Characteristics of uterine blood supply in women with chronic endometritis depending on the duration of infertility
Objective. To assess the hemodynamics of the uterus, including the endometrium, in women with chronic endometritis depending on the duration of infertility.Ozerskaya I.A., Ivanov V.A., Porkhovaty S.Ya., Kazaryan G.G.
Materials and methods. This was a retrospective analysis of an ultrasound study of 581 reproductive-aged women suffering from infertility and diagnosed with endometritis. All women were divided into groups according to the duration of infertility: less than 2 years, from 2 to 5 years and more than 5 years. In the uterus and endometrium, the vascularization index (VI), the flow index (FI), and the vascular-flow index (VFI) were evaluated. Dopplerography of the uterine artery showed the arterial perfusion index (API), which reflects perfusion of 1 cm3 of the uterus.
Results. According to the data of VI, FI and VFI, vascularization of the uterus and endometrium decreased not only in phase I, but also in phase II along with the increase in the duration of infertility. Arterial perfusion of the uterus decreased in phase I. There were no significant changes in the maximum blood flow rate (Vmax), pulsation index (PI), and resistance index (RI) in the groups.
Conclusion. The increase in the duration of infertility is accompanied by a decrease in vascularization not only of the endometrium, but also of the myometrium, as well as a decrease in arterial blood flow.
Keywords
At the beginning of the last century, the frequency of infertile marriages was almost 10%, while the proportion of female infertility was from 33 to 50% [1]. Nowadays, pregnancy does not occur in up to 30% of married couples in Eastern Europe and Central Asia, female infertility is noted in 45%, male infertility causes 40%, and combined infertility factors are found in 15% [2, 3]. A common cause of female infertility has been chronic endometritis (CE) which is characterized by a latent and long-term course. CE impairs a woman’s reproductive function and makes in vitro fertilization attempts unsuccessful. Moreover, it negatively affects implantation and placentation. The incidence of CE in patients with infertility and recurrent pregnancy loss is 70–80% [4–6]. According to the XVIII FIGO World Congress of Gynecology and Obstetrics (2006), V.E. Radzinsky et al. report that it is reasonable to diagnose CE in all women who have a previous history of missed pregnancy [7].
As a rule, ultrasonography is the first instrumental method for diagnosing gynecological diseases. A number of articles in Russian and foreign literature, including recent ones, have been devoted to the problem of infertility and endometrial pathology [8–12]. A large literature review is provided by E. Puente et al. [13]. According to the authors, CE is a pathology that remains understudied and it is associated with unfavorable reproductive outcomes. In their opinion, it is necessary to standardize the criteria for all methods for diagnosing CE, including histopathological analysis, immunohistochemistry and ultrasound studies.
V.N. Demidov was the first specialist in our country who described ultrasound signs of CE in 1993, later he added some markers and calculated that the sensitivity of echography is 86%, and the specificity is 92% [14]. Due to the lack of the true signs of the disease, difficulties in diagnosing and differentiation in diagnosing with other pathological processes in the endometrium, M.N. Bulanov proposed a system of points [15], which has been used by researchers [16].
The inflammatory process caused by the infectious agents results in an impaired balance of pro- and antiangiogenic factors, which are responsible for hypoxia and tissue ischemia. They affect the blood supply to the uterus in general and to the endometrium in particular [7, 17, 18].
In order to assess the blood flow in the uterus, it is possible to use the method for visualization of vessels with a 4-point characteristic of the degree of severity, which ranges from 1 (avascular endometrium) to 4 (referring to abundant blood flow). This method was suggested by specialists who published the recommendations of the IETA (International Endometrial Tumor Analysis) consensus [19]. The disadvantage of this method is a subjective evaluation, which depends on the doctor’s experience, settings, and technical level of the apparatus. The objective assessment is based on the use of 3D Doppler imaging, which makes it possible to obtain digital values of the vascularization index (VI), the flow index (FI), and the vascular-flow index (VFI). The comparison of this method and the standard Doppler assessment revelated higher accuracy of using VI, FI, and VFI [20].
Since the beginning of the 2000s, there have been works devoted to the assessment of blood supply to the mid-uterine structures using 3D Doppler imaging [21]. The constant interest of researchers in vascularization of the endometrium and subendometrial zone in women suffering from infertility has been growing since then [22–25]. Detection of these disorders in women with infertility and pregnancy loss is expected to improve the quality of diagnosis, conduct appropriate treatment, and prepare a woman for pregnancy. However, there are very few works both in our country and abroad that present the results of ultrasound examination of the uterine blood flow in patients with endometritis which is a factor of infertility [16, 26, 27].
The aim of the study was to assess the hemodynamics of the uterus, including the endometrium, in women with chronic endometritis depending on the duration of infertility.
Materials and Methods
This was a retrospective analysis of an ultrasound study of 581 reproductive-aged women suffering from infertility and diagnosed with endometritis. The age of the patients ranged from 26 to 35 years. All women were divided into groups according to the duration of infertility: less than 2 years (group I), from 2 to 5 years (group II) and more than 5 years (group III). There were 468 (80.6%) women whose menstrual cycle was in phase I and 113 (19.4%) patients with phase II of the menstrual cycle.
Clinical diagnosis of endometritis was based on patient’s complaints, history, bimanual examination, results of cytological examination of cervical smears, endometrial immunohistochemical examination results obtained by pippele biopsy or hysteroscopy, and endometrial histological examination after hysteroscopy. Clinical diagnosis of endometritis was based on patient’s complaints, history, bimanual examination, results of cytological examination of cervical smears, endometrial immunohistochemical examination results obtained by pippele biopsy or hysteroscopy, and endometrial histological examination after hysteroscopy. Cytological examination of the discharge from the cervical canal and vagina was performed in 581 (100%) patients, pipelle biopsy with morphological and (or) immunohistochemical examination was carried out in 437 (75.2%) patients, hysteroscopy with morphological and (or) immunohistochemical examination was performed in 114 (19.6%) patients, and bacteriological analysis of the discharge from the uterine cavity was conducted in 69 (11.9%) patients.
The blood test did not reveal any abnormalities in the level of hormones in all the patients and corresponded to the phase of the menstrual cycle.
The pelvic organs were examined using iU22 and Epiq7 ultrasound systems (Philips, the Netherlands).
The quantitative assessment of vascularization degree consisted in obtaining VI, FI and VFI. In order to get the listed indices, it is necessary to use the QLab application program that works with 3D angio reconstruction. Owing to the adjustment of the magnification, the uterus took up almost the entire screen of the monitor. The speed parameter was 3 cm/s, and the color flow mapping had the maximum value before the appearance of acoustic noise. The angle of construction of the 3D object was 85º so that the entire uterus entered the study area. Manual outline of the uterus contour was carried out using 10 planes. The indicators of these indices in the endometrium were obtained in a similar way.
The next step was to evaluate the hemodynamics of the uterus using the indicators of both uterine arteries. The diameter of the uterine arteries was measured in the straightest section along the color contour perpendicular to the axis of the vessel. Not only whole numbers, but also tenths of a millimeter were taken into account.
Pulsed wave doppler of the uterine artery was used to study such indicators as the maximum blood flow velocity (Vmax) (cm/s), the pulsation index (PI) and resistance index (RI), which appear on the monitor screen during automatic spectrum tracing. When obtaining angle-dependent parameters of velocity, an adequate angle of insonation was correlated.
The arterial perfusion index (API) was subsequently determined; it reflects the perfusion of 1 cm3 of the uterine body with blood flowing through both uterine arteries and it is expressed as a percentage. For this purpose, the volumetric blood flow (cm3 per cardiac cycle) in each of the uterine arteries was calculated using the following formula:
Vvol = Vmean S, where S is the area of the uterine artery (cm2).
The area of the vessel was calculated using the standard circular formula:
S = ¼πd2, where d is the diameter of the artery (cm). API is calculated using the formula:
API (%) = (VvolRUA + VvolLUA) / Vuterus х 100, where VvolRUA is the volume of blood flow through the right uterine artery (cm3); VvolLUA is the volume of blood flow through the left uterine artery (cm3); Vuterus is the volume of the uterus (cm3).
It should be noted that the study did not include patients with fibroids, internal endometriosis, or any pathology of the adnexa. Due to the fact that the physiological blood supply to the uterus decreases in late reproductive age, women over 35 years of age were also excluded from the study [28].
Statistical analysis
The results were processed using standard statistical methods with MS Excel and MedCalc resources.
When studying the type of distribution, the values of the Shapiro-Wilk test and frequency histograms were evaluated. Given that some of the data did not follow the normal distribution, all the results are presented as median and interquartile range. The differences were considered statistically significant at the level of p<0.05.
Results
During the first phase of the menstrual cycle, we examined 176 (37.6%) patients with infertility lasting less than 5 years, 153 (32.7%) patients with infertility from 2 to 5 years, and 139 (29.7%) women with infertility lasting more than 5 years. During the second phase, 22 (19.5%), 40 (35.4%) and 51 (45.1%) women were examined, respectively. The age of patients and the day of the menstrual cycle in both phases in the groups of patients did not differ significantly (p>0.05).
In the second phase of the cycle, ovulation occurred in 45 (39.8%) patients, with the right ovary ovulating in 26 (57.8%) cases and the left ovary in 19 (42.2%) cases. Anovulatory cycles were observed in 68 (60.2%) women. The analysis of blood flow indicators did not reveal any asymmetry in the digital values of the right and left uterine arteries.
In the proliferative phase of the cycle, Vmax and PI indicators did not depend on the duration of infertility (p>0.05).
There was a tendency to an increase in RI in the proliferative phase as infertility became longer. Therefore, the values in the group with infertility up to 2 years were 0.85 (0.79; 0.90), in the group with infertility from 2 to 5 years the values were 0.86 (0.80; 0.91), and in the group with infertility over 5 years the values were 0.89 (0.86-0.98). In the secretory phase of the cycle, no dependence was detected in the groups (Table 1).
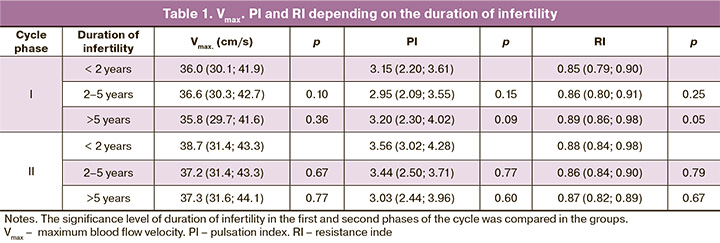
The API indicators in the first phase of the cycle in the groups were statistically significantly different (p<0.05), decreasing from 1.1% (0.7; 1.3, if the duration of infertility was less than 2 years) to 0.9% (0.6; 1.2, if infertility was from 2 to 5 years). When infertility was observed for more than 5 years, API was 0.8% (0.5; 1.0). In the second phase of the menstrual cycle, the indicators did not differ in groups.
According to the data of the VI indicator, uterine vascularization decreased not only in the first phase, but also in the second phase of the cycle as the duration of infertility increased, and the difference was statistically significant (p<0.001). So, the median of the VI indicator was almost twice lower in the group with infertility from 2 to 5 years than one in the group with infertility up to 2 years, and amounted to 5.7% (4.4; 7.1) versus 9.8% (6.2; 12.6), respectively. In the group with infertility lasting more than 5 years, the decrease of vascularization continued, reaching 4.0% (2.9; 5.4). In the secretory phase, this trend persisted, and depending on the duration of infertility, the VI findings are as follows: 10.8% (7.8; 13.5), 6.2% (4.8; 7.3) and 4.8% (3.5; 6.3), respectively.
As for the FI indicator, there were no such marked changes. Statistically significant differences (p<0.001) were observed in the first phase of the cycle only the group with infertility up to 2 years, namely 18.9 (15.4; 22.2), compared to women with infertility from 2 to 5 years, namely 16.7 (13.4; 18.9). In the second phase in similar groups, these values were 19.9 (15.8; 25.2) and 16.7 (14.3; 18.8), respectively. If the duration of infertility was more than 5 years in the proliferative phase, the FI value was 15.7 (11.8; 18.6), and in the secretory phase this value was 15.2 (11.6; 17.3).
Since the VFI values were dependent on VI and FI, they were significantly different in both phases of the cycle in the groups, decreasing as the duration of infertility increased. VFI in the first phase was 2.0 (1.0; 2.5), 1.0 (0.6; 1.3) and 0.7 (0.4; 0.9), and in the second phase it was 2.2 (1.3; 3.2), 1.1 (0.7; 1.3) and 0.8 (0.4; 1.1), respectively (Table 2).
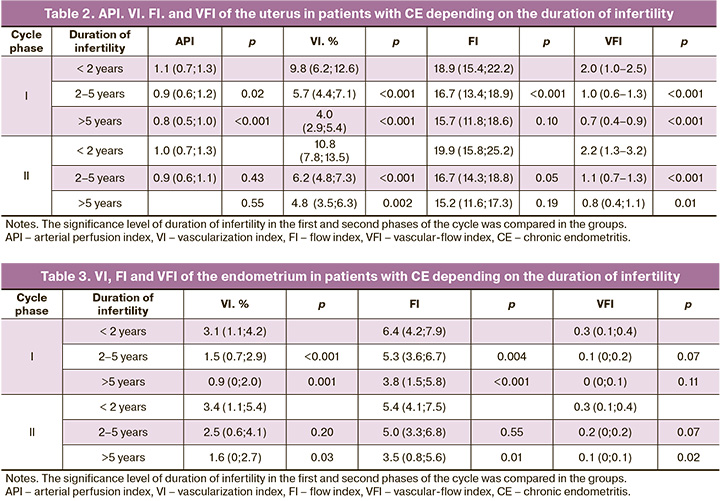
Endometrial vascularization was lower than myometrial vascularization which was proved by the findings of VI. This index progressively decreased in the proliferative phase; its values were 3.1% (1.1; 4.2) in the group with the minimum duration of infertility, 1.5% (0.7; 2.9) in the group with infertility from 2 to 5 years, and 0.9% (0; 2.0) in the group with infertility for more than 5 years. In the secretory phase, the VI indicators were 3.4% (1.1; 5.4), 2.5% (0.6; 4.1) and 1.6% (0; 2.7), respectively; a statistically significant (p<0.05) difference was found only in the group of patients who were infertile for more than 5 years.
The FI data were obtained with similar dynamics: the values in the first phase of the cycle were 6.4 (4.2; 7.9), 5.3 (3.6; 6.7) and 3.8 (1.5; 5.8), and in the second phase of the cycle they were 5.4 (4.1; 7.5), 5.0 (3.3; 6.8) and 3.5 (0.8; 5.6) in the groups, respectively.
There was a statistically significant difference in the VFI values (p<0.05) for the secretory phase of the cycle only in the group of patients whose infertility lasted more than 5 years; the VFI value in this group was 0.1 (0; 0.1), compared with the group with infertility duration from 2 to 5 years, where this indicator was 0.2 (0; 0.2) (Table 3).
Discussion
CE is one of the main causes of infertility and miscarriages. The duration of infertility is not totally consistent with the duration of the chronic inflammatory process. Given the latent course and nonspecific clinical signs that occur also in other gynecological diseases, CE is diagnosed when a patient suffers from infertility, one of the most common symptoms of this disease.
In case of inflammation pathophysiological changes are characterized by disorders of microcirculation in the inflamed tissue (exudation period), vasodilation, stagnation of blood and lymph circulation, and stasis, which lead to plasma exudation and migration of the white blood cells [17]. These changes affect the frequency and degree of vascularization of the uterus and, especially, the endometrium.
When color mapping was introduced into practice, the degree of vascularization was assessed subjectively. Nowadays, it is possible to assess the degree of vascularization objectively using the application programs, which show VI as a percentage of color voxels in the tissue. The degree of vascularization should be determined in points (from 1 to 4), since the use of such indicators as VI, FI, and VFI requires further research on implementation of this technique and unification of the device settings [20]. Moreover, not all medical institutions are equipped with scanners with this option, and this fact is especially relevant for our country.
According to the data of J.L. Alázar et al. (2017), who compared the results of the studies of four qualified doctors and four trainees on 3D volume processing, the reproducibility was from 0.77 to 0.96 and did not depend on experience [29]. For good reproducibility, one should always follow the standards of the device settings, which are described in detail in the literature [29, 30].
The study revealed that the VI indicator decreased in patients with endometritis, both in the uterus and in the endometrium in the first phase of the cycle, as the duration of infertility increased. This is probably due to the transition from the exudation period, when there is congestion, to the proliferation stage characterized by the excessive growth of connective tissue elements [17].
The study published by Yu.P. Titchenko and co-authors showed a sharp decrease in VI in the uterus, as well as in the endometrium, in patients with missed miscarriage and sexually transmitted infections mainly of viral etiology, in comparison with healthy women [26]. Unfortunately, the incomplete description of the 3D Doppler technique does not allow us to compare the obtained results.
The findings obtained by Chinese researchers confirm a sharp decrease in VI in women with intrauterine adhesions due to CE, which is suggestive of its long-term course [11].
M.N. Bulanov in his study noted poor vascularization of the functional layer during the secretory phase in the inflamed endometrium [15]. Similar results were obtained by Yu.P. Titchenko [26]. This fact was also noticed in our study; it is evident that there is no increase in vascularization in the secretory phase, when there are almost identical parameters of VI, both in the first and second phases of the cycle when the corresponding groups are compared for the duration of infertility. The decrease in blood supply to the middle parts of the uterus can be affected not only by CE, but also by a high frequency of anovulatory cycles, which is 60.2%, and possibly by hormonal insufficiency of the corpus luteum.
Due to the fact that subjective assessment of the presence of co-vessels in the uterine mucosa is imperfect, spiral arteries are detected in 28–30% of patients in the first phase and in 50–82% in the second phase [29, 30]. Earlier studies of the assessment of the blood supply to the endometrium in healthy reproductive-aged women revealed rare cases of avascularization, when the indicators VI, FI and VFI were equal to zero only in the early proliferative phase, while in the secretory phase, blood vessels are always registered [21, 22, 30]. Therefore, one should not consider endometrial avascularization before the 10th day of the cycle as a fact of endometritis, but avascularization in the second phase is an extremely unpleasant factor for implantation and placenta.
CE has a damaging effect on the receptors of the uterine mucosa [2, 4, 13]. Narrowing and obliteration of arterial vessels due to connective tissue proliferation as well as sclerotic and dystrophic changes in their walls due to long-term inflammation lead to an increase in peripheral resistance indices in the endometrium [16, 18, 19]. Changes in the vascular wall affect not only the endometrium, but also the myometrium. According to A.G. Yashchuk et al., patients with recurrent miscarriage had hemodynamic disorders in the form of increased RI in all uterine vessels, including the indicators of the uterine arteries [19]. Probably, the involvement of the myometrium in the process leads to an increase in the maximum speed of the uterine arteries in the proliferative phase of the cycle. In the secretory phase, these changes are less remarkable and statistically significant differences were not obtained in the course of this study. The numerical values are consistent with the data published in the Russian literature [4, 16, 19].
Spasm or obliteration of the arteries leads to an increase in RI up to 1.0 in one or both uterine arteries; it was observed in 52 (11.1%) patients in the first phase and in 11 (9.7%) patients in the second phase in all groups, regardless of the duration of infertility. Such high resistance at the level of uterine arteries can be associated with spasm due to edema not only in the endometrium, but also in the myometrium and impaired venous outflow. Obliteration and sclerosis, which occur as a reaction of connective tissue proliferation, also lead to high vascular resistance and, as a consequence, endometrial ischemia [5, 10], which reduces its receptivity [13].
As the duration of infertility increases, API stays rather monotonous, and does not differ significantly in the secretory phase. Analyzing the digital values of the fluctuation range of API, attention is drawn to very low indicators of some women (0.3–0.5%), while indicators of others correspond to the parameters of healthy women (1.4–2.2%) [30]; however, there are patients with low indicators and women with indicators of healthy women in each group.
The combination of API and VI indicators is of particular interest: API gives an insight into the arterial blood flow, and VI shows the total arteriovenous blood flow. Thus, the specific values of these indices suggest the stage of the inflammatory process. For example, both hyper- and hypovascularization of the endometrium may occur when a patient has monotonous values of the API. If there is absolute or relative hypervascularization, which confirms venous stasis, impaired venous outflow, it should be noted that it occurs more often in patients with infertility lasting up to 2 years. If the duration of infertility increases, then the arterial flow and arteriovenous blood flow decreases not only in the mucosa before avascularization, but also in the myometrium, which is especially evident in the first phase of the cycle. Thus, as infertility increases in its duration, impaired uterine hemodynamics without its correction but accompanied by CE leads to infertility that cannot be treated, even using assisted reproductive technologies [23–25].
There is no discussion of the practical significance and use of the flow index in the Russian and foreign literature, therefore, further study is required.
Conclusion
The study shows that it is possible to diagnose impairments of hemodynamics in the uterus, including endometrium, using objective techniques, such as 3D dopplerography (VI, FI, VFI), as well as arterial perfusion index (API). The increase in the duration of infertility is accompanied by a decrease in vascularization not only of the endometrium, but also of the myometrium, as well as a decrease in arterial blood flow. Despite the information received on changes in blood flow in the inflammatory process of the uterine mucosa, further research is needed to conduct for determining clinical, morphological and echographic correlations.
References
- Менге К., Опитц Е., ред. Руководство по гинекологии. Пер. с нем. Петро-град: Практическая медицина; 1914: 321-8. [Menge C., Opitz E., ed. Guide to gynecology. Transl. from German. Petrograd: Publishing House "Practical Medicine" (V.S. Ettinger). 1914; 321-8. (in Russian)].
- Радзинский В.Е., ред. Бесплодный брак: версии и контраверсии. М.: ГЭОТАР-Медиа; 2019: 40-9. [Radzinsky V.E., ed. Infertile marriage: versions and contraverses. M.: GEOTAR-Media; 2019: 40-9 (in Russian)].
- Кулаков В.И., Манухин И.Б., Савельева Г.М., ред. Гинекология. Нацио-нальное руководство. М.: ГЭОТАР-Медиа; 2007: 576-607. [Kulakov V.I., Manukhin I.B., Savelyeva G.M., ed. Gynecology: national leadership. M.: GEOTAR-Media; 2007: 576-607. (in Russian)].
- Цаллагова Л.В., Кабулова И.В., Золоева И.А. Роль хронического эндометрита в генезе бесплодия. Кубанский научный медицинский вестник. 2014; 4: 131-6. [Tsallagova L.V., Kabulova I.V., Zoloeva I.A. Role in the genesis of chronic endometritis infertility. Kubanskiy nauchnyy meditsinkiy vestnik/Kuban Scientific Medical Bulletin. 2014; 4 (146): 131-6. (in Russian)].
- Базина М.И., Егорова А.Т., Ходорович Н.А., Сыромятникова С.А., Кириченко А.К., Хоржевский В.А. Хронический эндометрит: скрытая угроза репродукции. Доктор.Ру. 2015; 14: 20-7. [Bazina M.I., Egorova A.T., Khodorovich N.A., Syromyatnikova S.A., Kirichenko A.K., Khorzhevsky V.A. Chronic endometritis: a hidden threat of reproduction. Doctor.Ru. Ginekologiya Endokrinologiya/Gynecology Endocrinology. 2015; 14 (115): 20-7. (in Russian)].
- Шалина Р.И., Михалева М.В., Кирющенков А.П., Шаманова М.Б., Гаврилина Е.Н. Дифференцированный подход к прегравидарной подготовке у пациенток с привычным невынашиванием беременности в анамнезе. Рос-сийский вестник акушера-гинеколога. 2015; 15(5): 36-40. [Shalina R.I., Mikhaleva M.V., Kiryushchenkov A.P., Shamanova M.B., Gavrilina E.N. A differential approach to pregravid preparation in patients with a history of recurrent miscarriage. Rossiyskiy vestnik akushera-ginekologa/Russian Bulletin of the Obstetrician-Gynecologist. 2015; 5: 36-40. (in Russian)]. https://dx.doi.org/10.17116/rosakush201515436-40.
- Радзинский В.Е., Ордиянц И.М., Добрецова Т.А. Эндометрий в огне. Острое и хроническое воспаление эндометрия: от новых взглядов к новым стратегиям. StatusPraesens. Гинекология, акушерство, бесплодный брак. 2016; 2: 126-32. [Radzinsky V.E., Ordiyants I.M., Dobretsova T.A. Endome-trium on fire. Acute and chronic inflammation of the endometrium: from new perspectives to new strategies. StatusPraesens. Ginekologiya, akusherstvo, besplodnyy brak/Gynecology, obstetrics, barren marriage. 2016; 2: 126-32. (in Russian)].
- Малева Т.А. Современные методы диагностики хронического эндометрита (обзор литературы). Международный журнал прикладных и фундаментальных исследований. 2016; 4: 566-8. [Maleva T.A. Modern methods of diagnosis of chronic endometritis (review of literature). Mezhdunarodny zhurnal prikladnykh i fundamentalnykh issledovany/International Journal of Applied and Fundamental Research. 2016; 4: 566-8. (in Russian)].
- Доброхотова Ю.Э., Боровкова Е.И., Скальная В.С., Ильязов Т.К., Рассохина О.В. Клинико-иммунологические параллели у пациенток с бесплодием и хроническим эндометритом до и после экзогенной цитокинотерапии. Акушерство и гинекология. 2019; 12: 154-60. [Dobrokhotova Yu.E., Borovkova E.I., Skalnaya V.S., Ilyazov T.K., Rassokhina O.V. Clinical and immunological parallels in patients with infertility and chronic endometritis before and after exogenous cytokine therapy. Akusherstvo i ginekologiya/Obstetrics and gynecology. 2019; 12: 154-60 (in Russian)]. https://dx.doi.org/10.18565/aig.2019.12.154-160.
- Klenov V., van Voorhis B. Ultrasound in infertility treatment. Clin. Obstet. Gynecol. 2017; 60(1): 108-20. https://dx.doi.org/10.1097/GRF.0000000000000263.
- Ni J., Han B., Liang J., Wang F. Three-dimensional 3D ultrasound combined with power Doppler for the differential diagnosis of endometrial lesions among infertile women. Int. J. Gynaecol. Obstet. 2019; 145(2): 212-8. https://dx.doi.org/10.1002 / ijgo.12787.
- Campbell S. Ultrasound evaluation in female infertility: Part 2, the uterus and implantation of the embryo. Obstet. Gynecol. Clin. North Am. 2019; 46(4): 697-713. https://dx.doi.org/10.1016/j.ogc.2019.08.002.
- Puente E., Alonso L., Laganà A.S., Ghezzi F., Casarin J., Carugno J. Chronic endometritis: old problem, novel insights and future challenges. Int. J. Fertil. Steril. 2020; 13(4): 250-6. https://dx.doi.org/10.22074/ijfs.2020.5779.
- Демидов В.Н., Гус А.И. Эхография органов малого таза у женщин. Выпуск IV. Патология полости матки и эндометрия. ВМК: Практическое пособие. М.: Издательский дом БИНОМ; 2016. 160с. [Demidov V.N., Gus A.I. Echography of pelvic organs in women. Issue IV. Pathology of the uterine cavity and endometrium. IUC: Practical manual. Moscow: Publishing house BINOM; 2016: 160 p. (in Russian)].
- Буланов М.Н. Ультразвуковая гинекология: курс лекций. ч. 1. 4-е изд. М.: Издательский дом Видар-М; 2017. 560с. [Bulanov M.N. Ultrasonic gynecologists: a course of lectures: in two parts. Part 1, Ch. 1-13. 4th ed. Moscow: Vidar-M Publishing House; 2017. 560 p. (in Russian)].
- Маринкин И.О., Трунченко Н.В., Серяпина Ю.В., Никитенко Е.В., Макаров К.Ю., Кулешов В.М., Айдагулова С.В. Хронический эндометрит с нормальным и тонким эндометрием в динамике реабилитации пациенток репродуктивного возраста: ультразвуковые и гистологические корреляции. Проблемы репродукции. 2017; 23(1): 29-36. [Marinkin I.O., Trunchenko N.V., Seryapina Yu.V., Nikiteno E.V., Makarov K.Yu., Kuleshov V.M. et al. Chronic endometritis with normal and fine endometrium in the dynamics of rehabilitation of patients of reproductive age: ultrasound and histological correlations. Problemy reproduktsii/Reproduction problems. 2017; 1: 29-36. (in Russian)]. https://dx.doi.org/10.17116/repro201723129-36.
- Шанин В.Ю. Воспаление. В кн.: Шевченко Ю.Л., ред. Клиническая патофизиология. СПб.: Специальная литература; 1998: 170-97. [Shanin V.Yu.Inflammation In: Shevchenko Yu.L., ed. Clinical pathophysiology. S.-Pb: Special Literature; 1998: 170-97. (in Russian)].
- Качалина Т.С., ред. Хронический эндометрит в репродуктивном возрасте. Современные представления об этиопатогенезе, диагностике и принципах лечения. Новые подходы к терапии. Учебное пособие. 2-е изд. Н-Новгород: Издательство Приволжского исследовательского медицинского университета; 2018. 88с. [Kachalina T.S., ed. Chronic endometritis in reproductive age. Modern ideas about etiopathogenesis, diagnosis and treatment principles. New approaches to therapy: a training manual. 2nd ed. N-Novgorod: Publishing House of the Volga Research Medical University; 2018. 88 p. (in Russian)].
- Ящук А.Г., Масленников А.В., Фаткуллина И.Б., Рахматуллина И.Р., Берг Э.А., Берг П.А. Применение сулодексида для улучшения внутриматочной гемодинамики у пациенток с невынашиванием беременности. Акушерство и гинекология. 2019; 10: 172-8. [Yashchuk A.G., Maslennikov A.V., Fatkullina I.B., Rakhmatullina I.R., Berg E.A., Berg P.A. The use of sulodexide to improve intrauterine hemodynamics in patients with miscarriage. Akusherstvo i ginekologiya/Obstetrics and gynecology. 2019; 10: 172-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.10.172-178.
- Leone F.P., Timmerman D., Bourne T., Valentin L., Epstein E., Goldstein S.R. et al. Terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: a consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet. Gynecol. 2010; 35(1): 103-12. https://dx.doi.org/10.1002/uog.7487.
- Alcázar J.L., Kudla M.J. Three-dimensional vascular indices calculated using conventional power Doppler and high-definition flow imaging: are there differences? J. Ultrasound Med. 2010; 29(5): 761-6. https://dx.doi.org/10.7863/jum.2010.29.5.761.
- Raine-Fenning N.J., Campbell B.K., Kendall N.R., Clewes J.S., Johnson I.R. Quantifying the changes in endometrial vascularity throughout the normal menstrual cycle with three-dimensional power Doppler angiography. Hum. Reprod. 2004; 19(2): 330-8.
- Kim A., Han J.E., Yoon T.K., Lyu S.W., Seok H.H., Won H.J. Relationship between endometrial and subendometrial blood flow measured by three-dimensional power Doppler ultrasound and pregnancy after intrauterine insemination. Fertil. Steril. 2010; 94(2): 747-52. https://dx.doi.org/10.1016/j.fertnstert.2009.03.084.
- Wang J., Xia F., Zhou Y., Wei X., Zhuang Y., Huang Y. Association between endometrial/subendometrial vasculature and embryo transfer outcome: a meta-analysis and subgroup analysis. J. Ultrasound Med. 2018; 37(1): 149-63. https://dx.doi.org/10.1002/jum.14319.
- Wang L., Lv S., Mao W., Pei M., Yang X. Assessment of endometrial receptivity during implantation window in women with unexplained infertility. Gynecol. Endocrinol. 2020; 36(10): 917-21.https://dx.doi.org/10.1080/09513590.2020.1727433.
- Титченко Ю.П., Зароченцева Н.В., Аршакян А.К., Меньшикова Н.С. Применение ультразвуковых методов исследования в оценке состояния эндометрия у пациенток с хроническим эндометритом и невынашиванием беременности. Российский вестник акушера-гинеколога. 2014; 14(1): 55-8. [Titchenko Yu.P., Zarochentseva N.V., Arshakyan A.K., Menshikova N.S. Use of ultrasound techniques in the evaluation of the endometrium in patients with chronic endometritis and miscarriage. Rossiyskiy vestnik akushera-ginekologa/Russian Bulletin of the Obstetrician-Gynecologist. 2014; 1: 55-8. (in Russian)].
- Cicinelli E., Matteo М., Tinelli R., Lepera A., Alfonso R., Indraccolo U. et al. Prevalence of chronic endometritis in repeated unexplained implantation failure and the IVF success rate after antibiotic therapy. Hum. Reprod. 2015; 30(2): 323-30. https://dx.doi.org/10.1093/humrep/ deu292.
- Engels V., Sanfrutos L., Pérez-Medina T., Álvarez P., Zapardiel I., Bueno B. et al. Evaluation of endometrial and subendometrial vascularization and endometrial volume by 3-D power Doppler ultrasound and its relationship with age and pregnancy in intrauterine insemination cycles. Gynecol. Obstet. Invest. 2011; 72(2): 117-22. https://dx.doi.org/10.1159/000323777.
- Alcázar J.L., Pascual M.A., Ajossa S., de Lorenzo C., Piras A., Hereter L. et al.Reproducibility of the International Endometrial Analysis group color score for assigning the amount of flow within the endometrium using stored 3-dimensional volume. J. Ultrasound Med. 2017; 36(7): 1347-54. https://dx.doi.org/10.7863/ultra.16.06002.
- Озерская И.А. Эхография в гинекологии. 3-е изд. М.: Издательский дом Видар-М; 2020. 704с. [Ozerskaya I.A. Sonography in gynecology. 3rd ed., Revised. and add. Moscow: Publishing house Vidar-M; 2020. 704 p. (in Russian)].
Received 13.04.2020
Accepted 07.05.2020
About the Authors
Irina A. Ozerskaya, M.D., Ph.D., Professor, Ultrasound Diagnostics and Surgery Department, Peoples’ Friendship University of Russia.Tel.: +7(926)606-09-05. E-mail: ozerskaya_usd@mail.ru. ORCID: 0000-0001-8929-6001. 6 Miklukho-Maklaya str., Moscow, 117198, Russian Federation.
Vladimir A. Ivanov, M.D., Ph.D., Full Professor, Head of the Department of Ultrasound Diagnostics and Surgery, Peoples’ Friendship University of Russia.
Tel.: +7(985)272-50-02. E-mail: ivanov.rudn@mail.ru. ORCID: 0000-0001-7208-3560. 6 Miklukho-Maklaya str., Moscow, 117198, Russian Federation.
Sergey Ya. Porkhovaty, Ph.D., ultrasound diagnostician, Asklepion Medical Center. Tel.: +7(915)309-82-97. E-mail: oracul2003@gmail.com.
41-2 Dubravnaya str., Moscow, 125222, Russian Federation.
Gayane G. Kazaryan, ultrasound diagnostician, Scientific and Practical Center for Minimally Invasive Surgery and Gynecology.
Tel.: +7(916)552-12-71. E-mail: 79165521271@yandex.ru. 9-5 Michurinsky Prospekt, Moscow, 119607, Russian Federation.
For citation: Ozerskaya I.A., Ivanov V.A., Porkhovaty S.Ya., Kazaryan G.G. Characteristics of uterine blood supply in women with chronic endometritis depending on the duration of infertility.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 10: 105-112 (in Russian)
https://dx.doi.org/10.18565/aig.2020.10.105-112