Association between the levels of heavy metals and IVF outcomes in women with infertility
Aim. To analyze the association between the levels of heavy metals (cadmium, mercury, lead) in the blood of patients with infertility and the outcomes of assisted reproductive technology (ART) programs.Syrkasheva A.G., Frankevich V.E., Dolgushina N.V.
Materials and methods. Infertility treatment by ART was carried out in 301 couples. The levels of mercury, cadmium, and lead were determined in the blood of patients by ICP-MS. The medians of heavy metal levels were evaluated in patients with different outcomes of ART (clinical pregnancy rate, live birth rate, cumulative live birth rate), as well as the ratio between the quartile groups of metals and different outcomes of ART.
Results. The levels of cadmium were statistically significantly higher in smoking patients compared to non-smokers. The median levels of cadmium, mercury and lead did not differ in patients with different outcomes of ART cycles. In different subgroups stratified by quartiles based on cadmium levels, a comparable frequency of clinical outcomes of ART were observed (the rates of clinical pregnancy, live births, cumulative live births). In patients with the highest cadmium level quartile (Q4), no blastocysts for embryo transfer could be obtained significantly more often – OR 2.95 (95% CI 1.22–7.02). When comparing mercury quartile groups, no statistically significant differences were noted. A decrease (but not statistically significant) in the rates of clinical pregnancy and live birth was noted along with an increase in the lead level quartile (Q1–Q4).
Conclusion. An increase in cadmium level is associated with a 3-fold increase in the risk of lack of blastocysts for embryo transfer, and an increase in lead level (Q1–Q4) led to a 10% decrease in the rates of the clinical pregnancy and live birth.
Keywords
Infertility is an important medical and social problem: according to different publications, 5–15% of married couples in the world face problems with conception during the first year of unprotected sex in marriage. The causes of infertility are variable, but in recent decades, the scientists pay increasingly greater attention to the impact of anthropogenic chemicals (heavy metals, pesticides, and various organic compounds) on human reproduction.
Certain heavy metals (cadmium, mercury, lead) are widespread pollutants being on the top of the list of toxic substances in the Comprehensive Environmental Response, Compensation, and Liability Act of 1980 (CERCLA).
It is known, that the adverse impact of heavy metals on reproduction can be both direct and indirect, for example, through formation of toxic metabolites. According to some publications, increased exposure to heavy metals is associated with impaired menstrual cycle, miscarriage, and an increased risk of preterm birth. [1, 2]. The data on the negative effect of heavy metals on folliculogenesis, spermatogenesis, corpus luteum function and the hypothalamic-pituitary system were mainly obtained from the studies on animal models. [3, 4]. At the same time, the results of studies in humans are contradictory. This may be due to the heterogeneity of the patients selected for the study (mainly, they are the patients of the reproductive clinics), a small number of selected patients, multiple confounders, and short list of the studied substances.
Purpose of the study: to analyze the association between the levels of heavy metals (cadmium, mercury, lead) in the blood of patients with infertility and the outcomes of assisted reproductive technology (ART) programs.
Materials and methods
The prospective study included 301 married couples, who applied for infertility treatment via ART in the period from 2017 to 2018. They had no contraindications for ART and signed an informed consent to participate in the study. The inclusion criteria were the normal karyotype of both spouses, the absence of severe pathozoospermia (100% teratozoospermia, absolute asthenozoospermia, all types of azoospermia), the women's age 18–39 years, and the women's body mass index (BMI) from 19 to 25 kg/m2 inclusively. The exclusion criteria were the use of donor gametes or surrogacy, as well as obtaining 3 or less oocytes.
All married couples participating in the study were examinedaccordingtothe Order№ 107ndated 30.08.2012 of the Ministry of Health of Russia «About the use of assisted reproductive technologies; contraindications and limitations on the use» [3].
Ovarian stimulation was performed with gonadotropin-releasing hormone antagonists according to the protocol. The dose of gonadotropins was selected individually. The ovulation trigger was administered when the follicles reached the diameter 17 mm or more. Human chorionic gonadotropin (HCG) 8000– 10,000 IU or a gonadotropin releasing hormone agonist 0.2 mg was used as the ovulation trigger. The support of the luteal phase and post-transfer period in all patients was carried out according to the standard protocol [5].
Venous blood collection for the study was carried out on the day of transvaginal puncture, after which the samples were cryopreserved at t = -700C. The levels of mercury, cadmium, and lead were determined by inductively coupled plasma-mass spectrometry (ICP-MS), and the specialists of the laboratory had no access to the clinical characteristics of the patients.
Fertilization of oocytes was carried out using classical in vitro insemination (IVF) or intracytoplasmic sperm injection (ICSI) [5]. During fertilization, morphological assessment of oocytes was carried out, and the presence of cytoplasmic dysmorphisms was determined. Cytoplasmic dysmorphisms included the presence of central cytoplasmic granularity, abnormal aggregates of the smooth endoplasmic reticulum in the cytoplasm, or cytoplasmic vacuoles. Cultivation and embryo transfer was carried out according to the standard clinical practice.
14 days after embryo transfer, the serum concentration of β-hCG was determined. 5 weeks after embryo transfer, the embryo's heartbeat was visualized, and the clinical pregnancy was stated. 40 weeks after embryo transfer, the patients were interviewed by telephone to analyze the pregnancy outcomes. Clinical pregnancy rate was calculated as the ratio between the number of clinical pregnancies and the total number of cycles. Live birth rate was defined as the ratio between the number of live births and the total number of cycles. Cumulative live birth rate was defined as the ratio between the number of live births per started cycle and live births after the transfer of thawed embryos obtained in a given IVF or ICSI cycle and the total number of cycles.
Statistical analysis
The statistical software package Statistica 10 (USA) was used for analysis. Normally distributed data were presented as the mean (standard deviation). The statistical analysis was performed using χ2-test to compare categorical variables and t-test – to compare mean values. Abnormally distributed data were presented as median (the interquartile range). The measure of association for binary comparisons was odds ratio (OR) with a 95% confidence interval (95% CI). The patients were stratified into subgroups by different metal levels in blood, depending on the quartile value (Q1: 0–25 percentile, Q2: 25–50 percentile, Q3: 50–75 percentile, Q4: 75–100 percentile).
The differences between the statistical values were considered statistically significant at the level р˂0,05.
The study was approved by the Ethics Commission of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology of the Ministry of the Healthcare of Russian Federation.
Results
Concentrations of cadmium, mercury and lead in the body of the female patients are presented in Table 1.
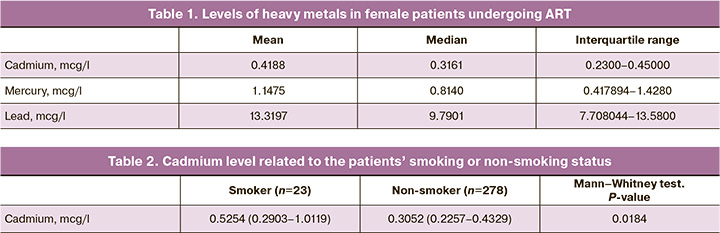
First, the relationship between the level of heavy metals and clinical and anamnestic characteristics was analyzed. Cadmium levels were significantly higher in female smokers than in non-smokers (Table 2).
Then, the factors affecting the conception in the selected patients were analyzed. For this, all patients were stratified into 2 groups: group 1 (n=137) – clinical pregnancy occurred in the treatment cycle, group 2 (n=164) – clinical pregnancy did not occur in the treatment cycle. The obtained data are presented in Table 3. The main clinical characteristics of the patients did not differ significantly in the comparison groups. The only difference was the duration of infertility, which was statistically significantly higher in the group of patients who failed to conceive.
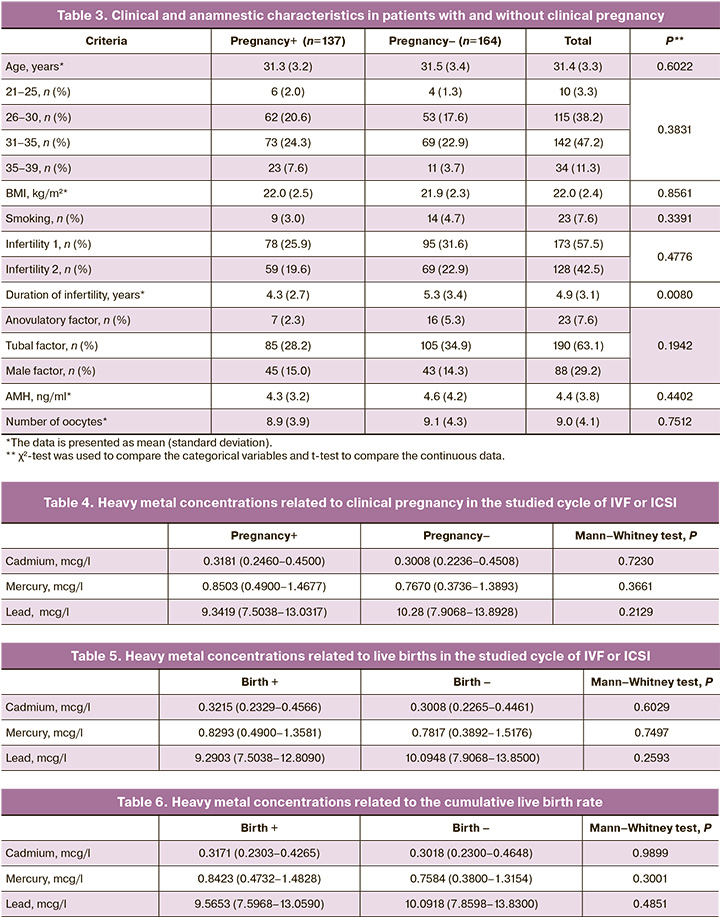
Then, the effect of the level of heavy metals on the onset of clinical pregnancy, live births and the cumulative frequency of live births was assessed. The obtained data are presented in Tables 4–6.
The analysis of the obtained data showed, that the median levels of cadmium, mercury and lead did not differ in patients with different outcomes of ART cycles. Therefore, for further analysis, the subgroups of patients were formed based on different levels of metals in blood depending on the quartile value (Q1: 0–25 percentiles, Q2: 25–50 percentiles, Q3: 50–75 percentiles, Q4 75–100 percentiles). In subgroups Q1–Q4, the rate of oocytes with cytoplasmic dysmorphisms, the rate of ET cancellation due to embryo cleavage failure, as well as the clinical pregnancy, live births, and the cumulative live births rates were analyzed. The data are summarized in Tables 7–9.
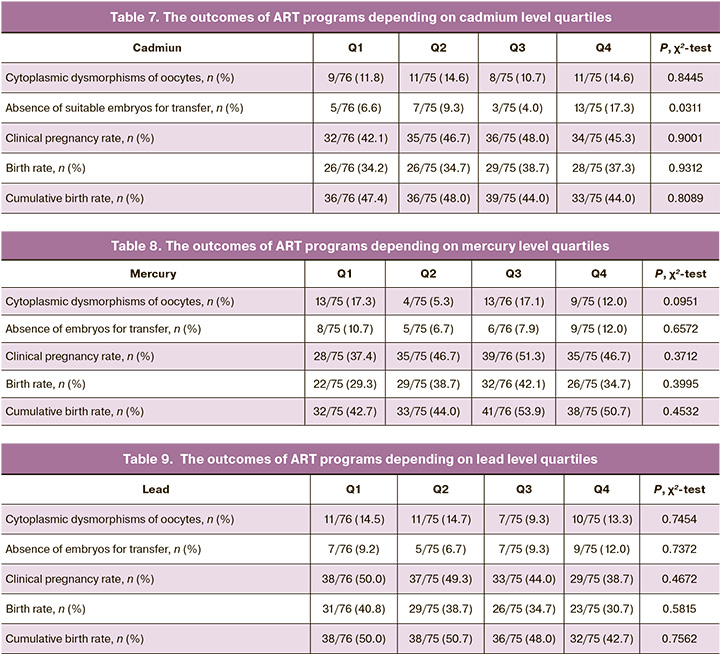
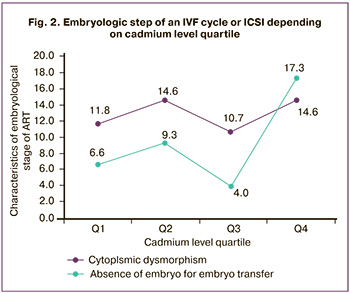
In different subgroups of cadmium level quartiles, comparable ART outcomes – pregnancy rate, birth rate, and cumulative birth rate were observed. Interestingly, in patients with the highest cadmium levels (Q4), embryo cleavage failure was significantly more often observed; this may be due to the impact of cadmium on genetic or metabolic mechanisms of oocytes development, which did not manifest themselves morphologically, since the frequency of cytoplasmic dysmorphisms of oocytes did not differ in quartile groups. The OR for embryo cleavage failure at cadmium level Q4 was 2.95 (95% CI: 1.22; 7.02).
 The comparison of mercury quartile groups showed no statistically significant differences. The rate of embryo cleavage failure was to some extent higher in groups Q1 and Q4. However, the differences were not significant (Table 8).
The comparison of mercury quartile groups showed no statistically significant differences. The rate of embryo cleavage failure was to some extent higher in groups Q1 and Q4. However, the differences were not significant (Table 8).
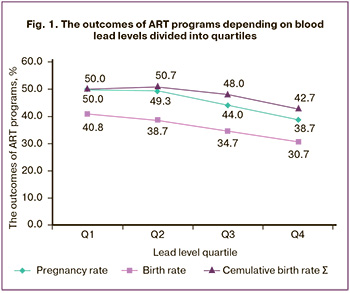
A decrease in the pregnancy and birth rates was associated with an increase in the level of lead, although the obtained differences did not reach statistical significance (Table 9, Fig.1).
The effect of an increase in cadmium level on the rate of cytoplasmic dysmorphisms of oocytes and the absence of embryos suitable for embryo transfer are shown in Fig. 2.
Discussion
Heavy metals are used in industry for a long time. Some heavy metals in low concentrations are necessary for humans and animals (for example, iron, copper and zinc), while other metals (mercury, cadmium, lead) do not participate in metabolism, but have the ability to accumulate in various tissues. Heavy metals are characterized by their widespread, toxicity, long elimination half-time and the ability to penetrate through the histohematogenous barrier. High exposure to heavy metals is considered to be one of the reasons for the gradual decrease in ejaculate quality and an increase in the incidence of infertility.
 This study examined the association between the levels of mercury, lead and cadmium in women’s blood and the outcomes of ART programs. The assessment of the clinical and anamnestic characteristics of the patients showed an association between an increase in cadmium levels and the smoking habit in women. Smoking may lead to an increase in the body concentration of heavy metals, as shown in the previous studies [6].
This study examined the association between the levels of mercury, lead and cadmium in women’s blood and the outcomes of ART programs. The assessment of the clinical and anamnestic characteristics of the patients showed an association between an increase in cadmium levels and the smoking habit in women. Smoking may lead to an increase in the body concentration of heavy metals, as shown in the previous studies [6].
The comparison of the medians of metal levels in patients with different outcomes of ART cycles showed no significant differences. At the same time, an increase in cadmium level was associated with an increase in the risk of embryo cleavage failure by almost 3 times, and an increase in lead levels (Q1 → Q4) led to a decrease in pregnancy and birth rates by 10%.
It should be noted that the results of analogous studies in various countries of the world are often contraversial. [2, 7–10]. The contradictions in the studies can be explained by a complexity of research in this area: the differences in the groups of patients, biological samples, investigation methods. In addition, many factors affect the conception and birth, and even when conducting large studies, only the main factors may be taken into account. Therefore, a number of studies assess only the quality of gametes and/or levels of steroid hormones as an endpoints. [11–13]. Of great interest are those studies, in which the pathogenetic mechanisms of the impact of heavy metals on steroidogenesis, spermatogenesis, and oocyte-cumulus complexes were assessed. However, these studies were carried out on animal models and could not be entirely envisioned for humans. [3, 4]. All of the above-mentioned emphasizes the need for further study of this problem.
Conclusion
According to the results of the study, an increase in cadmium cadmium was associated with an increase in the risk of embryo cleavage failure by almost 3 times, and an increase in lead level (Q1 → Q4) led to a 10% decrease in the rate of clinical pregnancy and live births. Consequently, even low concentrations of heavy metals may have a detrimental effect on the reproductive system.
References
- Казанцева Е.В., Долгушина Н.В., Донников А.Е., Беднягин Л.А., Баранова Е.Е., Терешков П.П. Влияние пренатальной экспозиции бенз(а)пирена, стирола и формальдегида на массу тела при рождении в зависимости от полиморфизмов генов системы детоксикации. Акушерство и гинекология. 2016; 7: 68-78. [Kazantseva E.V., Dolgushina N.V., Donnikov A.E., Bednyagin L.A., Baranova E.E., Tereshkov P.P. Impact of prenatal exposure to benz[a]pyrene, styrene, and formaldehyde on birth weight in relation to detoxification system gene. Akusherstvo i ginekologiya/Obstetrics and Gynecology. 2016; (7): 68-78. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.7.68-78.
- Lee S., Min J., Min K. Female infertility associated with blood lead and cadmium levels. Int. J. Environ. Res Public Health. 2020; 17(5): 1794. https://dx.doi.org/10.3390/ijerph17051794.
- Saedi S., Shirazi M.R.J., Zamiri M.J., Totonchi M., Dadpasand M., Sedaghati F. Impaired follicular development and endocrine disorders in female rats by prepubertal exposure to toxic doses of cadmium. Toxicol. Ind. Health. 2020; 36(2): 63-75. https://dx.doi.org/10.1177/0748233720912060.
- Huang Y., Zhu J., Li H., Wang W., Li Y., Yang X. et al. Cadmium exposure during prenatal development causes testosterone disruption in multigeneration via SF-1 signaling in rats. Food Chem. Toxicol. 2020; 135: 110897. https://dx.doi.org/10.1016/j.fct.2019.110897.
- Сыркашева А.Г., Долгушина Н.В., Макарова Н.П., Ковальская Е.В., Агаршева М.А. Исходы программ вспомогательных репродуктивных технологий у пациенток с дисморфизмами ооцитов. Акушерство и гинекология. 2015; 7: 56-62. [Syrkasheva A., Dolgushina N., Makarova N., Kovalskaya E., Agarsheva M. Outcomes of assisted reproductive technology programs in patients with oocyte dysmorphisms. Akusherstvo i ginekologiya/Obstetrics and Gynecology. 2016; (7): 56-62. (in Russian)].
- Lee J.W., Kim Y., Kim Y., Yoo H., Kang H.T. Cigarette smoking in men and women and electronic cigarette smoking in men are associated with higher risk of elevated cadmium level in the blood. J. Korean Med. Sci. 2020; 35(2): e15. https://dx.doi.org/10.3346/jkms.2020.35.e15.
- Gaskins A.J., Chiu Y., Mı L., Williams P.L., Ehrlich S., Chavarro J.E. et al. Urinary bisphenol A concentrations and association with in vitro fertilization outcomes among women from a fertility clinic. Reprod. Toxicol. 2015; 30(9): 2120-8. https://dx.doi.org/10.1093/humrep/dev183.
- Bloom M.S., Fujimoto V.Y., Steuerwald A.J., Cheng G., Browne R.W., Parsons P.J. Background exposure to toxic metals in women adversely influences pregnancy during in vitro fertilization (IVF). Reprod. Toxicol. 2012; 34(3): 471-81. https://dx.doi.org/10.1016/j.reprotox.2012.06.002.
- Tolunay H.E., Şükür Y.E., Ozkavukcu S., Seval M.M., Ateş C., Türksoy V.A. et al. Heavy metal and trace element concentrations in blood and follicular fluid affect ART outcome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016; 198: 73-7. https://dx.doi.org/10.1016/j.ejogrb.2016.01.001.
- Wright D.L., Afeiche M.C., Ehrlich S., Smith K., Paige L., Chavarro J.E. et al. Hair mercury concentrations and in vitro fertilization (IVF) outcomes among women from a fertility clinic. Reprod. Toxicol. 2015; 51: 125-32. https://dx.doi.org/10.1016/j.reprotox.2015.01.003.
- Li C.J., Yeh C.Y., Chen R.Y., Tzeng C.R., Han B.C., Chien L.C. Biomonitoring of blood heavy metals and reproductive hormone level related to low semen quality. J. Hazard. Mater. 2015; 300: 815-22. https://dx.doi.org/10.1016/j.jhazmat.2015.08.027.
- Zeng Q., Zhou B., Feng W., Wang Y., Liu A., Yue J. et al. Associations of urinary metal concentrations and circulating testosterone in Chinese men. Reprod. Toxicol. 2013; 41: 109-14. https://dx.doi.org/10.1016/j.reprotox.2013.06.062.
- Zhou Y., Fu X., He D., Zou X., Wu C. Evaluation of urinary metal concentrations and sperm DNA damage in infertile men from an infertility clinic. Environ. Toxicol. Pharmacol. 2016; 45: 68-73. https://dx.doi.org/10.1016/j.etap.2016.05.020.
Received 30.07.2020
Accepted 28.10.2020
About the Authors
Anastasia G. Syrkasheva, M.D., Ph.D., Senior Researcher of the IVF Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: a_syrkasheva@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.Vladimir E. Frankevich, PhD, Head of Department of Systems Biology in Reproduction, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. Tel.: +7(495)438-07-88; -21-98. E-mail: v_frankevich@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.
Nataliya V. Dolgushina, M.D., Ph.D., M.P.H., Head of R&D Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,
Ministry of Health of the Russian Federation. E-mail: n_dolgushina@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.
For citation: Syrkasheva A.G., Frankevich V.E., Dolgushina N.V. Association between the levels of heavy metals and IVF outcomes in women with infertility. Akusherstvo i Ginecologiya/Obstetrics and Gynecology. 2020; 11: 124-130 (in Russian).
https://dx.doi.org/10.18565/aig.2020.11.124-130



