В последние десятилетия значительно возросла частота выполнения кесарева сечения - по статистическим данным, приблизительно каждая четвертая женщина подвергается оперативному родоразрешению. В свою очередь, «эпидемия» [1] кесарева сечения обуславливает увеличение числа отдаленных осложнений после этой операции, одним из которых является формирование несостоятельного рубца на матке - тяжелых рубцовых изменений с резко выраженным истончением и углублением («нишей») миометрия. Нарушение репарации миометрия может возникнуть по многим причинам, связанным как с техническими особенностями операции, так и с особенностями женского организма. Многими авторами в качестве основных причин развития несостоятельности маточного рубца рассматриваются послеродовый эндометрит и внутриматочные вмешательства в течение года после кесарева сечения, которые могут приводить к возникновению локального эндометрита и непосредственно травмировать область послеоперационного шва [2-7].
Для оценки рубца на матке применяют трансвагинальное ультразвуковое исследование в сочетании с сонографией, гистероскопию, магнитнорезонансную томографию (МРТ). Ofili-Yebovi et al. предложили определять степень выраженности дефекта по соотношению толщины миометрия в области рубца и толщины прилежащего миометрия [8]. Соотношение менее 50% оценивали как выраженный рубцовый дефект. Osser et al. предложили считать рубец несостоятельным при толщине сохраненного миометрия менее 2,2 мм [9].
В настоящее время несостоятельным рубцом на матке считается дефект с истончением миометрия до 2-3 мм (или даже его полным отсутствием) и/ или наличием «ниши/ниш» со стороны полости матки. Дополнительными признаками несостоятельности рубца на матке считаются ослабление васкуляризации миометрия в зоне рубца при допплерометрии маточного кровотока и прерывистость контуров рубца с наличием в нем значительного количества гиперэхогенных включений (соединительной ткани) [10, 11]. В 2019 г. были опубликованы результаты консенсуса, согласно которому «нишу» в области рубца следует определять как углубление на месте после кесарева сечения не менее 2 мм [12].
Доказано, что дефекты в области рубца могут негативно влиять на менструальный цикл, вызывая длительные постменструальные кровяные выделения, приводить к болевому синдрому в виде диспареунии и дисменореи, способствовать нарушению имплантации эмбриона, увеличивая риск спонтанного прерывания беременности в случае имплантации эмбриона в области дефекта [13-22].
Самыми тяжелыми, жизнеугрожающими осложнениями при несостоятельном рубце являются разрыв матки во время беременности и родов, прикрепление и/или врастание плаценты в этой области. По ряду данных, разрыв матки во время беременности встречается в 1 случае из 280-12 000 родов [23, 24]; в развитых странах сообщается о 1,9-38 случаев разрыва матки на 10 000 родов [25]. Наличие рубца на матке является доказанным значимым фактором, повышающим риск разрыва матки во время беременности [26-28]. При анализе исходов 2 951 297 беременностей частота возникновения разрыва оперированной матки составила 0,07% против значительной меньшей частоты при отсутствии операций на матке - 0,012% [29, 30]. По данным различных систематических обзоров, частота разрыва матки по рубцу при последующей беременности варьирует от 0,8 до 2% [31-33]. Опубликованы результаты исследования, согласно которым наличие большого дефекта стенки миометрия (6 мм и более) и истончение стенки сохраненного миометрия менее 2,5 мм увеличивают риск расхождения краев рубца до 42,9% (p=0,47; отношение шансов 11,8%) [34].
Эффективным методом лечения данной патологии является выполнение реконструктивно-пластической операции - метропластики, которая подразумевает иссечение патологических тканей в зоне послеоперационного рубца после кесарева сечения и формирование нового полноценного шва. В настоящее время сформулированы четкие показания к реконструкции рубца на матке [10, 11]. При расположении несостоятельного рубца ниже внутреннего зева на 5 мм и более при отсутствии клинических симптомов выполнение метропласти- ки на этапе планирования беременности не показано даже при выраженном истончении миометрия. Абсолютным показанием к выполнению операции является наличие несостоятельного рубца на матке выше внутреннего зева у женщин, планирующих повторную беременность, и имплантация плодного яйца в области рубца во время предшествующей беременности, независимо от его расположения по отношению к внутреннему зеву. Также выполнение метропластики целесообразно при наличии клинических признаков «ниши» в области рубца, независимо от ее локализации по отношению к внутреннему зеву, значимо нарушающих качество жизни пациентки, - длительные сукровичные выделения из половых путей после менструации, межменструальные кровяные выделения, болевой синдром, диспареуния. Реконструктивная операция позволяет улучшить качество жизни пациентки, восстановить репродуктивную функцию и снизить риск жизнеугрожающих осложнений при беременности.
Хирургическая коррекция несостоятельного рубца на матке может быть выполнена абдоминальным, эндоскопическим (традиционный лапароскопическим, робот-ассистированным, гистероскопическим) или влагалищным доступами. В настоящее время активного развития эндоскопической хирургии все чаще предпочтения отдаются лапароскопическому или робот-ассистированному доступу.
Основной принцип абдоминальной, лапароско-пической, робот-ассистированной метропластики заключается в иссечении патологических тканей в зоне послеоперационного рубца с последующим формированием нового полноценного шва. Данная методика реконструкции наиболее распространена и признана в мировом сообществе [11, 35-38].
В некоторых публикациях описана лапароско-пическая реконструкция рубца на матке методом «шейвинга»: рубцовая ткань «сбривается» с миометрия без вскрытия полости матки [1]. По мнению авторов, полное иссечение рубца может способствовать увеличению натяжения между проксимальным и дистальным краями миометрия и ухудшить заживление вновь сформированного рубца. При оценке результатов после проведения «шейвинга» у большинства пациенток сохранялись выраженные рубцовые изменения миометрия (81,8%), однако все клинические симптомы были устранены у 63,6% пациенток. Наилучшие результаты были достигнуты в сокращении постменструальных кровяных выделений. Возможно, данная методика допустима у женщин, уже реализовавших репродуктивную функцию, для которых цель операции - улучшение клинической симптоматики.
В настоящее время большинство опубликованных работ представляет собой описание клинических наблюдений [36, 39, 40] или результатов лапа-роскопических метропластик у небольших групп пациенток (от 11 до 101) [1, 35, 37, 38, 41-43]. Наибольшие исследования по лапароскопической метропластике, которые мы встретили при литера-турном поиске, включают 104 пациентки [41], 63 пациентки [11] и 101 пациентку [43].
Робот-ассистированный доступ пока мало рас-пространен в реконструктивной хирургии матки. Возможно, это обусловлено достаточно редкой частотой несостоятельности рубца матки, аккуму-лированием пациенток с данной проблемой пре-имущественно в акушерско-гинекологических стационарах, достаточно высокой стоимостью роботи-ческих операций, ограниченными возможностями по оснащению лечебных учреждений роботическими установками, а также наиболее частым применением робототехники для лечения больных с онкоги- некологическими заболеваниями. Описаны клини-ческие наблюдения по роботическим метропласти- кам за последние 10 лет [44-48], а также результаты роботической метропластики у 10 пациенток [49]. Представленные данные сообщают об успешных результатах реконструкции рубца с использованием роботической техники, а также об улучшении качества этапов хирургического вмешательства. Wang H.F. et al. в 2021 г. опубликовали результаты успешной реконструкции рубца на матке роботическим (n=3) и лапароскопическим (n=17) доступами. Авторами приведены обобщенные результаты без сравнительной оценки лапароскопической и роботической метропластики: сообщается о статистически значимом уменьшении размеров «ниши» и увеличении остаточной толщины миометрия с 0,41±0,35 до 1,15±0,55 см через 9 месяцев, а также об улучшении клинической симптоматики [50].
Одним из возможных методов устранения кли-нических симптомов послеоперационной «ниши» является гистерорезектоскопия под контролем сонографии. Основными условиями для выполнения данной операции являются отсутствие планов реализации репродуктивной функции и наличие достаточной толщины сохраненного миометрия (не менее 3 мм) [51], что необходимо для снижения риска перфорации матки и травмы мочевого пузыря. Vervoort A. et al. в рандомизированном исследовании сообщают об улучшении клинической картины в виде сокращения постменструальных кровяных выделений и уменьшения болевого синдрома при резекции «ниши» с сохраненным миометрием >3 мм [52].
Клиническое наблюдение
Пациентка Ф., 36 лет, обратилась в ГБУЗ «Московский клинический научный центр им. А.С. Логинова» для хирургического лечения по поводу несостоятельности рубца на матке.
Из анамнеза известно, что у пациентки врожденная аномалия внутренних половых органов (полное удвоение матки), 3 беременности: в 2015 г. плановое кесарево сечение, две неразвивающиеся беременности. В послеоперационном периоде женщина отметила ухудшение состояния в виде увеличения продолжительности постменструальных кровяных выделений до 10—12 дней, общая продолжительность менструации до 15—16 дней. У пациентки диагностирована «ниша» в области послеопера-ционного рубца. В 2019 г. пациентке выполнена гистероскопическая коагуляция дефекта стенки матки, однако ожидаемого положительного эффекта достигнуто не было — сохранились жалобы на длительные, нарушающие качество жизни, пост-менструальные кровяные выделения. Пациентка планировала беременность, в связи с чем в 2020 г. повторно обратилась для комплексного обследования. Был диагностирован несостоятельный рубец после кесарева сечения в области перешейка левого тела матки: истончение миометрия до 2,5 мм с фор-мированием «ниши» размерами 10x8 мм (рис. 1).

Учитывая наличие несостоятельного рубца на матке, жалоб, значимо нарушающих качество жизни, неудачную попытку гистероскопической коррекции клинических симптомов в анамнезе у пациентки, планирующей реализацию репродуктивной функции, было решено выполнить реконструктивно-пластическую операцию — иссечение патологически измененных тканей в области перешейка левого тела матки с формированием нового рубца с использованием роботического комплекса DaVinci.
Хирургическое лечение проводилось под эндотра- хеальным наркозом. На первом этапе выполнена гистероскопия с визуальной оценкой размеров, глубины и расположения «ниши» по отношению к внутреннему зеву. С использованием комплекта оборудования KarlStorz произведен осмотр правой и левой полостей матки: область рубца визуализи-ровалась в левой полости матки сразу за внутренним зевом в виде «ниши» на всю ширину перешейка, глубиной более 5—7 мм (рис. 2).
Далее с использованием хирургического комплекса DaVinci была выполнена метропластика, основными задачами которой являлись максимально точное иссечение патологически измененного рубца на матке, минимизация травмы и адекватное сопоставление сохраненного миометрия с созданием условий для формирования полноценного послеоперационного рубца на матке.
Инициализация лапароскопии проведена с использованием иглы Вереша в надпупочной области на 5 см выше пупка. После наложения пневмо- перитонеума устанавливался оптический троакар 12 мм, 3 роботических манипулятора (троакары 8 мм) и 1 порт (троакар 12 мм) для работы ассистента лапароскопическими инструментами (зажим, ирригатор-аспиратор, подача шовного материала). Расположение первых двух роботических портов осуществлялось на расстояние не менее 10 см от оптического троакара. Третий роботический порт устанавливали латеральнее первого. Порт для работы ассистента устанавливали латеральнее второго роботического порта. Пациентка переводилась в литотомическое положение с последующим докингом роботической установки — подключение портов к роботическим манипуляторам. Для удобства работы ассистентов использовался боковой докинг — расположение роботической консоли справа от пациентки.
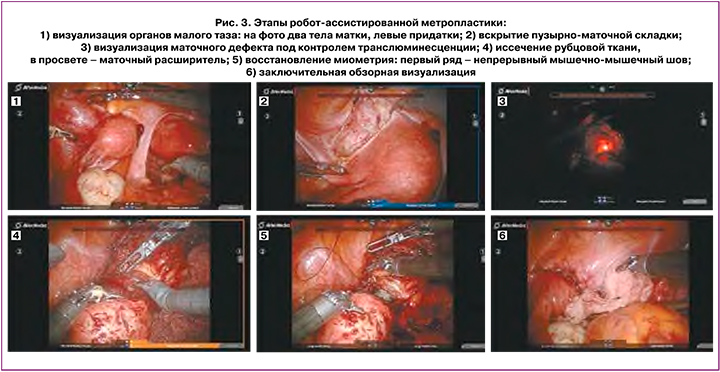
Интраоперационно было визуализировано два тела матки овоидной формы нормальных размеров бледно-розового цвета (рис. 3.1). В области перешейка левого тела матки определялась зона послеоперационного рубца в виде деформации миометрия и фиксации листка брюшины передне-маточного пространства. Выполнение метропластики начиналось с мобилизации области перешейка матки и задней стенки мочевого пузыря (рис. 3.2). Зона рубца была выделена в дистальном направлении от нижнего края на 15 мм, в латеральном направлении — до области маточных сосудов. Для улучшения точности иссечения несостоятельного рубца использовался описанный в литературе метод транслюминесценции [35]: при одновременном комбинировании гистероскопии и робот-ассисти- рованной лапароскопии наиболее тонкая область рубца фиксировалась гистероскопическим светом (рис. 3.3). Под контролем транслюминесценции вскрыта наиболее тонкая область рубца на матке. Верхний и нижний края рубца полностью иссечены с использованием моно- и биполярной энергии под контролем манипулятора, установленного в цервикальном канале (рис. 3.4). Восстановление миометрия — наиболее сложный с технической точности зрения этап операции. Миоррафия произведена в два ряда: первый ряд — непрерывный мышечномышечный шов нитью монокрил, второй ряд — непрерывный серозно-мышечный шов (рис. 3.5). С целью предотвращения сшивания передней и задней стенок цервикального канала восстановление миометрия также проводилось под контролем манипулятора, установленного в цервикальном канале левой матки. Завершена метропластика перитонизацией за счет пузырно-маточной складки брюшины (рис. 3.6).
Продолжительность операции вместе с докингом роботической установки и гистероскопическим этапом составила 150 мин. Объем кровопотери — минимальный (около 50 мл). Интра- и послеоперационных осложнений не выявлено. Ведение послеоперационного периода было стандартным для роботических операций в гинекологии. Продолжительность госпитализации составила 6 койко-дней.
На амбулаторном этапе реабилитации пациентке рекомендован прием оральных контрацептивов в непрерывном режиме и исключение беременности в течение 6 месяцев. Оценка состояния рубца на матке после метропластики проведена через 6 месяцев. Комплекс обязательного обследования включал выполнение МРТ органов малого таза с определением толщины миометрия, наличия/ отсутствия «ниши» в области рубца и гистероскопии с визуальной оценкой области рубца.
Контрольное обследование показало положи-тельные результаты выполненной метропластики роботическим доступом: «ниша» в области рубца отсутствовала, толщина миометрия составила 9,3 мм. Клинически также отмечена положительная динамика в виде купирования длительных постменструальных кровяных выделений. Отмечено сокращение общей продолжительности менструации с 15—16 дней до 5—6 дней. После контрольного обследования пациентке было разрешено планирование беременности.
Обсуждение
В настоящее время не вызывает сомнения, что несостоятельный рубец на матке является абсолютным показанием к выполнению хирургической реконструкции рубца на матке у женщин при планировании беременности. Наличие клинических симптомов, значимо нарушающих качество жизни пациенток, также является показанием для метропластики. В настоящее время коррекция рубца на матке возможна разными способами — гистероскопическим, лапаротомным, лапароско-пическим, робот-ассистированным, влагалищным. Выбор доступа зависит от цели реконструктивной операции (прегравидарная подготовка или только уменьшение клинической симптоматики), оснащения операционной, навыков и предпочтений хирургической бригады. Гистероскопический метод зарекомендовал себя как надежный, безопасный и достаточно эффективный метод коррекции рубцовой ткани при необходимости уменьшения клинической симптоматики «ниши» у пациенток, не планирующих беременность, при достаточной толщине сохраненного миометрия (более 2,5—3 мм). При выполнении реконструкции рубца на этапе прегравидной подготовки, или при наличии глубокой «ниши» с толщиной сохраненного миометрия менее 2—2,5 мм, или при неэффективности ранее выполненной гистероскопической операции целесообразно иссечение рубцовой ткани и формирование нового рубца на матке одним из возможных доступов (лапаротомным, лапароскопическим, робот-ассистированным или влагалищным). Согласно литературным публикациям, все эти доступы продемонстрировали эффективные интра- и послеоперационные результаты в виде уменьшения размеров послеоперационный ниши, увеличения толщины миометрия в области рубца, уменьшения клинической симптоматики и улучшения качества жизни пациенток. Однако в эру активного технологического прогресса и развития малоинвазивных методов лечения особый интерес представляют результаты робот-ассисти- рованной реконструкции рубца. Благодаря наличию трехмерного изображения высокой четкости, стабилизации движений и уменьшению тремора, увеличению амплитуды движения инструментов (7 степеней свободы движения), позволяющих про-изводить изгиб инструмента на 90°, в роботической системе исключаются недостатки лапароскопической хирургии.
Технические трудности выполнения метропла- стики очевидны: работа в труднодоступной области малого таза, тщательное выделение послеоперационного рубца посредством выделения переднематочной складки брюшины и мочевого пузыря, тщательное иссечение измененного миометрия, качественное сопоставление проксимального и дистального краев посредством наложения двухрядных мышечно-мышечных и серозно-мышечных швов. Два принципиально важных и ответственных этапа метропластики — это выделение и адекватное иссечение измененной рубцовой ткани и качественное сопоставление краев миометрия. Формирование спаечного процесса и плотной рубцовой ткани в области передне-маточной складки брюшины и мочевого пузыря создает технические сложности выделения рубца на матке и значительно повышает риск травмирования мочевого пузыря [1]. Также важным фактором формирования полноценного рубца является адекватное репонирование краев миометрия без чрезмерного натяжения, которое может привести к нарушению кровотока и ишемизации миометрия [1].
Преимущества роботической системы Da Vinci, по сравнению с традиционной лапароскопической, позволяют улучшить доступность к органам малого таза (особенно при аномальной анатомии и рубцово-спаечном процессе), повысить качество визуализации, создают условия для качественной, точной, прецизионной работы хирурга. Все это, несомненно, повышает качество каждого этапа метропластики и способствует формированию полноценного рубца на матке.
Особый клинический интерес нашего наблюдения связан с сочетанием двух крайне редких гинекологических патологий у пациентки репродуктивного возраста: аномалии внутренних половых органов в виде полного удвоения матки с несостоятельным рубцом после кесарева сечения в перешейке левого тела матки, а также неэффективная попытка гистероскопической резекции рубцовой ткани в анамнезе.
По данным литературы, аномалии развития матки и влагалища наблюдаются у 4,3—6,7% общей популяции женщин репродуктивного возраста [53]. Об истинной частоте несостоятельного рубца на матке судить достаточно сложно, поскольку она зависит от популяции, частоты кесарева сечения в той или иной стране, от точности используемых диагностических методик и охвата обследуемых женщин [54]. По данным анализа исходов кесарева сечения у 7883 женщин в США [55] и результатов крупного метаанализа родов после кесарева сечения [36, 48], несостоятельный рубец выявлен у 1,03 и 1,9% женщин соответственно.
Коррекция несостоятельного рубца на матке у пациентки в нашем клиническом наблюдении была обязательной ввиду планирования беременности и значительного нарушения качества жизни из-за длительных постменструальных кровяных выделений (общая продолжительность менструации достигала 15-16 дней). Комплексная предоперационная подготовка позволила диагностировать в области рубца в перешейке левого тела матки глубокую «нишу» размерами 10x8 мм и истончение миометрия до 2,5 мм. Попытка устранить клиническую симптоматику путем гистероскопической коагуляции «ниши» (в анамнезе в 2019 г.) не привела к ожидаемому результату. В данной клинической ситуации единственным возможным методом устранения клинических симптомов и подготовки пациентки к беременности являлись иссечение рубцовой ткани и формирование нового полноценного рубца, что было успешно выполнено с использованием роботической системы Da Vinci. В нашем клиническом наблюдении хирургическое вмешательство осложнялось наличием полного удвоения матки, что технически создавало трудности для визуализации послеоперационного рубца, его иссечения и миоррафии. Учитывая аномалию развития матки (полное удвоение матки), наличие рубцово-спаечного процесса в полости малого таза, очевидные трудности к доступности области рубца на левом теле матки, использование роботической системы Da Vinci позволило прецизионно выделить и иссечь рубцовую ткань, максимально качественно сопоставить миометрий и создать условия для формирования нового полноценного рубца на матке. После стандартного послеоперационного периода и амбулаторной реабилитации через 6 месяцев после реконструкции рубца был диагностирован полноценный рубец на матке: «ниша» отсутствовала, толщина миометрия составила 9,3 мм, дли-тельные постменструальные кровяные выделения купированы.
При сравнении с имеющимися незначительными литературными данными мы получили сопоставимые результаты роботической метропластики. Однако крупных исследований по оценке результатов реконструкции рубца роботическим доступом на данный момент не представлено. О недостаточности информации также сообщается в крупном метаанализе хирургических методик коррекции рубца на матке, опубликованном в 2020 г. [56]. Вероятно, это можно объяснить наиболее частым обращением пациенток с проблемой несостоятельности рубца на матке в акушерско-гинекологические (точнее, даже в акушерские) стационары, среди которых не так часто имеется роботическое оснащение.
Заключение
В настоящее время выполнение реконструкции рубца возможно разными доступами и методиками, выбор которых определяется, как целью реконструктивной операции, так и оснащением операционной и навыками хирургической бригады. Неоспорим факт активного развития малоинвазивных эндоскопических технологий, в частности робот-ассистированной хирургии. Усовершенствование возможностей роботических систем, увеличение количества уста-новленных роботических комплексов, как во всем мире, так и в России, безусловно, создает условия к увеличению доступности данной хирургической методики и расширению областей ее применения. В нашем клиническом наблюдении роботическая метропластика показала хорошие интра- и после-операционные результаты. Продемонстрированы преимущества робот-ассистированного доступа на всех основных этапах реконструкции рубца. Это позволяет считать робот-ассистированный доступ безопасным и эффективным в реконструктивной хирургии на матке.