13,5%). Аналогичная диспропорция отслеживалась и в группе II: верификация БВ обнаружена у 11/44 (25%) женщин по Ньюдженту и у 16/44 (36,4%) по Амселю. Обнаруженная диспропорция требует дальнейших углубленных исследований на большей выборке больных.
Для более интенсивного изучения и понимания исходов лечения нами проводилась ПЦР-РВ (табл. 3).
Как видно из данных, приведенных в таблице 3, разнообразная видовая микрофлора влагалищного биотопа характерна для представительниц обеих групп. Отмечено также, что и автохтонная флора в виде Lactobacillus spp. присутствует в высоком процентном соотношении в обеих группах. Однако это не исключило наличия значимых различий между представительницами групп I и II, что указывало на преобладание положительного эффекта от сочетанного применения вагинального геля с метронидазолом и геля «Флоражель» против монотерапии локальным метронидазол-гелем 5,0 г 2 раза в сутки.
В обеих группах диагностировалось наличие полимикробной ассоциации Gardnerella vaginalis, Atopobium vaginae и Bacteria, но с разной частотой присутствия.
Результаты ПЦР-РВ позволили уточнить частоту распространенности недолеченного БВ после первой линии терапии и выделить пациенток в группу III для назначения второго этапа лечения. Наибольшее число женщин с оставшимися явлениями БВ, согласно критериям Амселя, диагностировалось в группе II – 16, тогда как в группе I эти явления отмечены только у 5 пациенток. Заметим, что по шкале Ньюджента число пациенток с БВ было меньше: группа I – 2 человека; группа II – 11 человек. В продолжении исследования мы основывались на данных критериев Амселя.
У всех пациенток по результатам ПЦР-РВ имело место наличие Gardnerella vaginalis, либо Atopobium vaginae, либо их ассоциации. Таким образом, в группу III вошло 21/81 (26%) женщин. Всем пациенткам на втором этапе лечения произведена смена антибактериального геля с метронидазолом 5,0 г на антисептическое средство «Септофемин» (деквалиния хлорид) по 1 свече 1 раз в сутки интравагинально 6 дней, согласно инструкции к препарату. При этом лечение усилено применением геля «Флоражель» интравагинально до 3 раз в сутки.
При рассмотрении критериев Ньюджента через 3 недели после окончания второй линии терапии в группе III отмечено, что у большинства пациенток после применения антисептического средства «Септофемин» и вагинального геля на основе молочной кислоты и пребиотика явления БВ нивелированы. В частности, «0–3 балла, БВ нет» имели 17/21 (81%) женщин, «4–6 балла, промежуточное состояние, БВ нет» – 2/21 (9,5%) и только у 2/21 (9,5%) имелись признаки БВ. У этих пациенток в анализе ПЦР-РВ после первого этапа лечения была установлена комбинация микроорганизмов Gardnerella vaginalis, Atopobium vaginae и Bacteria, что, по всей вероятности, и отразилось в устойчивости к лечению БВ.
БВ у 2/21 (9,5%) больных также подтверждался критериями Амселя (сочетание трех независимых параметров). Результаты по шкале Ньюджента и критериям Амселя согласовывались между собой. В соответствии с критериями Амселя обильные влагалищные выделения встречались только у 1/21 (4,8%) пациентки, так же как лишь в единичном случае диагностировался положительный аминный тест (4,8%); рН влагалища >4,5 на основании окраски тест-полоски имел место у 2/21 (9,5%) пациенток. В противоположность описанным выше патологическим симптомам отсутствие какого-либо симптомокомплекса, характерного для БВ, отмечено у 17/21 (80,9%) женщин, что свидетельствовало о достаточно продуктивном результате второй линии терапии Септофемином и Флоражелем.
Согласно задачам исследования, важно было оценить наличие рецидива БВ через 3 месяца после проведенного лечения. Для более объективной оценки возможного рецидивного процесса на третьем этапе обследования выбыли 2 устойчивые к лечению БВ пациентки, которым рекомендовалось применение системной терапии.
Через 3 месяца после лечения отмечены преобладание нормофлоры (0–3 балла), а также меньшая доля больных с промежуточным состоянием (4–6 балла) в группе I в сравнении с группой II. Наличие рецидива БВ в группах не отличалось и верифицировалось в единичных случаях (табл. 4).

Полученные результаты терапии через 3 месяца на основании критериев Амселя представлены в таблице 5.
Важно отметить, что по всем критериям различий в группах не обнаружено. Частота излеченного БВ и как следствие отсутствие рецидива в группах не отличались. В то же время в обеих группах диагностировались изменения в виде повышенного количества выделений, положительного аминного теста, рН выше 4,5, однако это были единичные случаи (табл. 5).
Для полноценной оценки исходов лечения и исключения рецидива БВ проведена ПЦР-РВ (табл. 6).
Результаты ПЦР-РВ показали, что в группе I по сравнению с группой II значимо преобладало число пациенток с излеченным БВ. В группе II имелись больные с различными патогенными бактериями в микрофлоре влагалища, в том числе с Gardnerella vaginalis и Atopobium vaginae, но ввиду малой численной представленности проведение статистического анализа было ограничено. Однако данные ПЦР-РВ подтверждали наличие БВ, что согласовывалось с результатами критериев Ньюджента и Амселя.
Обсуждение
Проблема БВ, несмотря на имеющиеся на сегодняшний день сведения и знания, оставляет множество вопросов, касающихся его лечения, поскольку все современные методы терапии имеют определенные недостатки и ограничения [17, 18]. Идет активный поиск альтернативных подходов воздействия на БВ. Один из методов предполагает использование вагинального геля с молочной кислотой для снижения pH влагалища, что способствует повторной колонизации лактобацилл [10]. Низкий pH влагалища способствует лизису отшелушенных эпителиальных клеток и высвобождению гликогена в просвет влагалища для его метаболизации лактобациллами [8]. Проведенное нами исследование во многом согласуется с существующими данными, демонстрируя еще не до конца утвердительные, но многообещающие результаты относительно эффективности вагинального геля с молочной кислотой и пребиотиком BIOECOLIA (Флоражель) в лечении БВ. Результаты также демонстрируют высокую комплаентность антисептического препарата «Септофемин» на основе деквалиния хлорида в терапии БВ.
В соответствии с методическими рекомендациями Центров по контролю и профилактике заболеваний США лечение БВ показано только женщинам с симптомным течением БВ [19, 20]. Согласно клиническим протоколам Российской Федерации, лечение БВ проводится на основании «снижения количества “ключевых” клеток при микроскопическом исследовании влагалищного отделяемого при контрольном обследовании и достижения клинического выздоровления» [13]. В проведенном исследовании мы руководствовались клиническими и диагностическими показателями БВ.
На первом этапе, через 3 недели после окончания лечения, оценка успешности терапии БВ в группах предусматривала анализ субъективных и объективных показателей, в частности критериев Амселя, шкалы Ньюджента, а также результаты ПЦР-РВ. Отмечено увеличение частоты нормофлоры в 1,5 раза в группе I, женщины которой получали сочетанную топическую терапию: метронидазол 5,0 г 2 раза в сутки, а также гель с молочной кислотой и пребиотиком BIOECOLIA (Флоражель). Доказательством эффективности комбинированного лечения в группе I было и снижение в 5,5 раза остаточных проявлений БВ (7 баллов и выше) по шкале Ньюджента. Аналогичная картина представлялась и на основании критериев Амселя. В то же время нельзя не отметить, что обнаружен определенный диссонанс между категориями Ньюджента и критериями Амселя. В частности, в соответствии с показателями Амселя имелось численное превышение больных с остаточными явлениями БВ в обеих группах, нежели по шкале Ньюджента. Данная несогласованность результатов, по нашему мнению, может быть в определенной степени обусловлена субъективным характером отдельных критериев Амселя. Однако данный факт требует более углубленного изучения. При этом нельзя не отметить, что с применением обеих методов недолеченный БВ после первого этапа лечения диагностирован чаще в группе II (топическая монотерапия метронидазолом 5,0 г 2 раза в день).
Для объективизации анализа в исследовании проводилась ПЦР-РВ, которая четко определила превалирование резидентной флоры в виде Lactobacillus spp. в группе I (67,5%) против группы II (43,2%). Нельзя оставить без внимания и разность содержания Atopobium vaginae между группами. Так, содержание данного микроорганизма в группе II было в 5,5 раза выше, чем в группе I. Заметим, что Atopobium vaginae, как и Gardnerella vaginalis, может диагностироваться и у женщин с нормальной экологией влагалища (от 8 до 25%), однако гораздо чаще этот микроорганизм встречается у больных БВ (от 50 до 96%) [18, 21–24]. В нашем исследовании на основании ПЦР-РВ Gardnerella vaginalis обнаруживалась примерно в одинаковом количестве в обеих группах, статистически значимо не различаясь, что объяснялось высокой чувствительностью кокков к метронидазолу, как в моно-, так и в комбинированной терапии БВ. Надо отметить, что еще в 2011 г. O’Hanlon D.E. et al. представили данные, подтверждающие эффективность использования молочной кислоты in vitro для инактивации бактерий, ассоциированных с БВ, без воздействия на вагинальные лактобациллы [25]. Важно подчеркнуть, что сведения о применении молочной кислоты в лечении БВ носят контраверсионный характер. Так, в систематическом обзоре Plummer E.L. et al. (2021) сравнили текущие исследования, изучающие использование вагинальной молочной кислоты in vivo, и получили неоднозначные результаты: продукт вагинальной молочной кислоты действовал так же или значительно хуже метронидазола [26]. Оппоненты данного обзора Tidbury F. et al. (2025) провели пилотное исследование, сравнивающее эффективность вагинального геля с молочной кислотой со стандартным пероральным метронидазолом в терапии БВ. Результаты превысили оптимистичные ожидания: вагинальный гель с молочной кислотой действовал так же, как пероральный метронидазол, и был успешным в уменьшении выделений на 69%, неприятного запаха из влагалища на 50% и зуда на 84% в течение первых трех недель. Однако по сравнению со стандартным лечением пероральным метронидазолом краткосрочные показатели излечения были значительно ниже. Все это, по словам исследователей, требовало более углубленного анализа. Однако авторами отмечена сильная сторона их исследования, включающая фокусировку внимания на варианте лечения без антибиотиков, что весьма актуально в контексте растущей к ним резистентности [10]. Также необходимо отметить, еще в 2006 г. Decena D.C. et al. сообщали, что сочетание метронидазола и вагинального геля с молочной кислотой давало лучшие результаты в профилактике как объективных, так и субъективных рецидивов БВ [27].
Результаты нашего исследования продемонстрировали эффективность применения геля с молочной кислотой и пребиотика BIOECOLIA (Флоражель) в терапии БВ, что определенным образом может выступить продолжением к имеющимся работам, посвященным возможностям альтернативных методов терапии БВ.
Оценка исходов БВ показала и частоту неизлеченного БВ после первой линии терапии. Пациентки из обеих групп (5 из группы I и 16 из группы II) вошли в группу III. Данным женщинам были предложены вторая линия терапии БВ антисептическим средством «Септофемин» и увеличенная кратность приема геля «Флоражель» до 3 раз в сутки. Усиленная формула лечения повлекла нивелирование проявлений БВ как клинически, так и диагностически. Только у 2/21 пациенток (9,5%) сохранялись признаки болезни, которые подтверждались наличием поливалентной микрофлоры (Gardnerella vaginalis, Atopobium vaginae и Bacteria). По нашему мнению, именно такое сочетание бактериальных агентов давало стойкий резистентный характер течения БВ. Это обстоятельство потребовало назначения системной терапии и исключения данных пациенток из дальнейшего исследования. Несмотря на сохранение БВ у двух женщин, отмечаем достаточно успешное воздействие антисептического средства «Септофемин» на основе деквалиния хлорида и увеличение дозы геля «Флоражель» во время проведения второй линии терапии БВ. Доступные на сегодняшний день научные данные подтверждают, что деквалиния хлорид является одним из эффективных средств лечения БВ, поскольку обладает широким спектром антимикробной активности в отношении соответствующих патогенных микроорганизмов, особенно в отношении Gardnerella vaginalis, Atopobium vaginae и имеет приемлемый профиль безопасности [17]. В работе Ших Е.В. и соавт. (2024) подчеркивается, что препарат «Септофемин» – первый отечественный дженерик на фармацевтическом рынке РФ. Экономическая доступность лекарственного средства открывает перспективу расширения его медицинского применения. Высокая эффективность и безопасность препарата позволят сократить применение антибиотиков в фармакотерапии вульвовагинальных инфекций [28].
Важно было сравнить частоту рецидива БВ на фоне топической монотерапии метронидазолом 5,0 г и комбинированной терапии вагинальным гелем с метронидазолом 5,0 г в сочетании с гелем «Флоражель». Во-первых, было отмечено отсутствие выраженных изменений в микробиоте влагалища у всех пациенток. Наличие рецидива БВ в группах значимо не отличалось и верифицировалось в единичных случаях: в группе I – 2,7%, в группе II – 7,2%. ПЦР-РВ также подтверждала наличие единичных случаев БВ, что согласовывалось с результатами критериев Ньюджента и Амселя. Случайные патологические проявления в виде повышенного количества выделений, положительного аминного теста, рН выше 4,5 не представляли триаду БВ и соответственно не повлекли за собой клинических изменений самочувствия больных. При этом данные проявления не имели статистически значимых различий между группами. Однако необходимо сказать, что нормальный микробиоценоз влагалища чаще диагностировался в группе I по сравнению с группой II (86,6% против 59,5%). Весомым обстоятельством, на наш взгляд, было наличие в группе I большего числа женщин с достаточным количеством Lactobacillus spp. в отличие от группы II, что свидетельствовало о выраженном положительном эффекте сочетанного лечения метронидазол-гелем 5,0 г и вагинальным гелем «Флоражель».
В ранее проведенных исследованиях [10] показана возможность монотерапии БВ гелями на основе молочной кислоты, но такая терапия имела высокий процент рецидивов – 37,5%, что более чем вдвое превышало показатели группы, принимавшей системно метронидазол (14,3%). По мнению исследователей, безусловно, требуются дальнейшие углубленные разработки данной проблемы.
Завершая обсуждение результатов применения геля на основе молочной кислоты, пребиотика BIOECOLIA, сока алоэ вера, пантенола, а также экстракта ромашки (Флоражель) для лечения БВ нельзя не отметить, что основной точкой приложения данного средства является терапия менопаузального генитоуринарного синдрома. И в данном аспекте все растительные и лекарственные компоненты, входящие в состав Флоражеля, уже показали свою высокую эффективность [29]. В нашем исследовании мы обнаружили дополнительные возможности геля «Флоражель» в комбинированном лечении БВ, а также его эффективность в снижении частоты рецидивов заболевания. Полученные результаты расширяют окно возможностей альтернативной медицины, улучшающих исходы терапии, и позволяют внедрять в практику безопасные, но достаточно качественные методы лечения БВ.
Выводы
Проведенное исследование позволило нам сделать следующие выводы.
1. Вагинальный гель с молочной кислотой является безопасной и, как правило, хорошо переносимой альтернативой, которая легкодоступна без рецепта.
2. Комбинированное применение топического геля с метронидазолом в стандартной дозировке, усиленное гелем с молочной кислотой и пребиотиком BIOECOLIA (Флоражель), демонстрирует положительные результаты, превосходящие монотерапию топическим гелем с метронидазолом 5,0 г.
3. В качестве второй линии терапии БВ с высокой безопасностью и эффективностью может быть рекомендовано сочетанное применение антисептического средства на основе деквалиния хлорида (Септофемин) в комбинации с гелем «Флоражель», но с увеличением кратности приема геля до 3 раз в сутки.
По нашему мнению, несмотря на показатели хорошей эффективности вагинального геля с молочной кислотой и пребиотиком BIOECOLIA следует изучить проблему в более масштабном исследовании, на репрезентативной выборке когорты больных.