Efficacy of the tourniquet hemostasis combined with vaginal balloon tamponade using a Zhukovsky vaginal catheter during delivery in placenta accreta spectrum
Objective: To evaluate the efficacy of distal tourniquet hemostasis combined with vaginal balloon tamponade using a Zhukovsky vaginal catheter during delivery of pregnant women with placenta accreta spectrum to reduce intraoperative blood loss.Kulikov I.A., Shmakov R.G., Belousova T.N., Plakhotina E.N., Nizyaeva N.V., Geilis I.A., Iskakov D.D., Milyutina E.R., Vdovichenko E.A., Prochakovsky D.V.
Materials and methods: A prospective observational study enrolled 164 pregnant women with histologically confirmed placenta accreta spectrum and underwent distal tourniquet hemostasis. The patients were divided into Group 1 (study group, n=133) and Group 2 (control group, n=31) who had and did not have vaginal balloon tamponade in addition to distal tourniquet hemostasis, respectively.
Results: All patients in Group 1 (n=133) underwent organ-sparing surgery. The median blood loss was 959 (699; 1651) mL in Group 1 and 1549 (899.5; 2098) mL in Group 2. Patients in Group 1 did not require a transfusion of donor blood components. The volume of autotransfusion in the study group was 208 ml versus 485 ml in the control group.
Conclusions: Distal tourniquet hemostasis combined with vaginal balloon tamponade using a Zhukovsky vaginal catheter was highly effective in surgical delivery in patients with placenta accreta spectrum and allowed significant reduction in intraoperative blood loss. The findings of the study give reason to recommend the use of this technique in daily clinical practice to guide the delivery strategy in pregnant women with this pathology.
Keywords
Obstetric hemorrhage continues to be the leading cause of maternal mortality, ranging from 19.9% to 36.2%, and is responsible for 127 000 deaths of women of reproductive age annually [1, 2]. A significant proportion of massive obstetric hemorrhage is associated with the placenta accreta spectrum. Year by year, the number of these patients is increasing, which is directly associated with increased rates of abdominal delivery. Over the past 50 years, their number has increased 10 times [3].
The accumulated evidence suggests an increase in the risk of the placenta accreta spectrum with each subsequent cesarean section (CS), which in turn, increases the risk of maternal morbidity and mortality [4]. To date, there is a proven relationship between the increasing number of C-sections and the frequency of abnormal placentation. Moreover, the risk of placenta accreta spectrum in the uterine scar increased by 7 times after one previous CS and by 56 times after three or more operations [5].
Currently, there is no unified approach to the treatment of patients with placenta accreta spectrum; surgical techniques vary from country to country [6]. Surgical strategies include non–organ-sparing (primary or delayed hysterectomy) and organ- sparing approaches.
In most countries, traditional surgical treatment of the antenatally diagnosed placenta accreta spectrum is planned early operative delivery and single-step hysterectomy [7–9]. CS with a fundal uterine incision, fetal extraction, and hysterectomy without an attempt to remove the placenta significantly reduces blood loss [10]. This strategy is considered the standard of care, recommended by most specialized centers in the United States and the American College of Obstetricians and Gynecologists (ACOG); only 14.9–32.0% of specialists choose conservative methods (leaving the placenta in situ) [11, 12]. According to an international 2018 survey, about 60% of specialists prefer radical surgery for the placenta accreta spectrum [13].
The current study aimed to evaluate the efficacy of distal tourniquet hemostasis combined with vaginal balloon tamponade using a Zhukovsky vaginal catheter during delivery of pregnant women with placenta accreta spectrum to reduce intraoperative blood loss.
Materials and methods
A prospective observational study included 164 pregnant women with histologically confirmed placenta accreta spectrum who underwent surgery with distal tourniquet hemostasis at the Vidnovsky Perinatal Center from 2017 to 2022. The patients were divided into Group 1 (study group, n=133) and Group 2 (control group, n=31) who had and did not have vaginal balloon tamponade in addition to distal tourniquet hemostasis, respectively.
Inclusion criteria were age 18–45 years, singleton pregnancy, placenta accreta spectrum, uterine scar after previous CS, and abnormal placental implantation.
Exclusion criteria were multiple pregnancies, severe maternal somatic comorbidities, delivery before 26 weeks of gestation, and fetal malformations incompatible with life.
Placenta accreta spectrum is diagnosed by antenatal ultrasound examination. Typical ultrasound characteristics of the placenta accreta spectrum include the absence of a hypoechogenic retroplacental space, bladder-wall interruption, abnormal placental lacunae, placental hypervascularity, aberrant vessels penetrating the posterior wall of the bladder. The labor management strategy was individually tailored by a multidisciplinary Concilium with the participation of obstetricians, neonatologists, anesthesiologists, and a transfusion medicine specialist.
The primary endpoint of the study was the possibility of reducing intraoperative blood loss during distal tourniquet compression hemostasis in combination with vaginal balloon tamponade using the Zhukovsky vaginal catheter versus distal tourniquet compression hemostasis only during delivery of pregnant women with placenta accreta spectrum. For this purpose, intraoperative blood loss, measured by the gravimetric method, and analysis of perioperative hemoglobin level dynamics were performed in both groups. Volumes of intraoperative reinfusion of washed red blood cells and donor blood components were also evaluated. The second endpoint of the study was the effect of the compared surgical treatment methods of the placenta accreta spectrum on its outcomes for patients. For this purpose, a comparative analysis of complications, operative time and hospital length of stay was performed.
Statistical analysis
Statistical analysis was performed using MS EXCEL 2010 and Statistica 10 software (StatSoft., Russia). Descriptive statistics included median (Me), 25% and 75% percentiles (P25 and P75); nonparametric tests were used to determine the significance of differences. Binary variables are presented as counts and percentages. Continuous variables were compared with the Mann–Whitney U test. Categorical variables were compared using the Chi-square test (χ2) or Fisher's exact test. The final results for binary outcomes were reported using odds ratios (OR) with 95% confidence intervals (CI). The significance threshold was defined as p<0.05.
Results
There were no differences between the study groups in age, body mass index, and number of previous CSs (Table 1). The mean age of patients was 35 years in Group 1 and 33 years in Group 2, which was aimed at preserving the reproductive function.
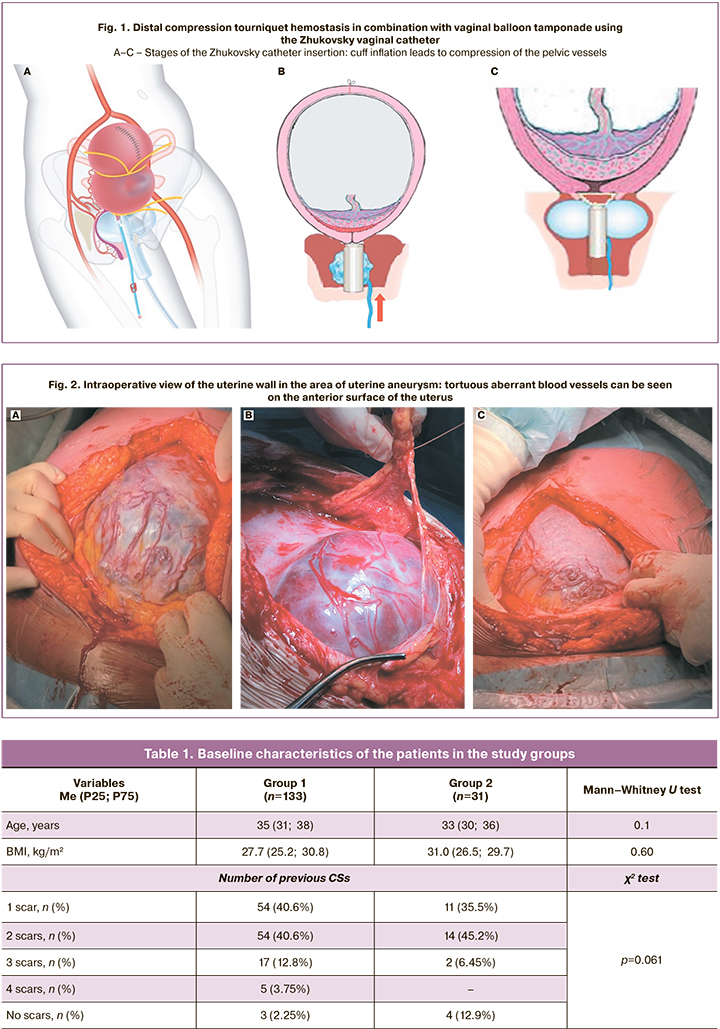
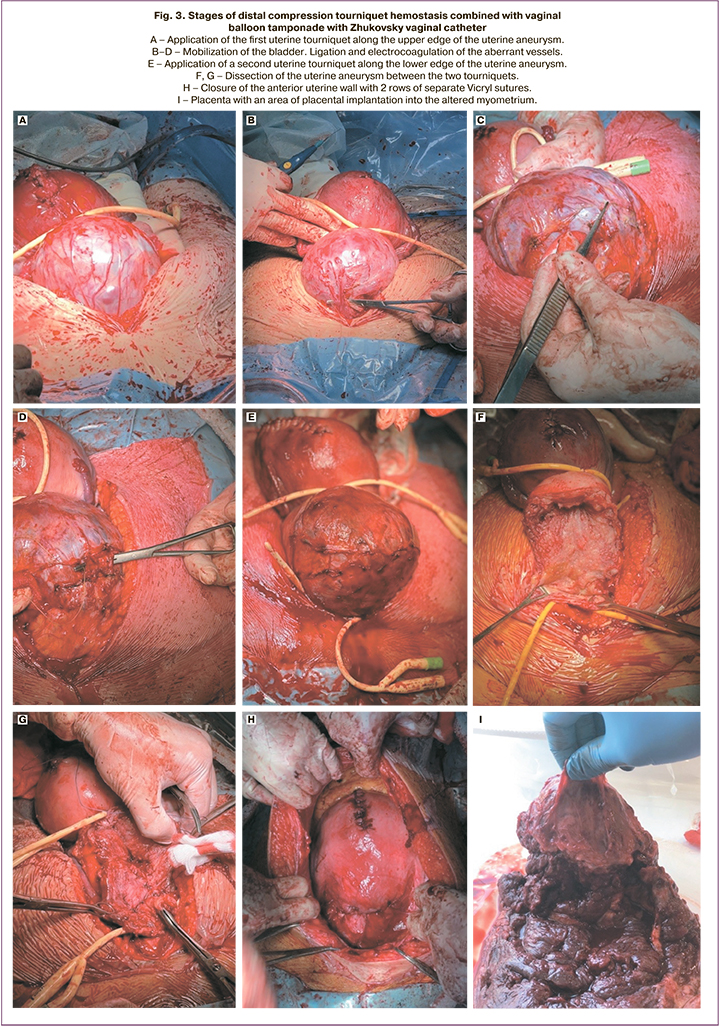
The method consists of combining distal compression hemostasis with the simultaneous use of tourniquets and vaginal balloon tamponade with a Zhukovsky vaginal catheter. The method is shown in the figures (Fig. 1–3).
After performing a lower abdominal midline incision passing around the umbilicus, the fetus was extracted via uterine fundus CS, then the umbilical cord was cut and immersed in the uterus, and the placenta was not separated. The uterine fundal incision was closed by two rows with separate Vicryl sutures.
The Zhukovsky vaginal catheter was inserted during the uterine incision closure and filled with 180–200 ml of physiological solution (Fig. 1), ensuring compression (tamponade) of the vaginal branches of the uterine and pudendal arteries. The first uterine tourniquet was placed along the upper edge of the uterine aneurysm around the uterus, capturing the broad uterine ligaments with fallopian tubes on both sides in a single block. When the first uterine tourniquet was placed, the ascending branches of the uterine arteries and ovarian arteries were clamped. Then the peritoneum of the vesicoureteral fold was dissected. Large vessels were ligated and cut, and small vessels were coagulated. The bladder was mobilized to the border of healthy uterine tissue (to the lower edge of the uterine aneurysm). The second uterine tourniquet was placed around the uterus at the level of the lower edge of the uterine aneurysm in a single block with capture of broad uterine ligaments. The ureteral arteries were clamped while the second tourniquet was applied. Then, the dehiscent uterine wall was dissected, including uterine aneurysm with a placental implantation site within healthy tissues. Remaining placental tissue was removed manually and surgically. The placental site was sutured with separate Vicryl sutures, if necessary. Then, the lower uterine segment was closed by two rows with separate Vicryl sutures. The tourniquets were removed. The wound to the anterior abdominal wall was tightly sutured. The vaginal catheter was removed 4–6 hours after its placement.
The volume of intraoperative blood loss, which was assessed by the gravimetric method, was the key indicator of hemostasis efficiency in our study. Intraoperative blood loss volume in Group 1 was lower than in Group 2. The median volume of intraoperative blood loss in groups 1 and 2 was 959 (699; 1651) and 1549 (899.5; 2098) ml (p=0.03), respectively. At the same time, hemoglobin levels before delivery were comparable in both groups. In the postoperative period there was a decrease in hemoglobin in Group 2 where isolated distal compression hemostasis with tourniquet was performed compared to Group 1 where distal compression hemostasis with tourniquet was combined with vaginal balloon tamponade using a Zhukovsky catheter. The volume of autotransfusion in the study group was 208 ml versus 485 ml in the comparison group. The differences were significant (p<0.05, Mann–Whitney test) (Table 2). Transfusion of packed red blood cells was required in 12/133 (9%) cases in the study group, and in 13/31 (42%) cases in the comparison group. The findings indicated a high frequency of donor red blood cell transfusion in the comparison group, with an OR value of 7.3 (95% CI 2.88–18.42; p=0.00004). Transfusion of donor fresh frozen plasma was performed more frequently in Group 2 – 12/31 (38.7%) than in Group 1 – 2/133 (1.5%). The OR was 41.4 (95% CI 8.6–199.3; p<0.0001). There were no significant differences between the groups in terms of operative time and hospital length of stay after surgery.
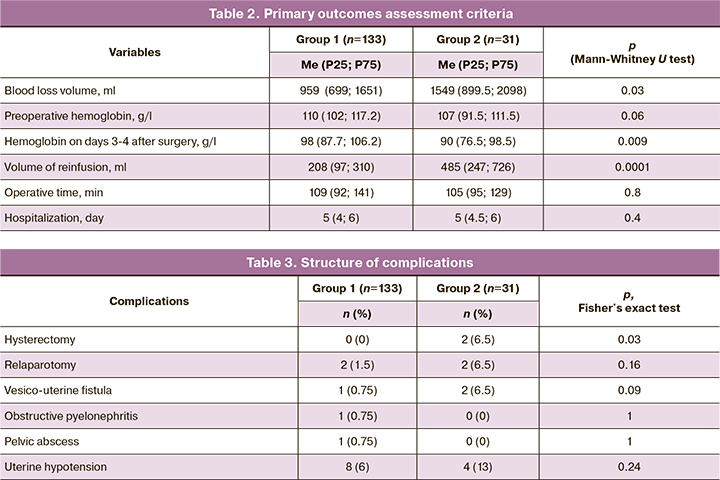
The structure of the complications is presented in Table 3. It should be noted that organ-sparing surgery in the study group (n=133) was performed in 133/133 (100%) cases, in the control group (n=31) in 29/31 (93.5%) (p=0.03). Damage to the ureters was not observed in any group. Relaparotomy was required in 2/133 (1.5%) cases in Group 1 and 2/31 (6.5%) cases in Group 2, respectively (p=0.16). The indication for relaparotomy in Group 2 was bleeding in the early postoperative period (n=2), and in Group 1 we performed relaparotomy in the delayed postoperative period due to pelvic abscess (n=1) and development of dynamic intestinal obstruction (n=1). Intraoperative uterine hypotension was observed in Group 1 in 8/133 (6%) cases, in Group 2 in 4/31 (13%) cases. Compression sutures were used in all cases when this complication developed. There was no bleeding in the postoperative period in the study group. Vesicoureteral fistulas were diagnosed in 1/133 (0.75%) and 2/31 (6.5%) a month after surgery in Groups 1 and 2, respectively (p=0.09). In Group 1, the fistula subsequently closed spontaneously, while in Group 2 it required excision of the vesicoureteral fistula, in one case using laparoscopic access, and in the other using laparotomy. In one case, the study group patient was diagnosed with obstructive pyelonephritis in the postoperative period due to edema of the ureters against the background of their catheterization before surgery. Thus, the complications during the surgical intervention with the tourniquet hemostasis method were minimal.
Discussion
Organ-sparing surgery in pregnant women with a placenta accreta spectrum aims to preserve the uterus and reproductive function. Palacios-Jaraquemada JM was first proposed in 2004 to dissect the uterine wall in the area of the placenta accreta spectrum with further reconstruction of the uterus. [14, 15]. The extraction of the fetus was performed through a fundal uterine incision after ligation of the newly formed vessels between the uterus and the bladder. The placenta and the uterine wall were dissected in one block within healthy tissues with further restoration of uterine integrity.
In Russia, Kurtser, MD, was the founder of organ-sparing surgery in pregnant women with placenta implantation on a previous uterine scar. Initially, ligation of the internal iliac arteries was performed for hemostasis and compression sutures were applied to the uterus [16, 17]. Later, temporary balloon occlusion of the common iliac arteries was introduced into practice. The use of this technique led not only to a decrease in the number of patients with massive blood loss, but also to a decrease in the median blood loss in the remaining patients, which was 1000-1450 ml [18].
The method of distal compression hemostasis using tourniquets has become an alternative to endovascular methods [19, 20]. The method consists of the following: after performing CS by fundal uterine incision and suturing the uterus in the broad ligaments at the level of the isthmus, "windows" were formed on both sides, through which tourniquets were applied along the uterine side. Further, a third tourniquet was placed through the same windows and tightened, after which uterine aneurysm dissection was performed [21]. The advantages of this method were that there was no need to use expensive equipment for balloon vessel occlusion, as well as a significant reduction in intraoperative blood loss. The authors of China reported similar findings in a study investigating the tourniquet technique [22].
In 2019, the method of surgical delivery of patients with placenta accreta spectrum using distal compression hemostasis with the use of tourniquets was developed and patented at the Vidnovsky Perinatal Center. Later, this method was supplemented by vaginal tamponade with a Zhukovsky vaginal catheter [23, 24].
The proposed method was used in the surgical delivery of 133 pregnant women with the placenta accreta spectrum. Organ-sparing surgery was performed in 100% of the cases. There was no need for transfusion of donor blood components. The duration of the operation was averaged 109 minutes; mean blood loss was 959 ml; mean blood reinfusion volume was 208 ml; mean hospital stay was 5 days.
Our study showed the advantages of the proposed method for organ sparing surgery in patients with placenta accreta spectrum. The simplicity and accessibility of hemostasis is achieved due to the following factors: mobilization and constriction of the common iliac arteries is excluded, imposition of circular tourniquets does not require additional mobilization of surrounding tissues. Reliability of hemostasis is increased by temporary cessation of blood flow in the distal vascular bundles from various main sources of uterine blood supply: uterine and ovarian arteries. Installation of the Zhukovsky vaginal catheter allows additional compression of the vaginal branches of the uterine arteries and the pudendal arteries, preventing bleeding at these stages of surgical delivery. The use of distal compression hemostasis using tourniquets in combination with vaginal balloon tamponade with Zhukovsky vaginal catheter reduces the amount of blood loss by clamping the maximum number of vessels providing the uterine blood supply. The proposed method can be performed by an obstetrician gynecologist without the involvement of a vascular surgeon. An ischemic zone occurs between the two tourniquets, allowing the operating obstetrician-gynecologist to work practically in the "dry" surgical field.
Conclusion
The proposed method of distal compression hemostasis using tourniquets in combination with vaginal balloon tamponade with the Zhukovsky vaginal catheter in patients with placenta accreta spectrum resulted in a 1.6-fold decrease in blood loss compared to distal tourniquet hemostasis alone. At the same time, the number of complications in the study group was minimal, which significantly reduced the number of transfusions of packed red blood cells and fresh frozen plasma, as well as shortened the time of rehabilitation in the postoperative period due to the preservation of hemoglobin levels closer to normal values.
References
- Say L., Chou D., Gemmill A., Tunсalp O., Moller A., Daniels J. et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Heal. 2014; 2(6): 323-33. https://dx.doi.org/10.1016/s2214-109x(14)70227-x.
- Ящук А.Г., Лутфарахманов И.И., Мусин И.И., Бирюков А.А., Решетникова Л.Р., Мингазов Н.Н., Галимова Э.Р., Молоканова А.Р. Органосохраняющие операции при истинном приращении плаценты. Практическая медицина. 2019; 17(4): 52-6. https://dx.doi.org/10.32000/2072-1757-2019-4-52-56. [Yashchuk A.G., Lutfarakhmanov I.I., Musin I.I., Biryukov A.A., Reshetnikova L.R., Mingazov N.N., Galimova E.R., Molokanova A.R. Organ preservation operations with placenta accreta. Practical Medicine. 2019; 17(4): 52-6. (in Russian)]. https://dx.doi.org/10.32000/2072-1757-2019-4-52-56.
- Jauniaux E., Chantraine F., Silver R.M., Langhoff-Roos J.; FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int. J. Gynaecol. Obstet. 2018; 140(3): 265-73. https://dx.doi.org/10.1002/ijgo.12407.
- Kyozuka H., Yamaguchi A., Suzuki D., Fujimori K., Hosoya M., Yasumura S.et al.; Japan Environment and Children’s Study (JECS) Group. Risk factors for placenta accreta spectrum: findings from the Japan environment and Children's study. BMC Pregnancy Childbirth. 2019; 19(1): 447.https://dx.doi.org/10.1186/s12884-019-2608-9.
- Thurn L., Lindqvist P.G., Jakobsson M., Colmorn L.B., Klungsoyr K., Bjarnadóttir R.I. et al. Abnormally invasive placenta-prevalence, risk factors and antenatal suspicion: results from a large population-based pregnancy cohort study in the Nordic countries. BJOG. 2016; 123(8): 1348-55. https://dx.doi.org/10.1111/1471-0528.13547.
- Collins S.L., Alemdar B., van Beekhuizen H.J., Bertholdt C., Braun T., Calda P. et al. Evidence-based guidelines for the management of abnormally invasive placenta: recommendations from the International Society for Abnormally Invasive Placenta. Am. J. Obstet. Gynecol. 2019; 220(6): 511-26.https://dx.doi.org/10.1016/j.ajog.2019.02.054.
- Warshak C.R., Ramos G.A., Eskander R., Benirschke K., Saenz C.C., Kelly T.F. et al. Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet. Gynecol. 2010; 115(1): 65-9. https://dx.doi.org/10.1097/AOG.0b013e3181c4f12a.
- Eller A.G., Porter T.F., Soisson P., Silver R.M. Optimal management strategies for placenta accreta. BJOG. 2009; 116(5): 648-54. https://dx.doi.org/10.1111/j.1471-0528.2008.02037.x.
- Cahill A.G., Beigi R., Heine R.P., Silver R.M., Wax J.R. Placenta accreta spectrum. Am. J. Obstet. Gynecol. 2018; 219(6): B2-B16. https://dx.doi.org/10.1016/j.ajog.2018.09.042.
- Silver R.M., Branch D.W. Placenta accreta spectrum. N. Engl. J. Med. 2018; 378(16): 1529-36. https://dx.doi.org/10.1056/NEJMcp1709324.
- O'Brien J.M., Barton J.R., Donaldson E.S. The management of placenta percreta: conservative and operative strategies. Am. J. Obstet. Gynecol. 1996; 175(6): 1632-8. https://dx.doi.org/10.1016/s0002-9378(96)70117-5.
- Wright J.D., Silver R.M., Bonanno C., Gaddipati S., Lu Y.S., Simpson L.L. et al. Practice patterns and knowledge of obstetricians and gynecologists regarding placenta accreta. J. Matern. Fetal Neonatal Med. 2013; 26(16): 1602-9.https://dx.doi.org/10.3109/14767058.2013.793662.
- Cal M., Ayres-de-Campos D., Jauniaux E. International survey of practices used in the diagnosis and management of placenta accreta spectrum disorders. Int. J. Gynaecol. Obstet. 2018; 140(3): 307-11. https://dx.doi.org/10.1002/ijgo.12391.
- Sentilhes L., Kayem G., Chandraharan E., Palacios-Jaraquemada J., Jauniaux E.; FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. Int. J. Gynaecol. Obstet. 2018; 140(3): 291-8. https://dx.doi.org/10.1002/ijgo.12410.
- Palacios-Jaraquemada J.M., Fiorillo A., Hamer J., Martínez M., Bruno C. Placenta accreta spectrum: a hysterectomy can be prevented in almost 80% of cases using a resective-reconstructive technique. J. Matern. Fetal Neonatal Med. 2022; 35(2): 275-82. https://dx.doi.org/10.1080/14767058.2020.1716715.
- Курцер М.А., Лукашина М.В., Панин А.В., Штабницкий А.М.,Алексеева Т.В., Бреусенко Л.Е., Бреслав И.Ю. Истинное врастание плаценты. Органосохраняющие операции. Вопросы гинекологии, акушерства и перинатологии. 2009; 8(5): 31-5. [Kurtser M.A., Lukashina M.V., Panin A.V.б Shtabnitskiy A.M., Alekseeva T.V., Breusenko L.E., Breslav I.Yu. Placenta accreta. Organ-saving surgery. Issues of Gynecology, Obstetrics and Perinatology. 2009; 8(5): 31-5. (in Russian)].
- Курцер М.А., Бреслав И.Ю., Лукашина М.В., Штабницкий А.М., Панин А.В., Алексеева Т.В., Платицын И.В. Опыт осуществления органосохраняющих операций при врастании плаценты. Акушерство и гинекология. 2011; 8: 86-90. [Kurtser M.A., Breslov I.Yu., Lukashina M.V., Shtabnitsky A.M.,Panin A.V., Alekseyeva T.V., Platitsyn I.V. Experience with organ-sparing surgery for placenta accreta. Obstetrics and Gynecology. 2011; 8: 86-90.(in Russian)].
- Курцер М.А., Бреслав И.Ю., Григорян А.М., Латышкевич О.А.,Кутакова Ю.Ю., Кондратьева М.А. Временная баллонная окклюзия общих подвздошных артерий при осуществлении органосохраняющих операций у пациенток с врастанием плаценты. Акушерство и гинекология: новости, мнения, обучение. 2018; 6(4): 31-7. https://dx.doi.org/10.24411/2303-9698-2018-14003. [Kurtser M.A., Breslav I.Yu.,Grigorian A.M., Latyshkevich O.A., Kutakova Yu.Yu., Kondratieva M.A. Temporary balloon occlusion of common iliac arteries during organ preservation surgery in patients with placenta ingrowth. Obstetrics and gynecology: News, Opinions, Training. 2018; 6(4): 31-7. (in Russian)]. https://dx.doi.org/10.24411/2303-9698-2018-14003.
- Шмаков Р.Г., Пирогова М.М., Васильченко О.Н., Чупрынин В.Д.,Ежова Л.С. Хирургическая тактика при врастании плаценты с различной глубиной инвазии. Акушерство и гинекология. 2020; 1: 78-82. https://dx.doi.org/10.18565/aig.2020.1.78-82. [Shmakov R.G., Pirogova M.M., Vasilchenko O.N., Chuprynin V.D., Ezhova L.S. Surgery tactics for placenta increta with different depths of invasion. Obstetrics and Gynecology. 2020; 1: 78-82. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.1.78-82.
- Виницкий А.А., Шмаков Р.Г., Чупрынин В.Д. Сравнительная оценка эффективности методов хирургического гемостаза при органосохраняющем родоразрешении у пациенток с врастанием плаценты. Акушерство и гинекология. 2017; 7: 68-74. https://dx.doi.org/10.18565/aig.2017.7.68-74. [Vinitskiy A.A., Shmakov R.G., Chuprynin V.D. Comparative evaluation of the effectiveness of surgical hemostasis methods for organ-preserving delivery in patients with placental ingrowth. Obstetrics and Gynecology. 2017; 7: 68-74.(in Russian)]. https://dx.doi.org/10.18565/aig.2017.7.68-74.
- Шмаков Р.Г., Чупрынин В.Д., Виницкий А.А. Комплексный компрессионный гемостаз при выполнении органосохраняющего оперативного родоразрешения у пациенток с врастанием плаценты. Патент на изобретение RU 2627633 C, 09.08.2017. Заявка № 2016148856 от 13.12.2016. [Shmakov R.G., Chuprynin V.D., Vinnitskiy A.A. Complex compression hemostasis during organ-preserving operative delivery in patients with placenta accreta. Patent for the invention RU 2627633 C, 09.08.2017. Application no. 2016148856 dated 13.12.2016. (in Russian)].
- Meng J.L., Gong W.Y., Wang S., Ni X.J., Zuo C.T., Gu Y.Z. Two-tourniquet sequential blocking as a simple intervention for hemorrhage during cesarean delivery for placenta previa accrete. Int. J. Gynaecol. Obstet. 2017; 138(3):361-2. https://dx.doi.org/10.1002/ijgo.12199.
- Куликов И.А., Белоусова Т.Н., Соваев Н.И., Плахотина Е.Н., Милютина Е.Р.,Павлютина К.М., Латышев Р.В. Способ оперативного родоразрешения пациенток с врастанием плаценты в рубец на матке с использованием турникетного гемостаза. Патент на изобретение RU 2708369 C1, 05.12.2019. Заявка №2019112811 от 26.04.2019. [Kulikov I.A., Belousova T.N.,Sovaev N.I., Plakhotina E.N., Milyutina E.R., Pavlyutina K.M., Latyshev R.V.Method of operative delivery of patients with placenta ingrowth into the uterine scar using turnstile hemostasis. Patent for the inventionRU 2708369 C1, 05.12.2019. Application No. 2019112811 dated 26.04.2019. (in Russian)].
- Куликов И.А., Белоусова Т.Н., Соваев Н.И., Плахотина Е.Н., Мусаева С.В., Павлютина К.С., Петров А.Е. Способ оперативного родоразрешения пациенток с врастанием плаценты в рубец на матке. Патент на изобретение RU 2706368 C1, 18.11.2019. Заявка №2019118817 от 18.06.2019. [Kulikov I.A., Belousova T.N., Avaev N.I., Plakhotina E.N., Musaeva S.V., Pavlyutina K.S., Petrov A.E. Method of operative delivery of patients with placenta ingrowth into the uterine scar. Patent for the invention RU 2706368 C1, 18.11.2019. Application no.2019118817 dated 06/18/2019. (in Russian)].
Received 05.07.2022
Accepted 10.08.2022
About the Authors
Ilyas A. Kulikov, PhD, Head of the Department of Pregnancy Pathology, Vidnovsky Perinatal Center, +7(916)752-86-97, aesculap@inbox.ru,https://orcid.org/0000-0002-2460-1623, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Roman G. Shmakov, Dr. Med. Sci., Professor, Director of the Institute of Obstetrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics,
Gynecology and Perinatology, Ministry of Health of the Russian Federation, +7(495)438-72-00, r_shmakov@oparina4.ru, https://orcid.org/0000-0002-2206-1002,
117997, Russian Federation, Moscow, Oparina str., 4.
Tamara N. Belousova, PhD, Head Physician, Vidnovsky Perinatal Center, beltamara1@mail.ru, https://orcid.org/0000-0003-3804-7691,
142700, Russia, Moscow Region, Zavodskaya str., 17.
Elena N. Plakhotina, Dr. Med. Sci., Head of the Department of Anesthesiology and Intensive Care, Vidnovsky Perinatal Center, https://orcid.org/0000-0002-6793-2318, enp2004@inbox.ru, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Natalia V. Nizyaeva, Dr. Med. Sci, Head of the Laboratory of Pathology, Avtsyn Research Institute of Human Morphology, SPIN-code: 9893-2630,
https://orcid.org/0000-0001-5592-5690, niziaeva@gmail.com, 117418, Moscow, Tsyurupy street, 3
Dzhangar D. Iskakov, Physician at the Department of Pregnancy Pathology, Vidnovsky Perinatal Center, iskakov.jangar@yandex.ru, https://orcid.org/0000-0002-8267-699X, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Ekaterina R. Milyutina, Physician at the Department of Pregnancy Pathology, Vidnovsky Perinatal Center, milyutina.kate@mail.ru, https://orcid.org//0000-0003-2701-0607, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Elena A. Vdovichenko, Physician at the Department of Pregnancy Pathology, Vidnovsky Perinatal Center, e.vdovichenko.00@mail.ru, https://orcid.org//0000-0003-2385-7106, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Irina A. Geilis, Head of the Department of Antenatal Fetal Protection and Perinatal Diagnostics, Vidnovsky Perinatal Center,
dr.irina71@mail.ru, https://orcid.org//0000-0002-5000-8647, 142700, Russia, Moscow Region, Zavodskaya str., 17.
Denis V. Prochakovsky, Anesthesiologist-Intensivist at the Department of Anesthesiology and Resuscitation, Vidnovsky Perinatal Center,
https://orcid.org//0000-0003-2403-7185, Russia, Moscow Region, Zavodskaya str., 17.
Corresponding author: Ilyas A. Kulikov, aesculap@inbox.ru
Authors' contributions: Kulikov I.A., Shmakov R.G., Belousova T.N. – conception and design of the study; Kulikov I.A., Geilis I.A., Nizyaeva N.V., Iskakov D.D., Milyutina E.R., Vdovichenko E.A., Prochakovsky D.V. – material collection and analysis; Kulikov I.A., Plakhotina E.N. – statistical analysis; Kulikov I.A. – manuscript drafting; Shmakov R.G., Plakhotina E.N. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Vidnovsky Perinatal Center.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kulikov I.A., Shmakov R.G., Belousova T.N., Plakhotina E.N., Nizyaeva N.V.,
Geilis I.A., Iskakov D.D., Milyutina E.R., Vdovichenko E.A., Prochakovsky D.V.
Efficacy of the tourniquet hemostasis combined with vaginal balloon tamponade using
a Zhukovsky vaginal catheter during delivery in placenta accreta spectrum
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 10: 58-66 (in Russian)
https://dx.doi.org/10.18565/aig.2022.10.58-66



