Анемия в структуре экстрагенитальных заболеваний беременных занимает ведущее место и представляет собой одну из наиболее актуальных проблем в акушерстве и перинатологии [1]. По данным Всемирной организации здравоохранения, более 40% беременных женщин в мире имеют анемию [2]. Данные статистики свидетельствуют о том, что при длительном течении анемии чаще развивается плацентарная недостаточность. У 40–50% женщин имеет место риск развития преэклампсии; преждевременные роды наступают у 11–42%, слабость родовой деятельности отмечается у 10–15%, гипотонические кровотечения в родах возникают у 10% рожениц, послеродовой период осложняется гнойно-септическими заболеваниями у 12% и гипогалактией – у 38% родильниц [3].
По данным исследования M. Nair et al. [4], была показана взаимосвязь между уровнем гемоглобина у беременных и повышением риска мертворождения. Так, риск мертворождения/перинатальной гибели повышался в 5 раз при уровне гемоглобина менее 100 г/л у беременных при первом антенатальном визите и в 3 раза – при выявлении анемии у женщин в 28 недель беременности по сравнению с беременными с нормальным уровнем гемоглобина [4].
Проведены многочисленные исследования, в которых изучалось влияние уровня гемоглобина у женщин во время беременности на состояние их новорожденных детей [5–11]. Среди детей, родившихся у женщин с анемией, часто встречаются такие осложнения, как признаки внутриутробного инфицирования, асфиксия различной степени тяжести. В ряде исследований было продемонстрировано, что среди женщин с наличием анемии во время беременности был повышен риск преждевременных родов, рождения детей с задержкой физического развития и отмечалось повышение показателя неонатальной смертности [7, 8, 12–17]. Были получены статистически значимые корреляции низкого уровня гемоглобина в I триместре беременности и повышения риска рождения детей с низкой массой тела. В то же время есть исследования, где не выявлено статистически значимой связи уровня гемоглобина у женщин во время беременности, преждевременных родов и различных рисков со стороны новорожденных [18–20]. В исследовании Е. Willner et al. [21] не было выявлено статистически значимых отличий массы, длины тела и окружности головы при рождении среди детей, рожденных женщинами с анемиями различной степени тяжести и без анемии во время беременности. Также не было выявлено статистически значимых изменений уровня гемоглобина и гематокрита у этих новорожденных. Данные исследования включали женщин и их новорожденных детей при доношенных сроках беременности.
Противоречивые результаты в приведенных исследованиях могут быть связаны с тем, что определение уровня гемоглобина проводилось в разных триместрах беременности. В большинстве исследований оценивался уровень гемоглобина в I и III триместрах беременности. В ряде исследований и вовсе не указывалось время определения уровня гемоглобина. Неоднозначные результаты в исследованиях могут быть связаны с отсутствием данных о проводимой противоанемической профилактике и терапии у женщин c демографическими и социальными аспектами.
Подавляющее большинство исследований включало наблюдение за беременными женщинами и их новорожденными при доношенном сроке гестации.
Цель исследования – оценить влияние наличия анемии во время беременности на состояние здоровья недоношенных новорожденных с очень низкой и экстремально низкой массой тела (ОНМТ и ЭНМТ) при рождении.
Материалы и методы
Было проведено одномоментное сравнительное исследование на базе ФГБУ «НМИЦ АГиП им. В.И. Кулакова» Минздрава России в период с января 2017 по ноябрь 2018 г.
Критерии включения: все дети с ОНМТ и ЭНМТ, рожденные за этот период времени, и их матери, наблюдаемые в ФГБУ «НМИЦ АГиП им. В.И. Кулакова» Минздрава России; наличие информированного согласия пациенток.
Критерии исключения: дети с множественными пороками развития, критическими врожденными пороками сердца, хромосомной патологией, метаболическими заболеваниями, гемолитической болезнью новорожденных, многоплодные беременности.
В исследование были включены 105 женщин и их недоношенных новорожденных с ОНМТ и ЭНМТ. У 38 (36%) женщин отмечалась анемия во время беременности, у 67 (64%) анемии во время беременности не было.
По критериям Всемирной организации здравоохранения, у женщин диагноз анемии легкой степени выставлялся при уровне гемоглобина 90–109 г/л, умеренной анемии, или анемии средней тяжести, – при гемоглобине 70–89 г/л и тяжелой анемии – при гемоглобине менее 70 г/л [22].
Согласно данным критериям, среди женщин с наличием анемии во время беременности, родивших детей с ОНМТ и ЭНМТ (n=38), у 28 (74%) отмечалась анемия легкой степени, у 10 (26%) – анемия средней степени тяжести, тяжелой анемии не отмечалось.
Все новорожденные дети (n=105) были разделены на 2 группы в зависимости от наличия или отсутствия у их матерей анемии во время беременности: 1-я группа – дети с ОНМТ и ЭНМТ, родившиеся у женщин, у которых во время беременности перед родоразрешением отмечалась анемия различной степени тяжести (n=38); 2-я группа – дети с ОНМТ и ЭНМТ, родившиеся у женщин с отсутствием анемии во время беременности (n=67).
У всех недоношенных отмечались дыхательные расстройства при рождении, в связи с чем они были переведены из родильного блока в отделение реанимации и интенсивной терапии (ОРИТ), где им проводили лечение и обследование по общепринятым стандартам в соответствии с клиническими рекомендациями [23].
Был проведен анализ, который включал течение беременности, срок родоразрешения – гестационный возраст (ГВ), частоту летальных исходов – количество детей, умерших в течение неонатального периода, антропометрические данные и состояние детей при рождении, динамику и объем проводимого лечения. Оценка показателей физического развития новорожденных проводилась в соответствии с критериями Всемирной организации здравоохранения [24]. Критерием задержки развития являлось снижение массо-ростовых показателей, входящее в интервал ниже 10 перцентилей для соответствующего ГВ с учетом гендерного признака.
Статистическая обработка данных выполнена с помощью программы SPSS v.17.0. Для каждого количественного параметра были определены медиана (Ме), значения 25 и 75 квартилей (Q1;Q3). Для качественных данных определяли показатели частоты (%). При проведении сравнительного анализа количественных данных в исследуемых группах применялись методы непараметрической статистики – U-критерий Манна–Уитни для двух групп; при анализе номинальных переменных – χ2 Пирсона (ожидаемое явление >10), χ2 Пирсона с поправкой Йейтса (ожидаемое явление >5, но <10), точный критерий Фишера (ожидаемое явление <5). Статистически значимыми считались различия при р<0,05. Для оценки влияния факторов риска было рассчитано отношение шансов (ОШ). Значение ОШ приводилось с 95% доверительным интервалом (ДИ).
Результаты и обсуждение
По данным исследования, в материнском анамнезе недоношенных новорожденных с ОНМТ и ЭНМТ анемия во время беременности отмечалась в 38 (36%) случаях. Благодаря комплексным профилактическим и лечебным мероприятиям при ведении беременностей, в подавляющем большинстве случаев регистрировалась анемия легкой степени тяжести – 28 (74%) женщин, у 10 (26%) женщин – анемия средней степени тяжести, тяжелой анемии не отмечалось.
При проведении исследования не было выявлено статистически значимых отличий в паритете. В 1-й группе детей в материнском анамнезе отмечалась преэклампсия – в 5,3%, во 2-й – в 1,5%, истмико-цервикальная недостаточность в 1-й группе – в 2,6%, во 2-й – в 4,4% (p>0,05). В обеих группах с одинаковой частотой проводилась антенатальная профилактика респираторного дистресс-синдрома. Все родоразрешения были произведены в сроке 28–32 недель. Путем операции кесарева сечения в 1-й группе были родоразрешены 34 (89,5%) беременные, во 2-й – 62 (92,5%) беременные. В 1-й и 2-й группах после рождения всем детям проводилось «сцеживание» пуповины.
Родились 105 недоношенных детей: с ОНМТ – 61 ребенок, с ЭНМТ – 44.
Между исследуемыми группами были выявлены статистические различия в сроке гестации (р=0,004; табл. 1). Статистических различий массы и длины тела при рождении, оценки по шкале Апгар на 1-й и 5-й минутах жизни между группами получено не было (см. табл. 1). Частота летальных исходов в 1-й группе была выше, чем во 2-й, однако статистически достоверных различий не получено, р=0,093. В 1-й группе умерли 5 (13,2%) детей (4 – с ЭНМТ и 1 – с ОНМТ), во 2-й – 7 (10,4%) детей (5– с ЭНМТ и 2 – с ОНМТ).

При проведении анализа старта респираторной терапии в 1-й час жизни, общей длительности респираторной терапии (инвазивная и/или неинвазивная), общего количества гемотрансфузий эритроцитсодержащих компонентов крови, свежезамороженной плазмы, тромбоконцентрата, проводимых в период госпитализации, длительности лечения в ОРИТ у детей с ОНМТ и ЭНМТ из 1-й и 2-й групп статистически значимой разницы получено не было (табл. 2). Частота ранних гемотрансфузий эритроцитсодержащих компонентов крови (в 1-ю неделю жизни) была достоверно выше в 1-й группе детей, р=0,01. Шансы проведения гемотрансфузии на 1-й неделе жизни среди глубоконедоношенных детей с ОНМТ и ЭНМТ в 1-й группе были выше в 3,8 раза (95% ДИ 1,2–12,5) по сравнению со 2-й группой.
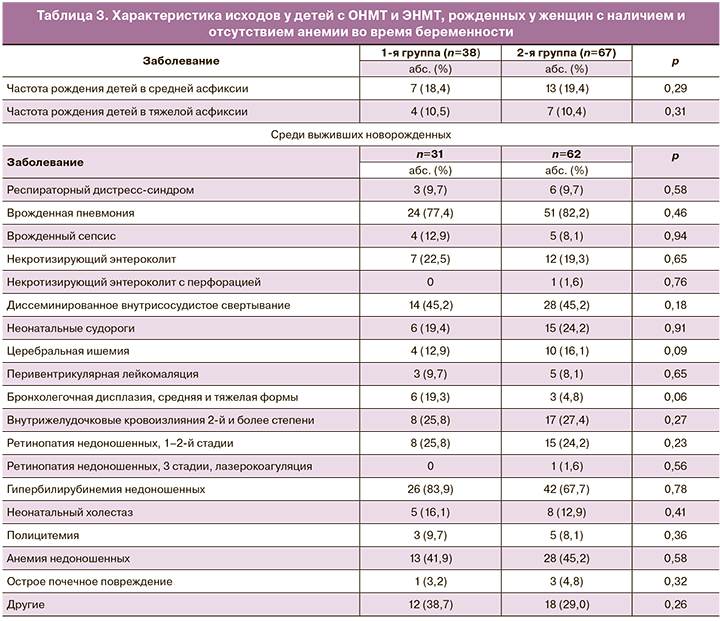
Среди выживших новорожденных с ОНМТ и ЭНМТ относительная частота бронхолегочной дисплазии была выше в 1-й группе по сравнению со 2-й, и отмечалась тенденция к статистической значимости, р=0,06 (табл. 3), что может быть связано с более частыми ранними гемотрансфузиями эритроцитсодержащих компонентов крови (в 1-ю неделю жизни) среди детей 1-й группы. Достоверных отличий при сравнении таких исходов, как наличие врожденной инфекции, внутрижелудочковых кровоизлияний, перивентрикулярной лейкомаляции, ретинопатии недоношенных и других заболеваний, между 1-й и 2-й группами выявлено не было (см. табл. 3).
Представленные данные свидетельствуют о том, что наличие анемии во время беременности у женщин, родивших детей с ОНМТ и ЭНМТ, ассоциировано с меньшим гестационным возрастом и особенностями течения неонатального периода. Глубоконедоношенным детям, которые родились у женщин с наличием анемии во время беременности, чаще проводились ранние гемотрансфузии, т.е. трансфузии эритроцитсодержащих компонентов крови в 1-ю неделю жизни, с чем может быть связана большая частота бронхолегочных дисплазий у данной группы детей.
В проводимом нами исследовании не были оценены социальный статус беременных женщин, курение, особенности диеты женщин до и во время беременности.
Данное исследование – одно из немногочисленных исследований, в котором проведена оценка влияния анемии во время беременности у женщин на состояние здоровья их новорожденных детей с ОНМТ и ЭНМТ.
Железодефицитная анемия – наиболее частая причина анемии у беременных. Всемирная организация здравоохранения рекомендует профилактическое назначение железа и фолиевой кислоты в течение беременности [21]. По данным базы Кохрейн, дотация железа во время беременности снижает риск развития железодефицитной анемии, однако влияние приема препаратов железа во время беременности на материнские исходы и исходы у их новорожденных детей требует дальнейшего изучения [25]. При низком уровне гемоглобина во время беременности снижается эффективность транспорта кислорода через плаценту к плоду. Анемия во время беременности может быть индикатором непосредственно нутритивного дефицита у женщины, который ранее, до беременности, не был выявлен.
В крупном метаанализе, проведенном В.А. Haider et al. [26], демонстрируется, что ежедневный прием препаратов железа во время беременности снижает риск рождения детей с малой массой тела. Увеличение уровня гемоглобина во время беременности приводит к увеличению массы тела ребенка к моменту рождения. Так, при доношенных сроках при увеличении уровня гемоглобина у женщины во время беременности на 1 г/л увеличивается масса тела плода в среднем на 14 г (от 6,8 до 21,8) (р=0,002). Описанные исследования, подобные нашему, демонстрируют, что анемия у женщин во время беременности коррелирует с неонатальными исходами. Профилактика и лечение анемии как до наступления, так и во время беременности являются актуальными задачами в современном акушерстве и перинатологии. Правильная тактика ведения беременных женщин уменьшает вероятность неблагоприятного влияния анемии на состояние здоровья и прогноз новорожденных детей, в особенности недоношенных с ОНМТ и ЭНМТ. С целью профилактики преждевременных родов и улучшения неонатальных исходов необходимо проводить тщательный сбор анамнеза, оценку клинико-анамнестических и лабораторных данных с идентификацией группы высокого риска по развитию анемии у женщин с этапа постановки на учет по беременности в I триместре и с последующим проведением комплексных профилактических и лечебных противоанемических мероприятий.
Заключение
Полученные данные свидетельствуют о том, что у женщин, родивших детей до 32-й недели гестации с ОНМТ и ЭНМТ, анемия была диагностирована в 36%. Благодаря комплексным профилактическим и лечебным мероприятиям при ведении беременностей в подавляющем большинстве случаев регистрировалась анемия легкой степени тяжести. Наличие анемии во время беременности у женщин, родивших детей до 32-й недели гестации с ОНМТ и ЭНМТ, статистически достоверно ассоциировано с меньшим сроком гестации (на 1 неделю, по данным нашего исследования), а также с особенностями течения неонатального периода их недоношенных детей, в частности, с более частой потребностью в проведении ранних гемотрансфузий.



