The significance of three-dimensional ultrasound in the assessment of the state of the endometrium in patients with diffuse and nodular forms of adenomyosis
Objective: To determine management tactics for patients with diffuse and nodular adenomyosis, by assessing the their functional state of the endometrium.Solomatina A.A., Ismaiilova P.D., Breusenko L.E., Shtyrov S.V., Tyumentseva M.Yu., Regul S.V., Khalifaeva Z.Z.
Materials and methods: Examinations were made in 104 patients who were ranged by groups Group 1 comprised 58 examinees with diffuse adenomyosis; Group 2 included 46 examinees with the nodular form. All the patients underwent three-dimensional ultrasound of pelvic organs. The investigators studied the thickness, volume and echostructure of the endometrium, indicators of volumetric blood flow: vascularization index (VI%); flow (FI) and vascular flow (VFI).
Results: The diffuse and nodular forms of adenomyosiosis are associated with the changes in the the thickness, the endometrial pattern, as well as with the hemodynamic parameters in the terminal branches of uterine arteries (hypovascularization, an increase in the angle-independent indices of blood flow velocity curves. The obvious uterine mucosal thinning particularly in patients with nodular adenomyosis, and which means the association with the disturbed endometrial functional state accompanied by a reduction in the implantation potential.
Conclusion: The patients with obvious endometrial thinning and the nodular form of adenomyosis, it is advisable to recommend a a reproductologist’s consultation to decide whether assisted reproductive technologies should be used. Three-dimensional ultrasound is an additional objective method for estimating the volume of the endometrium and hemodynamics in volume at the level of the basal and spiral arteries.
Authors' contributions: Solomatina A.A. – the concept and design of the investigation, editing, the final approval version for publication; Ismaiilova P.D. – the concept and the design of the investigation, material collection and processing, statistical data processing, editing; Breusenko L.E., Shtyrov S.V., Tyumentseva M.Yu., Regul S.V., Z.Z. Khalifaeva Z.Z. – material collection and processing.
Conflicts of interest: The authors declare that there are no conflicts of interest.
Funding: The investigation has not been sponsored.
Ethical Approval: The investigation has been approved by the Local Ethics Committee of N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Solomatina A.A., Ismaiilova P.D., Breusenko L.E., Shtyrov S.V.,
Tyumentseva M.Yu., Regul S.V., Khalifaeva Z.Z. The significance of three-dimensional ultrasound in the assessment of the state of the endometrium in patients with diffuse and nodular forms of adenomyosis.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (3): 83-90 (in Russian)
https://dx.doi.org/10.18565/aig.2022.268
Keywords
Endometriosis of the corpus uteri remains one of the most pressing problems of modern gynecology. The significance of the problem of adenomyosis is due to a number of factors: The prevalence of this disease among reproductive-aged women, the frequent development of severe clinical manifestations, the high rate of infertility, the unfavorable impact of this disease on reproductive outcomes, as well the significant decrease in quality of life in the patients [1–5].
From modern positions, adenomyosis is a benign disease characterized by the endometrial invasion into the myometrium, which causes uterine enlargement. The described neoplasia of the stromal component and endometrial glands of the uterus is surrounded by hypertrophic and hyperplastic muscle fibers [3, 5].
Most authors are agreed that the presence of adenomyosis is associated with morphofunctional impairments in the glandular uterine layer, which are characterized by a reduction in the nidational capacity of the latter [6]. Impaired implantation is determined by regenerative plastic uterine mucosal failure that has been recently called endometriopathy [7, 8].
The possibilities of noninvasive evaluation of endometrial properties are still limited today.
Today, monitoring of endometrial blood flow assessment has been introduced into clinical work according to the data of not only two-dimensional seroscale echography, but also to those of volumetric energy Doppler [9]. Novel technologies, such as three-dimensional imaging, estimation of the volume of the endometrium and its vascularization in the VOCAL application enable the echographic signs of endometrial competence to be analyzed from other positions.
Objective: to determine management tactics for patients with the diffuse and nodular forms of adenomyosis, by assessing the functional state of the endometrium.
Materials and methods
The presented investigation is a promising clinical study involving 104 patients of fertile age with the diffuse and nodular forms of adenomyosis.
All the examinees were given written and oral information about study methods. The patients gave their consent to participation in the investigation, the protocol of which had been approved by the Ethics Committee, N.N. Pirogov Russian National Research Medical University.
The inclusion criteria were a reproductive age of 19 to 42 years, the presence of echographically confirmed adenomyosis, no use of hormonal agents and intrauterine contraceptive use for 6 months before the investigation, a body mass index of 18.5–30 kg/m2.
The exclusion criteria were patients with uterine malformations, uterine fibroids, those with inflammatory diseases of the uterus, appendages, with malignant tumors, endocrine diseases, lactation, pregnancy.
The functional competence of the mucous uterine layer was evaluated according to the following ultrasound criteria: the thickness of the endometrium (М echo), M echo genicity; identification of the unevenness of closure of anterior and posterior uterine walls; the presence of inclusions of different ultrasound densities in the projection of the basal endometrial layer. Focal and diffuse alteration of the subendometrial area of the mucous uterine layer has been worthy of notice.
Color Doppler scanning estimated intra-organ blood flow; attention was paid to the analysis of the intensity of hemodynamics, the distribution of perfusion loci, and to the numerical ssessment of blood flow (pulsatility index (PI), resistive index (RI), and systolic-diastolic (S/D) ratio in the terminal branches of uterine vessels, radial, basal, and spiral arteries.
The endometrial borders from the inner ostium uteri to the uterine fundus were manually outlined with rotation through the saggital section at a step of 9 degrees; the line of demarcation was myo-endometrial junction. The findings from three-dimensional energy Doppler imaging were used to automatically calculate quantitative parameters as histograms reflecting the indices of volumetric blood flow in the endometrial and subendometrial (mode SHELL, by trimming along the external contour at 5 mm) areas.
The blood flow indices: the vascilarization index (VI-%) given in percentages measures the number of color voxels in the examined volume, by presenting tissue blood vessels. The flow index (FI) is the mean of color of all color voxels, which shows the mean intensity of color. The vascular flow index (VFI) is the mean color of all gray color voxels, which reflects the combined presentation of flow vascularization and intensity.
Statistical analysis
The findings were statistically analyzed using the IBM SPSS programs version 23.0.0.0 and Microsoft Excel 2016.
The following study methods were used:
1. Descriptive statistics. The quantitative values of compared groups are presented as the mean (standard deviation in the normal distribution of the findings) – M (SD), the median and и the lower and upper quartiles in the abnormal distribution of data Ме (Q1; Q3). The qualitative characteristics are given as the frequency of absolute n, relative to n/N and a percentage share.
2. Checking the compliance of data distribution to the normal distribution, by using the Kolmogorov–Smirnov single-selection criterion.
3. Analyzing differences in two independent groups, by using Student’s T test (ST) in the normal data distribution or the nonparametric Mann–Whitney U test in the abnormal distribution.
4. Analyzing differences in three groups, by using the nonparametrc Kruskel–Wallis (W) criterion.
5. Differences between the qualitative signs, by using the nonparametric χ2 criterion.
6. A relationship between the quantitative signs, by using the Spearman’s rank correlation coefficient.
7. The critical value of the significance level was taken equal to 5% (p≤0.05).
Results and discussion
The patients’ age varied 18 to 42 years. The mean age of patients with the diffuse form of adenomyosis was significantly younger (31.8 (2.6) years) than the mean age of those with the nodular form (33.1 (1.9) years (ST=2.45; p=0.02<0.05). The body mass index differed (U=986; p=0.023<0.05), being the median of 20.6 (19.39; 21.703) kg/m2 for the diffuse form of adenomyosis and 21.2 (20.52; 22.14) kg/m2 for the nodular form.
The main menstrual dysfunction in every three observed women was prolongation of their menstrual cycle up to 41 days. The changes in the cohort of the examinees do not depend on the form of endometriosis of the corpus uteri.
The incidence of primary and secondary infertility in Group 2 patients (with the nodular form of adenomyosis) was 1.5 and 1.8 times higher than in Group 1 patients (with the diffuse form of adenomyosis, making up 5/46 (10.9%) and 9/46 (19.6%) examinees, respectively; in the nodular form group and 4/58 (6.9%) and 6/58 (10.3%) in the diffuse form group. Nevertheless, there were no significant differences between the incidence of primary and secondary infertility in patients with diffuse and nodular forms (χ2=2.561; p=0.278>005).
The duration of infertility varied 1 to 7 years. The median duration of infertility in the examinees from Group 2 was 6 (5;7) years; was significantly longer (U=191; p<0.001); the mean duration of infertility in the examinees with the diffuse form was 3 (1;3) years.
The incidence of extragenital disease did not statistically differ in the diffuse form (20/58 (34.5%) and nodular form 16/46 (34.78%) groups (χ2=0.001; p=0975>0.05).
The thickness of M echo and the ultrasound pattern are known to be one of the criteria for endometrial susceptibility [10, 11]. Our previous studies have introduced the differentiation of the endometrium into the moderately thin one (the thickness varies 6.0 to 8.0 mm) and the extremally thin one (3.0–5.9 мм). In this investigation, for the sake of perception and understanding the degree of incompetence of the mucous uterine layer, we were guided by the above gradation in the similar fashion [12].
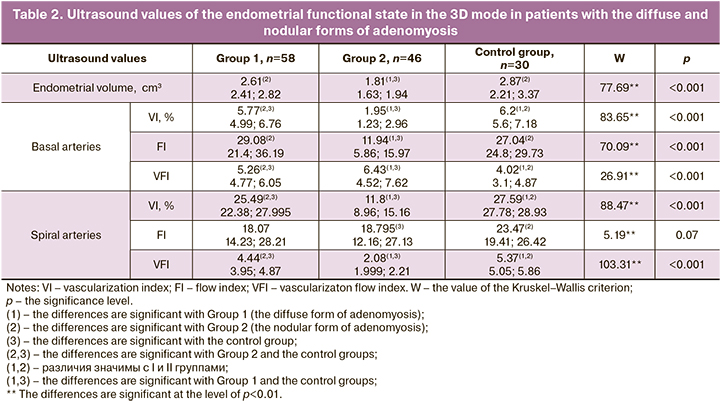
Due to the inconsistency of distribution of the examined variables to the normal distribution to compare the ultrasound endometrial susceptibility values obtained from two- and three-dimensional modes in patients with the diffuse and nodular forms of adenomyosis, as a well as in the comparison group, the Kruskel–Wallis criterion was used The results are given in Tables 1 and 2.
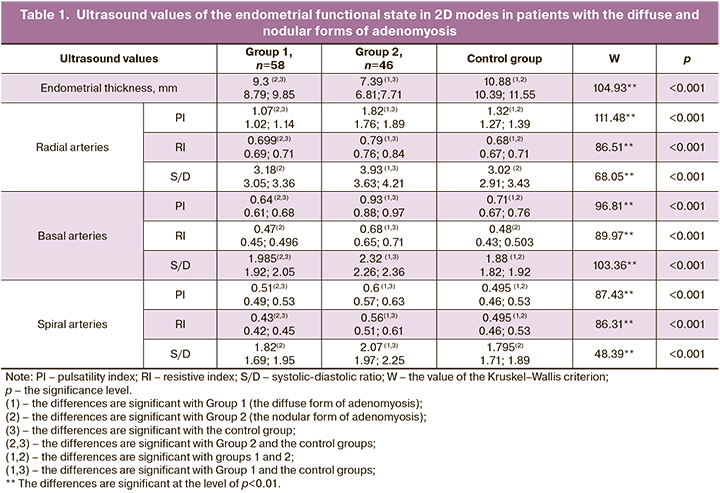
Ultrasound screening in Phase 2 of the cycle in the examinees of Group 1 (the diffuse form) recorded an endometrial thickness of 9.3 (8.79; 9.85) mm that correlated with the average population values and ranged 7.0–14.0 мм. Being consistent with the middle secretion phase, the endometrium had a higher echogenicity and a dropped shape narrowing down to the cervical canal. The hyperechogenic line of closure of the anterior and posterior endometrial folium assumed an interrupted appearance.
19/58 (32.8%) patients with the diffuse form were observed to have a poor ultrasound pattern: a moderately thin endometrium was visualized according to the mean values of 6.4 (0.9) mm. Asynchronicity of endometrial transformation was recorded since the day of the cycle, which was characterized by a clear-cut thin hyperechoic stripe in the center of the middle-line reflection, as well as by the enhanced reflection at the boundary of the mucous and muscular layers. The endometrial echographic pattern was noted for delayed development and/or insufficient transformation of the functional endometrial layer.
The ultrasound pattern of the uterine mucosa was seen as an interrupted line between the anterior and posterior follums in every three examined women with the moderately thin endometrium with the diffuse form of adenomyosis. The cambial nonrejectable layer displayed inclusions of both increased and reduced echogenicity, which frequently characterizes impairments in the nidational potential of the endometrium [13].
The personalized assessment could reveal that 12/19 (63.16%) patients with the moderately thin endometrium had a history of non-developing pregnancy; 7/19 (36/84%) patients with the moderately thin endometrium underwent hysteroscopy, separate diagnostic curettage in patients with the moderately thin endometrium; the history had evidence for curettage for abnormal uterine bleeding; morpholopathological study verified simple glandular hyperplasia.
The examinees with the extremely thin endometrium in the group under discussion were not identified.
At the present state of the art, the nidational potential of the endometrium is estimated in terms of the perfusion values of the terminal arteries in the uterine arterial bed [14]. The terminal branches of blood flow were identified in the overwhelming number of patients: the radial arteries were recorded in each examinee; the basal arteries were located in 49/58 (84.5%) patients; the spiral arteries were in 27/58 (46.5%) patients. Endometrial and subendometrial perfusion was absent in 9/58 (15.5%) patients; the history of these patients had evidence for old reproductive age and intrauterine interventions.
The qualitative assessment of endometrial blood flow perfusion indices can predict the functional competence of the glandular uterine layer. We identify the high impedance of angle-independent indices of blood flow velocity curves of endometrial perfusion, being the median for radial arteries: Me RI=0.699 (0.69; 0.71); Me S/D=3.18 (3.05; 3.36); for basal arteries: Me IR=0,47 (0.45; 0.496); Me S/D=1.985 (1.92; 2.05); for the spiral ones: Me IR=0,43 (0.42; 0.45); Me S/D=1,82 (1.69; 1.95).
The echographic screening of the examinees in Group 2 (the nodular form) revealed that the endometrial thickness in only 8/46 (17.4%) patients ranged from 8.9 to 11,6 mm, which corresponded to the values in the control group.
The endometrial echogenic interface in the majority of the observed patients (28/46 (60.8%) had not structural properties; the thickness averaged 7.39 (6.81;7.71) mm, which was regarded by us as the moderately thin endometrium. The pattern was characterized by a low homogeneous echogenicity. The contact of the mucosal membranes of the anterior and posterior walls was seen as a well-defined hyperechogenic stripe.
10/46 (21.7%) patients were noted to have an extremal endometrial thinning, which did not correspond to the phase of the menstrual cycle. M echo was in the range of 3.4–5.7 mm to 4.7 (0.8) mm. This echographic structure should be attributed to the hypoplastic endometriopaties that reduce the endometrial capability for the ovum nidation. [13]. These patents were observed to have ultrasound signs of chronic endometritis, which was manifested by the unevenness and interruption of the external endometrial contour, by the presence of anechogenic cystic inclusions up to 2–3 mm.
7/10 (70%) examinees with the extremally thinned endometrium were recorded to have an echo pattern of fibrosis and calcinosis in the endo-myometrial area, which is characterized by hyperechogenic areas with an acoustic effect. (The medical history of the above patients had evidence for undergone intrauterine interventions (tooling removal of the remnants of the fetal egg, curettage of the uterine mucosa).
The blood flow loci in the projection of radial arteries were identified in all the examinees from Group 2 (the nodular form of adenomyosis). Comparison of both qualitative and quantitative hemodynamic parameters in the radial arteries between the examined groups revealed no significant difference, which indicates that the analysis of perfusion in the vessels of this size is of low informative value and unreasonable.
Power Doppler imaging detected blood flow in the basal and spiral arteries in 24/46 (52.2%) and in 10/46 (21.77%) patients, respectively. 12/46 (26.1%) patients were not recorded blood flow areas in the terminal branches of the terminal branches of the uterine arteries. The thickness of the M-echo did not exceed 6.5 mm; that averaged 4.3 (0.8 mm). The uneven distribution of perfusion loci in the projection of spiral arteries engaged attention during the qualitative assessment of the intensity and symmetry of perfusion. This deterioration of the qualitative characteristics of blood flow during CDM can be explained by the decreased endometrial blood supply, which can reduce the rate of pregnancy and its carrying with a favorable outcome.
Ultrasound study with CDM in the basal and spiral arteries in the middle secretion phase showed a 1.2-1.4-fold increase in RI and S/D in every two patients (24/46 ((52.2%) with the nodular form compared to a group of patients with the diffuse form of endometriosis if the corpus uteri. The Me RI=0.68 (0.65; 0/71); the Me S/D=2.32 (2.26; 2.36) for the basal arteries. The perfusion values of the spiral arteries corresponded: Me RI=0.56 (0.51; 0.61); Me S/D=2.07 (1.97; 2/25).
According to the results obtained using three-dimensional ultrasound scanning, the examined groups were found to have significant differences in the functional competence of the uterine mucosa. We consider it important to note that the intergroup pairwise comparison using the Mann-Whitney U test recorded statistically significant endometrial volume differences in patients with the nodular and diffuse form (U=13; p<0.001). The volume of the uterine functional layer in Group 2 was 1.81 (1.63; 1.94) cm3 was significantly lower than that in the examinees in Group 1 (2.61 (2.41; 2.82); moreover, the marked value in Group 1 did not significantly with the data in the control group (U=688; p=0.11>0.05).
We recorded significant differences in the characteristics of blood flow in the endometrial and subendometrial areas in patients with the diffuse and nodular forms of adenomyosis. The described disorders can be associated with the incompetent nidational potential of the uterine mucosa.
The Spearman’s rank correlation coefficient was used to check the association of the values of the functional state of the urine mucosa in the 2D and 3D modes. The data are given in Table 3.
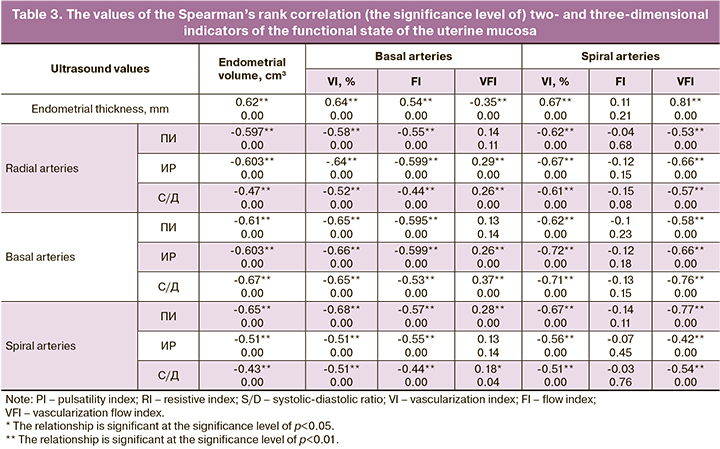
The sonographic indicators of the functional incompetence of the uterine mucosa are closely related to the hypovascularization of endometrial and subendometrial areas. It is also worth noting that the volume of the uterine mucosa has a negative inverse relationship to PI, RI, and S/D in the radical, basal, and spiral arteries.
The flow index in the basal arteries is correlated with the endometrial thickness (R = 0.54; p<0.001). There is no correlation of the flow index in the spiral arteries with the endometrial thickness (R=0.11; p=0.21>0.05).
The increase in IR and its monotonicity during the secretory phase, the higher S/D ratio in the terminal branches of the uterine arterial bed should be interpreted as impaired endometrial susceptibility. The decrease in perfusion in the terminal branches of the uterine arterial bed. The decrease in the perfusion in the terminal branches of the uterine arteries or the absence of perfusion is due to the impaired endometrial angiogenesis and is associated with alteration of the endomyometrial transitional area as a result of invasive endometrial processes. Hypovascularization could be due to morphological impairments in neoangiogenesis, which are typical for adenomyosis.
The vessels in endometroid heterotopies are known to be presented by muscle-type arteries, the bulk of which is sclerotic [10]. Arterial vessel narrowing and obliteration that are accompanied due to connective tissue proliferation by dystrophic and sclerotic changes in the vascular wall are characterized by higher vascular resistance and tissue ischemia.
Consequently, adenomyosis affects the functional state of the uterine mucosa, which may be one of the factors for endometriosis-associated infertility. The involvement of the endometrium into the pathogenetic mechanisms of infertility in endometriosis manifest itself as worse blood flow values in the uterine mucosa.
Conclusion
Thus, the pronounced decline in the endometrial thickness, which is particular in the nodular form of adenomyosis, is associated with the high index in the terminal vessels of the uterine arteries, which is manifested itself as the impaired competence of the endometrial state, which is accompanied by a decrease in the implantation potential. This cohort of patients should be recommended to have a reproductologist’s consultation to decide whether assisted reproductive technologies should be used.
Three-dimensional echography with power Doppler function is an additional method to estimate the volume of the endometrium and volumetric blood flow at the level of basal and spiral arteries.
The complex analysis of predictors for impaired endometrial receptivity enhances the effectiveness of assessing the functional compliance of the endometrium in reproductive-aged patients with adenomyosis. Three-dimensional echography is innovative, which means that the novel method that necessitates additional development of criteria for evaluation of endometriopathies.
References
- Chapron C., Marcellin L., Borghese B., Santulli P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat. Rev. Endocrinol. 2019; 15(11): 666-82. https://dx.doi.org/10.1038/s41574-019-0245-z.
- Chapron C., Vannuccini S., Santulli P., Abrão M.S., Carmona F., Fraser I.S. et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum. Reprod. Update. 2020; 26(3): 392-411. https://dx.doi.org/10.1093/humupd/dmz049.
- Джамалутдинова К.М., Козаченко И.Ф., Щеголев А.И., Файзуллина Н.М., Адамян Л.В. Клинико-морфологические особенности узлового и диффузного аденомиоза. Акушерство и гинекология. 2017; 9: 86-94. [Dzhamalutdinova K.M., Kozachenko I.F., Shchegolev A.I., Fayzullina N.M., Adamyan L.V. Clinical and morphological features of nodular and diffuse forms of adenomyosis. Obstetrics and Gynecology. 2017; (9): 86-94. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.9.86-94.
- Шкляр А.А., Адамян Л.В., Коган Е.А., Парамонова Н.Б., Козаченко И.Ф.,Гаврилова Т.Ю., Кононов С.Н. Трудности диагностики узловой и диффузной форм аденомиоза. Акушерство и гинекология. 2015; 3: 69-72. [Shklyar A.A., Adamyan L.V., Kogan E.A., Paramonova N.B., Kozachenko I.F., Gavrilova T.Yu., Kononov S.N. Difficulties in diagnosing nodular and diffuse adenomyosis. Obstetrics and Gynecology. 2015; (3): 69-72.(in Russian)].
- Шкляр А.А., Адамян Л.В., Коган Е.А., Парамонова Н.Б., Козаченко И.Ф., Гаврилова Т.Ю. Клинико-морфологические особенности диффузной и узловой форм аденомиоза. Проблемы репродукции. 2015; 21(1): 74‑9. [Shklyar A.A., Adamyan L.V., Kogan E.A., Paramonova N.B., Kozachenko I.F., Gavrilova T.Yu. The clinical and morphological features of nodular and diffuse forms of adenomyosis. Russian Journal of Human Reproduction. 2015; 21(1): 74‑9. (in Russian)]. https://dx.doi.org/10.17116/repro20152174-79.
- Alcalde A.M., Martínez-Zamora M.Á., Gracia M., Ros C., Rius M.,Carmona F. Assessment of quality of sexual life in women with adenomyosis. Women Health. 2021; 61(1): 520-6. https://dx.doi.org/10.1080/03630242.2021.1920557.
- Коган Е.А., Калинина Е.А., Колотовкина А.В., Файзуллина Н.М., Адамян Л.В. Морфологический и молекулярный субстрат нарушения рецептивности эндометрия у бесплодных пациенток с наружно-генитальным эндометриозом. Акушерство и гинекология. 2014; 8: 47-52. [Kogan E.A., Kalinina E.A., Kolotovkina A.V., Faizullina N.M., Adamyan L.V. The morphological and molecular substrate of impaired endometrial receptivity in infertile patients with external genital endometriosis. Obstetrics and Gynecology. 2014; (8): 47-52. (in Russian)].
- Кузнецова М.В., Пшеничнюк Е.Ю., Бурменская О.В., Асатурова А.В., Трофимов Д.Ю., Адамян Л.В. Исследование экспрессии генов в эутопическом эндометрии женщин с эндометриоидными кистами яичников. Акушерство и гинекология. 2017; 8: 93-102. [Kuznetsova M.V., Pshenichnyuk E.Yu., Burmenskaya O.V., Asaturova A.V., Trofimov D.Yu., Adamyan L.V. Study of gene expression in the eutopic endometrium of women with endometrioid ovarian cysts. Obstetrics and Gynecology. 2017; (8): 93-102. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.8.93-102.
- Alcazar J.L. Three-dimensional ultrasound assessment of endometrial receptivity: a review. Reprod. Biol. Endocrinol. 2006; 4: 56.https://dx.doi.org/10.1186/1477-7827-4-56.
- Руденко Ю.А., Кулагина Е.В., Кравцова О.А., Целкович Л.С., Балтер Р.Б., Ибрагимова А.Р., Иванова Т.В., Ильченко О.А., Тюмина О.В., Рябов Е.Ю. Готовность эндометрия к экстракорпоральному оплодотворению: прогноз по данным ультразвукового и морфологического исследования. Гены и клетки. 2019; 14(3): 142-6. [Rudenko Yu.A., Kulagina E.V., Kravtsova O.A., Tselkovich L.S., Balter R.B., Ibragimova A.R., Ivanova T.V., Ilchenko O.A., Tyumina O.V., Ryabov E.Yu. The readiness of the endometrium for extracorporeal fertilization: prognosis by the data of ultrasound and morphological study. Genes and Cells. 2019; 14(3): 142-6. (in Russian)].https://dx.doi.org/10.23868/201906025.
- Park H., Lee H.J., Kim H.G., Ro Y.M., Shin D., Lee S.R., Kim S.H., Kong M. Endometrium segmentation on transvaginal ultrasound image using key-point discriminator. Med. Phys. 2019; 46(9): 3974-84. https://dx.doi.org/1010.1002/mp.13677.
- Соломатина А.А., Михалева Л.М., Хамзин И.З., Братчикова О.В., Тюменцева М.Ю., Чабиева Л.Б., Кочеткова А.М., Хованская Т.Н. Овариальный резерв и имплантационные свойства эндометрия у пациенток после органосберегающих операций по поводу эндометриоидных образований яичников. Вопросы гинекологии, акушерства и перинатологии. 2021; 20(1): 64-70. [Solomatina A.A., Mikhaleva L.M., Khamzin I.Z., Bratchikova O.V., Tyumentseva M.Yu., Chabieva L.B., Kochetkova A.M., Khovanskaya T.N. Ovarian reserve and endometrial reseptivity in patients after organ-sparing surgeries for ovarian endometriotic cycts. Gynecology, Obstetrics and Perinatology. 2021; 20(1): 64-70. (in Russian)]. https://dx.doi.org/1010.20953/1726-1678-2021-1-64-70.
- Буланов М.Н. Ультразвуковая гинекология. Курс лекций в 2 частях. 4 изд. М.: Видар-М; 2017. [Bulanov M.N. Ultrasound gynecology. Course of lectures in 2 parts. 4th ed. Moscow: Vidar-M; 2017. (in Russian)].
- Краснопольская К.В., Назаренко Т.А., Ершова И.Ю. Современные подходы к оценке рецептивности эндометрия (обзор литературы). Проблемы репродукции. 2016; 22(5): 61-9. [Krasnopolskaya K.V., Nazarenko T.A., Ershova I.Yu. Modern approaches to endometrial receptivity assessment (a review). Russian Journal of Human Reproduction. 2016; 22(5): 61 9.(in Russian)]. https://dx.doi.org/10.17116/repro201622561-69.
Received 14.11.2022
Accepted 21.03.2023
About the Authors
Antonina A. Solomatina, Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia, +7(495)432-09-89, 9200690@mail.ru, https://orcid.org/0000-0002-3802-7343, eLibrary SPIN: 7681-9893;RSCI ID (Author ID): 524620, 1 Ostrovityanov str., Moscow, 117997, Russia.
Parvana D. Ismaiilova, PhD student, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University,
Ministry of Health of Russia, +7(909)683-98-89, velieva.95@mail.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Larisa E. Breusenko, PhD, Senior Reseacher, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University,
Ministry of Health of Russia, +7(985)998-87-08, 9988708@mail.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Sergey V. Shtyrov , Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University,
Ministry of Health of Russia, +7(985)763-01-22, 7630122@mail.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Marina Yu. Tyumentseva, PhD, Senior Researcher, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia, +7(916)196-54-71, andtium@yandex.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Svetlana V. Regul, PhD student, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health
of Russia, +7(915)157-57-33, reggyn@bk.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Zarema Z. Khalifaeva, PhD student, Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University,
Ministry of Health of Russia, +7(963)999-76-66, khalifaeva29@mail.ru, 1 Ostrovityanov str., Moscow, 117997, Russia.
Corresponding author: Parvana D. Ismaiilova, velieva.95@mail.ru