Characteristics of menopausal hormone therapy use in Russia: results of a large-scale survey of peri- and postmenopausal women
Smetnik A.A., Ivanov I.A., Ermakova E.I., Tabeeva G.I.
Menopause is accompanied by various symptoms that can reduce the quality of life of women and have an impact on society as a whole. The identification of factors that contribute and prevent the use of menopausal hormone therapy (MHT) can provide additional opportunities and perspectives for changing attitudes towards menopause and MHT. The article was prepared by the Russian Society of Gynecological Endocrinology and Menopause (ROSGEM)
Objective: To identify and systematize the causes of the low prevalence of MHT in Russia in terms of patient perception of the problem.
Materials and methods: The study was conducted by Ipsos Comcon through an online survey of 2,536 women aged 45–59 living in Russian cities with populations over 100,000 people. Among them, 1,743 were peri- and postmenopausal women. National representative quotas were established by gender, age, and federal district. All the respondents were divided into three groups: 45–49 years old (n=890), 50–54 years old (n=835) and 55–59 years old (n=811). In addition to the main sample, the survey included 200 women who had some experience in taking MHT over the past 12 months: 100 women took herbal medicines to relieve menopausal symptoms over the past 12 months, and 100 women previously took MHT but stopped using it less than 12 months after starting therapy.
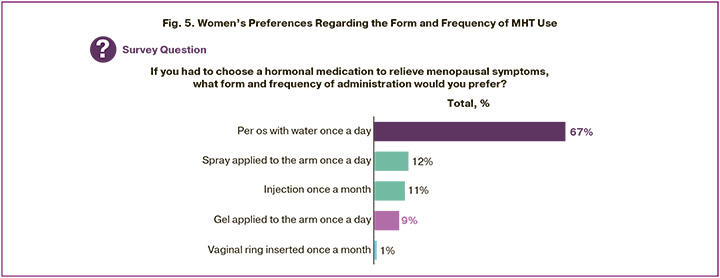
Results: The study revealed that 97.5% of women aged 45–59 years who were in the peri- and post-menopausal stages experienced at least one symptom of menopausal syndrome. The symptoms of menopause were rated as moderate or severe by 74% of patients. The women agree that their quality of life should not deteriorate during menopause (90%1). Endocrinological (55%) and vasomotor (56%) symptoms were often the cause for seeking medical help. Among all the medical professionals, the gynecologist was the primary source of knowledge (93%) about symptoms and therapy. However, gynecologists seldom initiated active discussions about menopause with their patients. Among women who went to the doctor at least once during menopause (n=845/1088), only 20% of women reported that the doctor was the first to initiate a conversation about menopause. Women who were aware of the appropriate treatment method perceived MHT as a therapy that totally relieves peri- and postmenopausal symptoms (49%) compared with non-hormonal therapy (36%) and combined oral contraceptives (23%). Most Russian women (67%) aged 45–59 years who associate health changes with the approach/onset of menopause and do not deny hormone therapy in the future preferred the oral route of MHT administration and only 9% of women chose the transdermal route. The need for information about MHT was reported by about 58% of women. The recommendation to discontinue MHT in 82% of cases (among all doctors) was given by the gynecologist. The lack of a doctor’s administration is also a significant barrier to MHT: the gynecologist did not prescribe MHT to women with severe menopausal symptoms in 21% of cases. Only 10% of women had absolute contraindications to MHT.
Conclusion: The level of MHT use in Russia increased from 1.3% to 6.5% but it remains low compared to developed countries. It is necessary to conduct educational events for gynecologists, other doctors, as well as patients. These events should provide information about menopause, its symptoms, potential long-term health consequences and they should also discuss current ideas about the safety and benefits of MHT.
Authors’ contributions: Smetnik A.A., Ivanov I.A., Ermakova E.I., Tabeeva G.I. – developing the concept of the study, collecting and processing the material, writing the text, editing the article.
Conflicts of interest: Authors declare lack of the possible conflicts of interest.
Funding: The study was conducted without sponsorship.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Smetnik A.A., Ivanov I.A., Ermakova E.I., Tabeeva G.I.
Characteristics of menopausal hormone therapy use in Russia:
results of a large-scale survey of peri- and postmenopausal women.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (8): 196-208 (in Russian)
https://dx.doi.org/10.18565/aig.2025.200
Keywords
By 2025, it is projected that over 1 billion women worldwide will be in the peri- or postmenopausal stages. In Russia, the average age of natural menopause ranges from 49 to 51 years [1–5]. More than 80% of women in this transitional period experience symptoms of the climacteric syndrome (CS). The classical manifestations of menopause – typically lasting 8 to 10 years – include vasomotor symptoms such as hot flashes, chills, and night sweats, as well as genitourinary menopausal syndrome, which encompasses vulvovaginal atrophy and urogenital dysfunction.
Prolonged sex hormone deficiency in postmenopause contributes to the development of somatic pathologies, including musculoskeletal, cardiovascular, metabolic, psychological, and other disorders [1, 6–10]. Women often seek medical care only when symptoms become sufficiently distressing and begin to impair their quality of life [1].
Menopausal symptoms can significantly limit social engagement, reduce productivity, and lead to decreased work capacity or even job loss [1]. According to some estimates, the economic burden in Russia associated with reduced work capacity due to climacteric syndrome, comorbid somatic conditions, and mortality exceeds 9 billion rubles annually [11].
According to recommendations from leading international menopause societies, including the International Menopause Society (IMS), North American Menopause Society (NAMS), European Menopause and Andropause Society (EMAS), National Institute for Health and Care Excellence (NICE), and British Menopause Society (BMS) as well as national guidelines from the Russian Society of Obstetricians and Gynecologists (RSOG) and the position of the Russian Society of Specialists in Gynecological Endocrinology and Menopause (ROSSGEM), menopausal hormone therapy (MHT) is considered the first-line treatment for climacteric disorders [3, 7, 10, 12–21].
MHT has substantial potential to improve the physical, social, and psychological well-being of women during peri- and postmenopause, extend healthy life expectancy, and generate significant economic benefits. Nevertheless, menopause and MHT remain subjects of ongoing debate and persistent misconceptions, which continue to negatively affect many women and society at large [1, 2].
A gynecologist’s primary responsibility is to ensure the rational selection of menopausal hormone therapy (MHT), including the relevant formulation, the lowest effective dose, an appropriate treatment regimen tailored to the clinical presentation, and the preferred route of administration based on the patient’s individual needs and characteristics.
Robust clinical evidence indicates that oral MHT can significantly improve women's quality of life, fully alleviate vasomotor symptoms in more than 75% of cases, reduce the risk of developing type 2 diabetes by 30%, substantially lower the incidence of disabling fractures—including hip fractures – and decrease cardiovascular mortality by 12–54%, as well as all-cause mortality by 31% [3, 7, 10].
The widespread integration of MHT into clinical practice, when indicated and in the absence of contraindications, represents a critical direction for advancing women's healthcare [1].
Significant demographic trends, including an increasing prevalence of early menopause and premature ovarian insufficiency, necessitate a revision of current approaches to identifying and managing estrogen-deficient conditions, as well as the development of new health maintenance programs. Modern medicine offers both the tools and the potential to reshape societal and clinical attitudes toward menopause and menopausal hormone therapy (MHT).
A key component of this effort is the identification of factors that facilitate or hinder the uptake of MHT. To address this, Ipsos Comcon LLC conducted a study aimed at identifying and systematizing patient-perceived reasons for the low prevalence of MHT use in Russia. Based on the findings of this research, the Russian Society of Specialists in Gynecological Endocrinology and Menopause (ROSSGEM) prepared the present article.
Materials and methods
The study was conducted by Ipsos Comcon LLC through an online survey of 2,536 women aged 45–59 years residing in Russian cities with populations exceeding 100,000. The aim was to assess their awareness of menopause and approaches to managing menopause-related conditions. From the total sample (general female population, GFP), 1,743 women were identified as being in peri- or postmenopausal stages (target menopausal population, TMP). The sampling included major cities across Russia and was based on nationally representative quotas by gender, age, and federal district. All respondents (GFP, n=2,536) were stratified into three age groups: 45–49 years (n=890), 50–54 years (n=835), and 55–59 years (n=811). Additionally, the study incorporated three subgroups: 200 women who had used menopausal hormone therapy (MHT) within the past 12 months, 100 women who had used herbal medicinal products for symptom management during the same period, and 100 women who had discontinued MHT within 12 months of initiating treatment.
The questionnaire was designed in accordance with established protocols for large-scale sociological research. Each interview lasted approximately 35 minutes. The severity of menopausal symptoms was evaluated using the Greene Climacteric Scale, in line with the 2021 clinical guidelines issued by the Ministry of Health of the Russian Federation, titled “Menopause and Climacteric Conditions in Women”, which were valid at the time of data collection.
Results
Prevalence and Clinical Presentation of Menopausal Symptoms
The first section of the questionnaire focused on the prevalence of menopausal symptoms – specifically psycho-emotional, vasomotor, endocrine, musculoskeletal, urogenital, and sexual issues—as key factors influencing the start of menopausal hormone therapy (MHT). Figure 1 illustrates the prevalence and severity of climacteric symptoms among peri- and postmenopausal women aged 45–59 years (TMP, n=1,743). The survey revealed that 97.5% of respondents reported experiencing at least one climacteric symptom.
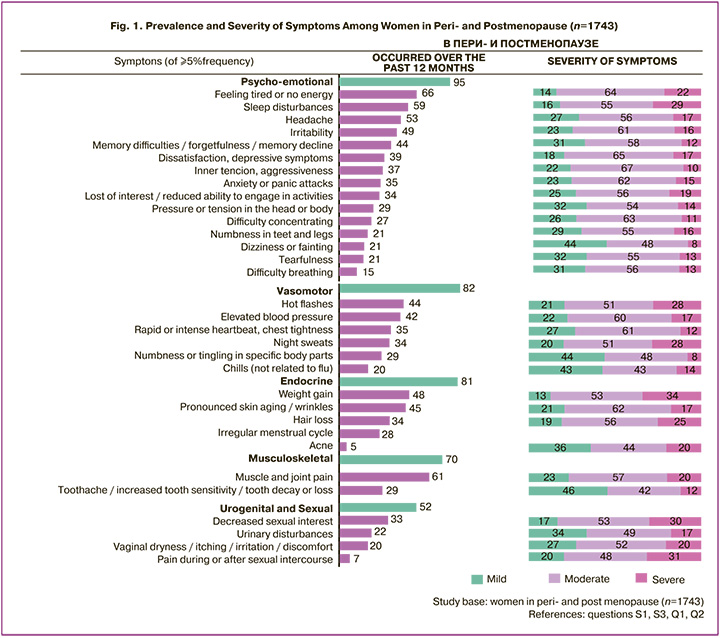
Among peri- and postmenopausal women (n=1,743), 95% reported experiencing psycho-emotional symptoms within the past 12 months. Fatigue was noted by 66% of respondents, while sleep disturbances were reported by 59%. According to the Greene Climacteric Scale, these symptoms were classified as moderate to severe in 86% and 84% of cases, respectively.
Vasomotor symptoms were reported by 82% of women in the same group. Specifically, 44% experienced hot flashes, 42% reported troubling elevated blood pressure, 35% noted episodes of rapid or intense heartbeat and chest tightness, and 34% experienced night sweats. Based on the Greene Scale, hot flashes and night sweats were identified as moderate to severe by 79% of women who experienced these symptoms.
Among peri- and postmenopausal women (n=1,743), 81% reported experiencing endocrine-related symptoms, with weight gain being the most frequently mentioned (48%). In the broader sample of women (GFP, n=2,536), the prevalence of weight gain was 44%, with a clear age-related trend: 47% of women aged 55–59 years (n=811) reported weight gain, compared to 41% in the 45–49 age group (n=890). Among those who experienced weight gain (TMP, n=1,743), 34% rated the symptom as severe and 53% as moderate.
Pronounced skin aging was also commonly reported (45%). Among those affected, 17% rated it as severe and 62% as moderate. Hair loss was reported by 34% of respondents, and 28% noted irregular menstrual cycles.
Musculo-skeletal complaints were reported by 70% of women (TMP, n=1,743), with joint and muscle pain being the most prevalent (61%). According to the Greene Climacteric Scale, this symptom was rated as severe by 20% and moderate by 57% of those affected.
Urogenital and sexual health issues affected more than half of the respondents (52%), including decreased sexual interest (33%), urinary disturbances (22%), and vaginal dryness (20%). Among those who experienced these symptoms, decreased libido and pain during or after intercourse were most frequently rated as severe – by 30% and 31% of women, respectively (TMP, n=1,743).
An analysis of climacteric symptoms based on their frequency and impact among peri- and postmenopausal women (n=1,743) (Fig. 2) revealed that the most persistent and distressing symptoms1 for women aged 45–59 were external manifestations such as weight gain, hair loss, and the appearance of wrinkles, along with fatigue, sleep disturbances, and night sweats. Although dyspareunia was reported by a relatively smaller proportion of women, it was identified as highly distressing among those affected. Other symptoms such as elevated blood pressure, difficulty concentrating, anxiety, and urinary disturbances were also frequently described as significantly bothersome. Hot flashes were both common and impactful among peri- and postmenopausal women.
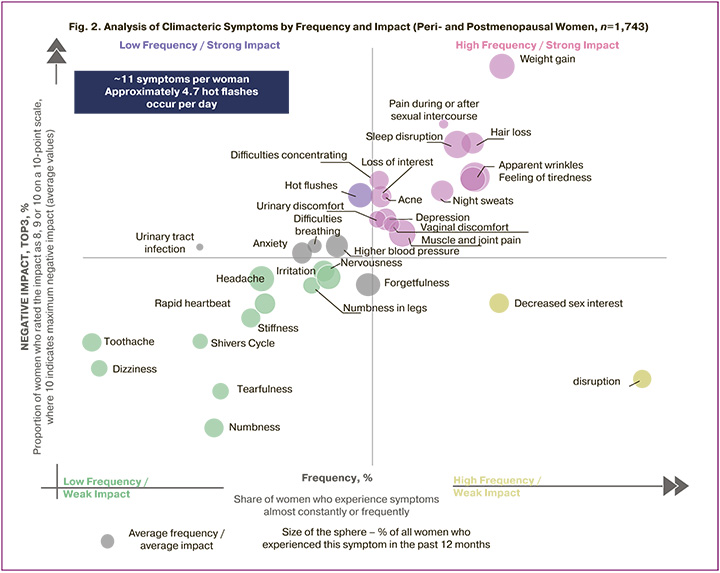
Overall, menopause was most frequently associated with psycho-emotional, vasomotor, and endocrine disturbances. Among these, weight gain was most often rated as severe, with 34% of affected women classifying it as such.
Perception of Menopause and Healthcare-Seeking Behavior among Women with Climacteric Symptoms
Among peri- and postmenopausal women who associated their symptoms with the onset or approach of menopause (n=1,334/1,743), many reported experiencing negative emotions such as sadness (28%) and anxiety (17%). However, 29% indicated feeling emotionally neutral, and 12% even described a sense of liberation.
While the majority of respondents (90%) agreed2 that their quality of life should not decline during menopause, only 46% believed that menopausal symptoms should not be ignored. Notably, this figure rose to 79% among women currently using menopausal hormone therapy (MHT, n=342). Younger women aged 45–49 (n=361/1,743) were more likely than older age groups to support the use of medications to alleviate menopausal symptoms (50%), a view shared by 48% of those experiencing severe symptoms (n=810/1,743).
The survey revealed that 55% of women who associated their symptoms with menopause or experienced hot flashes, night sweats, or menstrual irregularities (n=1,985) had consulted a gynecologist. In 67% of these cases, the discussion of menopause was initiated by the patient. Among those who had ever sought medical advice for menopausal symptoms (n=845/1,088), 77% were prompted by the symptoms themselves, while 7% were referred by another healthcare provider.
Endocrine (54%) and vasomotor (55%) symptoms were the most common reasons for seeking medical care among peri- and postmenopausal women. Specifically, menstrual irregularities (46%) and hot flashes (41%) were frequently cited. Psycho-emotional symptoms led 35% of women to consult a gynecologist.
Public Awareness of Menopause and Use of Symptom Management Strategies
More than half of peri- and postmenopausal women (TMP, n=1,743) reported insufficient awareness regarding menopause and available methods for alleviating climacteric symptoms. Among women who had never used menopausal hormone therapy (MHT, n=1,544), 35% had never heard of MHT, 22% expressed general concerns about hormones, 16% feared weight gain, 13% were concerned about cancer risks, and 9% feared thrombosis.
A significant proportion of respondents expressed a need for more information: 31% wanted to know which symptoms should raise concern, and 15% sought clarification on which symptoms may indicate the onset of menopause. Women aged 45–49 and those experiencing severe symptoms (65% in both groups) were more likely to report a need for additional information.
Another important factor contributing to the low uptake of MHT was the tendency to underestimate the severity of menopausal symptoms and the need for treatment. Among women who had never used MHT (n=1,544/1,743), 22% felt their symptoms were not bothersome enough to start therapy.
In the broader population (GFP, n=2,536), 72% of women associated at least one symptom with the onset or approach of menopause. However, 69% believed their symptoms could be indicative of a chronic condition, such as cardiovascular or endocrine disease. Additionally, 64% attributed their poor health to stress, and 53% to lifestyle factors.
Regarding treatment decisions, 21% of women expressed interest in knowing when to initiate therapy for menopausal symptoms, and 22% wanted guidance on when to discontinue it. Among peri- and postmenopausal women (n=1,743), 30% reported a need for better information on MHT safety, 26% on contraindications, 24% on relevant medication choices, and 23% on treatment duration. MHT users (n=342) were particularly interested in information about the duration of therapy (43%).
A notable finding is that 40% of women aged 45–59 (GFP, n=259/2,536) who had initiated menopausal hormone therapy (MHT) eventually discontinued its use. Among them, 39% stopped treatment within the first 12 months, while 53% discontinued after one year of therapy. The most frequently cited reason for discontinuation was concerns about safety and efficacy, reported by 56% of women who ceased MHT (n=217). Additional reasons included perceived negative impact on weight (21%), fear of cancer (20%), and side effects (19%).
Non-adherence was another common factor, accounting for 40% of discontinuations. Furthermore, 22% of women opted to try alternative therapies, 10% believed MHT was unnecessary at their age, and 5% cited inconvenience in using the medications. Notably, one-third of women (34%) discontinued therapy due to symptom relief or reduction. In 14% of cases, changes in health status led to new contraindications for continued MHT use.
Among women aged 45–59 who discontinued MHT (n=217), 15% did so based on a physician’s recommendation. In 82% of these cases (n=33), the recommendation came from a gynecologist. According to patient reports, the most common reasons cited by physicians for discontinuation included achievement of therapeutic goals (36%), increased risk of cancer (21%), and limitations on treatment duration (21%).
Importantly, 41% of women who discontinued MHT (n=217) subsequently adopted alternative methods for symptom management.
Contraindications and Special Considerations for MHT Use
Among women experiencing severe climacteric symptoms who were aware of menopausal hormone therapy (MHT) but had never used it (n=691/1,544), 21% cited the absence of a physician’s recommendation as the reason for not initiating treatment. Additionally, 56% of peri- and postmenopausal women reported having health conditions or lifestyle-related risk factors that complicated the prescription of MHT. Only 10% had one or more non-modifiable absolute contraindications to MHT – such as a history or predisposition to thrombosis, acute or chronic liver disease, breast cancer, cutaneous porphyria, or estrogen-dependent malignancies (Fig. 3).
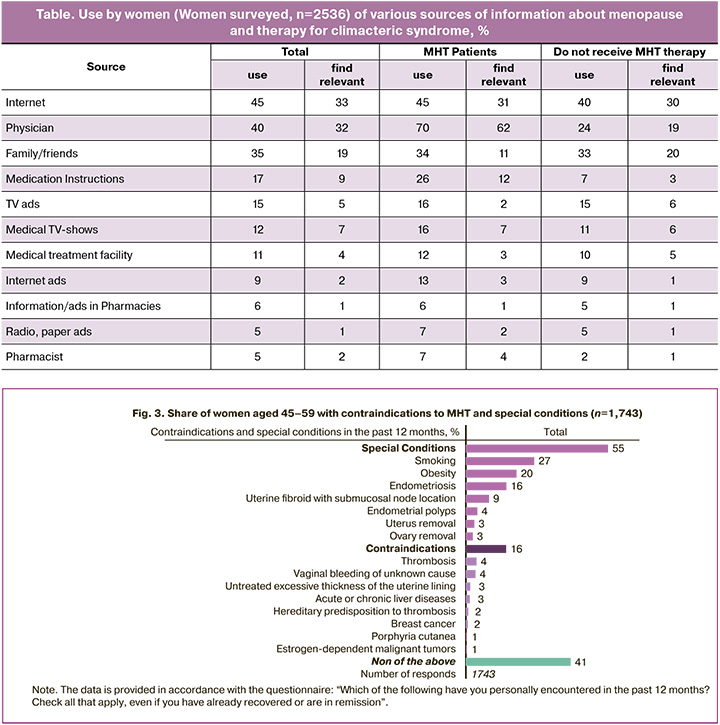
Notably, 41% of women (TMP, n=1,743) reported no known contraindications or special conditions that would preclude MHT use. However, several factors requiring caution in prescribing MHT were identified, including smoking (27%), obesity (20%), endometriosis (16%), submucosal uterine fibroids (9%), and history of hysterectomy (3%). The most commonly recognized non-modifiable contraindications included a history of thrombosis (4%), predisposition to thrombosis (2%), liver disease (3%), breast cancer (2%), and other estrogen-dependent malignancies (1%). Importantly, some of these conditions – such as endometriosis, uterine fibroids, unexplained bleeding, endometrial pathology, obesity, and smoking – may be modifiable.
Sources of Information about Menopause and MHT
Given the low level of awareness regarding MHT, the survey included questions about sources of information (Table). Most women (GFP, n=2,536) sought information about menopause and symptom relief from digital sources (45%), healthcare professionals (40%), and friends or relatives (35%). Online information was considered useful by 33% of respondents, while 32% found information from physicians helpful. However, 24% reported that none of the sources were useful.
Among MHT users, 70% received information from a physician, and 62% found it helpful. In contrast, only 19% of non-users considered physician-provided information useful. When seeking medical advice, women most frequently consulted gynecologists (93%, n=1,004/2,536). Despite this, gynecologists rarely initiated discussions about menopause. Among women who had consulted a physician at least once during menopause (n=845/1,088), only 19% reported that the physician initiated the conversation.
Of all peri- and postmenopausal women who had consulted a specialist at least once (n=1,088), only 25% (n=845) reported being prescribed MHT. Interestingly, unlike general discussions about menopause, MHT prescriptions were initiated by physicians in 67% of cases among those who received therapy (n=260).
Use of MHT and Other Methods for Managing Climacteric Symptoms
Among peri- and postmenopausal women (TMP, n=1,743), 74% rated their symptoms as moderate or severe. The primary motivation for initiating menopausal hormone therapy (MHT) among current patients (n=342) was the desire to alleviate physical discomfort (46%) and emotional symptoms (27%), as well as to improve overall well-being (42%). Social factors also played a significant role, including the desire to prolong youthfulness (37%), maintain physical appearance (20%), and lead a fuller life (31%). Preventive motivations, such as reducing the risk of osteoporosis (17%) and cardiovascular disease (16%), were mentioned less frequently.
Women who were aware of MHT perceived it as more effective3 in managing peri- and postmenopausal symptoms (49%) compared to non-hormonal therapies (36%) and combined oral contraceptive pills (23%)3. High efficacy of MHT was reported across all age groups and symptom severities. Among informed MHT users, 77%4 noted an improvement in quality of life after initiating therapy, and 80%5 expressed satisfaction with the results. The average self-reported improvement in quality of life was 8.4 out of 10, and overall satisfaction with MHT was rated at 8.6 out of 10.
In the general female population (GFP, n=2,536), 10.2% of women aged 45–59 living in cities with population over 100,000 had used MHT at some point. The average age of initiation was 48. In the past 12 months, 7.4% had used MHT, and 6% were current users. The average age of current users was 51 years, with an average duration of therapy of 2.8 years.
Among physician-prescribed alternatives to MHT, phytoestrogens (55%) and vitamins (45%) were most commonly recommended. Women (GFP, n=2,536) were more familiar with phytoestrogens, vitamins, and MHT as symptom management options than with physical activity, antidepressants/sedatives, or combined oral contraceptive pills. Despite relatively high awareness of MHT (62%), women more frequently used phytoestrogens and vitamins (Fig. 4).
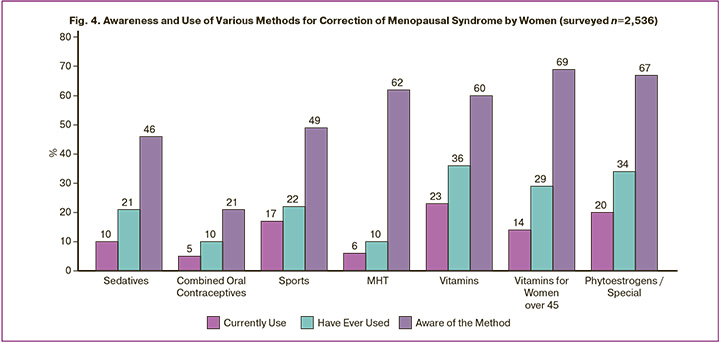
Approximately 10% of respondents had used combined oral contraceptive pills at some point, and 5% were currently using them to manage climacteric symptoms, although this is considered off-label use. Among peri- and postmenopausal women aware of combined oral contraceptive pills (n=1,485), 52% believed these pills were somewhat effective3, 21% considered them fully effective3, and 27% rated them as ineffective3. Among those aware of phytoestrogens (n=1,593), 53% rated them as somewhat effective3, 36% as fully effective3, and 11% as ineffective. Perceived effectiveness was lowest among women with severe symptoms.
Among Russian women aged 45–59 who associated health changes with the onset or approach of menopause and did not reject the possibility of future hormone therapy (GFP, n=1,131/2,536), 67% preferred per os once daily. Only 9% were open to considering transdermal gel (Fig. 5).
Among current users of menopausal hormone therapy (MHT, n=342), the average duration of treatment was approximately 3.8 years by the age of 55–59. Among those who discontinued MHT (n=113), 38% did so within the first 6–12 months of initiation. Of the women who had been prescribed MHT (n=260), 34% reported that the therapy was intended for less than one year, 10% for one to three years, 11% for three to five years, 8% for five to ten years or longer, and 15% were prescribed MHT for an indefinite period. In 8% of cases, the therapy was prescribed to be continued until symptoms resolved.
Discussion
The medical and social significance of the peri- and postmenopausal period is difficult to overstate. The most common vasomotor (hot flashes, night sweats), endocrine (weight gain), and psycho-emotional symptoms are strongly associated with a decline in quality of life and work capacity. These findings, combined with the fact that 90% of women believe their lives should not deteriorate due to the onset or approach of menopause, highlight the substantial potential of menopausal hormone therapy (MHT) – a treatment that remains underutilized.
According to the current 2021 edition and the 2024 draft of the national clinical guidelines “Menopause and Climacteric Conditions in Women”, 28.5% of women suffer from moderate to severe hot flashes. However, the present survey revealed that the prevalence of moderate and severe climacteric symptoms is significantly higher than previously estimated, reaching 74%.
Nearly all women aged 45–59 in peri- or postmenopause reported psycho-emotional symptoms (95%), yet it is endocrine (55%) and vasomotor (56%) symptoms that most often prompt them to seek medical care.
As of 2020, the rate of MHT use in the Russian Federation was only 1.3% among women aged 45–69. According to the current survey, in cities with populations over 100,000, 10.2% of women aged 45–59 (approximately 1 million) had initiated MHT at some point, 7.4% had started therapy within the past 12 months, and 6% were still in MHT therapy (approximately 588,000 women). In 2024, the total number of women aged 45–59 in Russia was estimated at around 15 million. Thus, the rate of MHT use has increased from 1.3% to 6.5% over the past five years (see calculation formula in Appendix). Despite this growth, MHT use in Russia remains significantly lower than in European countries.
Several key barriers to timely initiation and use of MHT were identified. Insufficient awareness of menopause and MHT (58%) contributes to negative stereotypes, fears, and substantial loss of patients at the pre-consultation stage. Among respondents who had never used MHT, 35% had never heard of hormone replacement as a treatment option. Approximately one-third of peri- and postmenopausal women (31%) expressed a need for information on which symptoms should raise concern. Moreover, many women attributed their climacteric symptoms to other conditions or diseases unrelated to menopause. There is a tendency to underestimate the importance of treating menopausal symptoms – only 46% of peri- and postmenopausal women agreed that such symptoms should not be ignored. As a result, many women are less likely to seek medical help.
Lack of information also contributes to negative attitudes toward MHT. Interestingly, respondents were more concerned about potential weight gain from hormone therapy (16%) than about the risk of cancer (13%) or thrombosis (9%). In general, women attempted to fill gaps in their knowledge about menopause and symptom relief through digital sources, healthcare professionals, and conversations with friends or relatives. However, most found the information insufficient. The need for more detailed guidance was especially pronounced among women entering the menopausal transition and those experiencing severe climacteric symptoms.
A critical factor contributing to the loss of potential MHT users is the stage of medical consultation. Among all healthcare professionals, gynecologists were identified as the primary opinion leaders regarding menopause and MHT. However, information about MHT provided during individual consultations was perceived by respondents as equally useful as general information found online. Notably, among MHT users, three times as many women found physician-provided information helpful compared to non-users. This may reflect, on one hand, the pivotal role of qualified specialists in guiding treatment decisions, and on the other, a general lack of trust in physicians or limited time during consultations to discuss menopause in detail.
Only 19% of respondents reported that their physician initiated a conversation about menopause during a consultation. Furthermore, gynecologists were found to recommend MHT infrequently, often favoring non-hormonal treatments or alternative therapies. MHT was frequently prescribed for short durations – one-third of patients were advised to use it for less than one year. Among all physicians, gynecologists were most likely to discontinue MHT, typically due to perceived achievement of therapeutic goals or concerns about treatment duration. The high rate of discontinuation upon symptom relief may contribute to the misconception that MHT is purely symptomatic, indicating a potential gap in physician knowledge and undermining the therapy’s preventive potential for somatic conditions.
The absence of a physician’s recommendation remains a significant barrier to MHT use: 21% of women with severe climacteric symptoms did not receive an MHT prescription. Only 10% of women had one or more non-modifiable absolute contraindications to MHT. Regarding special conditions and contraindications, the frequently discussed clinical scenario of prescribing MHT to women with a history of hysterectomy was found to be relatively rare – only 3% of respondents reported having undergone hysterectomy and could be candidates for estrogen monotherapy.
Moreover, according to Russian clinical guidelines, in cases of hysterectomy due to external genital endometriosis and/or adenomyosis, or supracervical uterine amputation, combined MHT is recommended in the absence of contraindications. Thus, in routine practice, physicians are most often required to select an individualized combined MHT regimen that includes both estrogen and progestogen components. Tailoring combined MHT to meet patient needs is a key factor in achieving optimal treatment outcomes for climacteric symptoms.
Among Russian women aged 45–59 who currently use MHT and are open to future hormone therapy, 67% preferred oral administration once daily. Only 9% were willing to consider transdermal gel as a treatment option.
Today, menopausal hormone therapy (MHT) is available in a variety of formulations, dosages, regimens, and routes of administration, all of which influence both therapeutic efficacy and safety. According to the 2024 draft of the clinical guidelines by the Russian Society of Obstetricians and Gynecologists (RSOG), MHT should be prescribed following established algorithms for peri- and postmenopausal women [4,10]. Oral MHT has demonstrated effectiveness in alleviating climacteric symptoms, improving metabolic health, and reducing all-cause mortality by 31%, offering a potential solution to the social and economic challenges associated with menopause [4,7,22]. The combination of estradiol and dydrogesterone has been shown to meet the criteria for efficacy, safety, and tolerability in high-quality randomized clinical trials [23–27].
Educational initiatives on menopause and symptom management are essential for both women and healthcare providers. Motivational counseling forms the foundation of long-term, effective collaboration between physician and patient. A thorough consultation with clarifying questions helps build trust and improve understanding of the condition and its treatment options. It is crucial to shape a positive and evidence-based perception of menopause and MHT among physicians. A gynecologist’s personal bias against MHT may be projected onto patients, discouraging them from starting therapy. Therefore, continuing medical education is needed to update gynecologists on modern principles of MHT, including treatment duration, risks, contraindications, and indications.
In this context, the development of clear algorithms for prescribing various MHT formulations and managing potential side effects is highly relevant. The Russian Society for Menopause and Midlife Health (ROSHEM) has been actively working on this in recent years.
In 2021 and 2023, additional key documents were introduced to support MHT use in real-world clinical practice in Russia [9,10]. A group of national medical societies (RSOG, ROSHEM, the Association of Gynecological Endocrinologists) developed the “Algorithms for MHT Use in Peri- and Postmenopausal Women” (2021), which provides step-by-step guidance on initiating therapy, adjusting regimens and dosages, and managing adverse effects [9].
In 2023, the “Russian Criteria for Acceptability of MHT Prescription” were published. This consensus document, developed by five leading professional societies – the Russian Society of Cardiology, RSOG, Russian Association of Endocrinologists, Eurasian Association of Therapists, and the Russian Phlebology Association – summarizes all currently available clinical evidence and outlines criteria for prescribing MHT to women with cardiovascular and metabolic comorbidities. Experts in cardiology, endocrinology, and internal medicine emphasized that MHT remains the most effective treatment for climacteric symptoms. The presence of cardiovascular or metabolic disease does not preclude MHT use, provided there are no contraindications [9].
Sharing positive experiences of current MHT users is also important. According to the authors, such information is especially valuable for younger women in the menopausal transition and for those experiencing severe symptoms. To improve patient adherence, efforts should be made to promote MHT, highlight its health and quality-of-life benefits, and dispel myths and misconceptions about associated risks. Personalized therapy that considers individual needs and preferences is a key component of maintaining well-being in the postmenopausal period.
Conclusion
Menopause has a significant impact on women’s health and quality of life. Although the rate of menopausal hormone therapy (MHT) use in Russia has increased from 1.3% to 6.5%, it remains substantially lower than in European countries. This gap is largely attributed to limited patient awareness about menopause and available treatment options, as well as insufficient physician training in the appropriate use of MHT.
Gynecologists and related specialists should pay greater attention to women over the age of 45 to ensure timely identification and management of menopausal disorders. To improve adherence to therapy among both patients and healthcare providers, educational initiatives are needed to raise awareness about menopause, its symptoms, potential long-term health consequences, and current evidence regarding the safety and benefits of MHT.
It is essential to develop comprehensive public health strategies aimed at optimizing the quality and longevity of life for women in the peri- and postmenopausal stages. Scientifically grounded information and thorough, personalized consultations on topics relevant to each woman can support informed decision-making between physician and patient regarding appropriate treatment approaches.
____________________
1Ratings of 8, 9, and 10 on a 10-point scale were interpreted as indicating a high level of negative impact, where 1 corresponds to “Minimal negative impact” and 10 to “Maximum negative impact.”
2Agreement levels were assessed using a 5-point scale, where 1 means “Strongly disagree” and 5 means “Strongly agree.” Responses of 4 and 5 were considered indicative of agreement.
3Effectiveness of symptom relief was evaluated using a 10-point scale, where 1 indicates “Does not relieve menopausal symptoms at all” and 10 indicates “Fully relieves menopausal symptoms.” Fully effective (8–10/10), Moderately effective (4–7/10), Poorly effective (1–3/10).
4Improvement in quality of life was assessed using a 10-point scale, where 1 means “Minimal improvement” and 10 means “Significant improvement compared to pre-MHT.”
5Satisfaction with therapy was measured using a 10-point scale, where 1 means “Not satisfied at all” and 10 means “Completely satisfied.” Ratings of 8, 9, and 10 were considered high satisfaction.
References
- Panay N., Ang S.B., Cheshire R., Goldstein S.R., Maki P., Nappi R.E. Menopause and MHT in 2024: addressing the key controversies – an International Menopause Society White Paper. Climacteric. 2024; 27(5): 441-57. https://dx.doi.org/10.1080/13697137.2024.2394950
- https://www.worldometers.info/demographics/world-demographics/(Accessed 20 Jan 2021).
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Менопауза и климактерическое состояние у женщины. М.; 2024. [Ministry of Health of the Russian Federation. Clinical guidelines. Menopause and menopausal symptoms in women. Moscow; 2024 (in Russian)].
- Steiner B.M., Berry D.C. The regulation of adipose tissue health by estrogens. Front. Endocrinol. (Lausanne). 2022; 13: 889923. https://dx.doi.org/10.3389/fendo.2022.889923
- Li M., Zhu Y., Wei J., Chen L., Chen S., Lai D. The global prevalence of premature ovarian insufficiency: a systematic review and meta-analysis. Climacteric. 2023; 26(2): 95-102. https://dx.doi.org/10.1080/13697137.2022.2153033
- Santoro N., Roeca C., Peters B.A., Neal-Perry G. The menopause transition: signs, symptoms, and management options. J. Clin. Endocrinol. Metab. 2021; 106(1): 1-15. https://dx.doi.org/10.1210/clinem/dgaa764
- The 2022 hormone therapy position statement of the North American Menopause Society. Menopause. 2022; 29(7): 767-94. https://dx.doi.org/10.1097/GME.0000000000002028
- Ламбриноудаки И., Армени Э., Гулис Д., Бретц С., Чаусу И., Дурмусоглу Ф., Эрккола Р., Фистонич И., Гамбаччани М., Геукес М., Хамода Х., Хартли К., Хиршберг А.Л., Мечекальски Б., Мендоса Н., Муек А., Сметник А., Штуте П., ван Троценбург М., Рис М. Согласованное заявление Европейского общества по менопаузе и андропаузе: менопауза, благосостояние и здоровье – принципы ведения пациенток. Акушерство и гинекология: новости, мнения, обучение. 2023; 11 Спецвыпуск: 151-68. [Lambrinoudaki I., Armeni E., Goulis D., Bretz S., Ceausu I., Durmusoglu F., Erkkola R., Fistonic I., Gambacciani M., Geukes M., Hamoda H., Hartley C., Hirschberg A.L., Meczekalski B., Mendoza N., Mueck A., Smetnik A., Stute P., van Trotsenburg M., Rees M. EMAS Consensus Statement Menopause, wellbeing and health: a care pathway from the European Menopause and Andropause Society. Obstetrics and Gynecology: News, Opinions, Training. 2023; 11 Special Issue: 151-68 (in Russian)].
- Шляхто Е.В., Сухих Г.Т., Серов В.Н., Дедов И.И., Арутюнов Г.П., Сучков И.А. Российские критерии приемлемости назначения менопаузальной гормональной терапии пациенткам с сердечно-сосудистыми и метаболическими заболеваниями. Согласительный документ Российского кардиологического общества, Российского общества акушеров-гинекологов, Российской ассоциации эндокринологов, Евразийской ассоциации терапевтов, Ассоциации флебологов России. Акушерство и гинекология. 2023; 11: 211-32. [Shlyakhto E.V., Sukhikh G.T., Serov V.N., Dedov I.I., Arutyunov G.P., Suchkov I.A. Russian eligibility criteria for menopausal hormone therapy in patients with cardiovascular and metabolic diseases. Consensus document of the Russian Society of Cardiology, Russian Society of Obstetricians and Gynecologists, Russian Association of Endocrinologists, Eurasian Association of Therapists, Russian Phlebological Association. Obstetrics and Gynecology. 2023; (11): 211-32 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.267
- Ашрафян Л.А., Балан В.Е., Баранов И.И., Белая Ж.Е., Бобров С.А., Воронцова А.В., Дубровина С.О., Зазерская И.Е., Иловайская И.А., Карахалис Л.Ю., Лесняк О.М., Мазитова М.И., Подзолкова Н.М., Протасова А.Э., Серов В.Н., Сметник А.А., Сотникова Л.С., Ульрих Е.А., Чернуха Г.Е., Юренева С.В.. Алгоритмы применения менопаузальной гормональной терапии у женщин в период пери- и постменопаузы. Совместная позиция экспертов РОАГ, РАМ, АГЭ, РАОП. Акушерство и гинекология. 2021; 3: 210-21. [Ashrafyan L.A., Balan V.E., Baranov I.I., Belaya Zh.E, Bobrov S.A., Vorontsova A.V., Dubrovina S.O., Zazerskaya I.E., Ilovayskaya I.A., Karakhalis L.Yu., Lesnyak O.M., Mazitova M.I., Podzolkova N.M., Protasova A.E., Serov V.N., Smetnik A.A., Sotnikova L.S., Ulrikh E.A., Chernukha G.E., Yureneva S.V. Algorithms for menopausal hormone therapy during the period of peri- and postmenopause. Joint position statement of RSOG RAM, AGE, RAOP experts. Obstetrics and Gynecology. 2021; (3): 210-21 (in Russian)]. https://dx.doi.org/10.18565/aig.2021.3.210-221
- Улумбекова Г.Э., Худова И.Ю. Оценка демографического, социального и экономического эффекта при приеме менопаузальной гормональной терапии. ОРГЗДРАВ: новости, мнения, обучение. Вестник ВШОУЗ. 2020; 4(6): 23-53. [Ulumbekova G.E., Khudova I.Yu. Demographic, social and economic effects of menopause hormonal therapy. Healthcare Management: news, views, education. Bulletin of VSHOUZ. 2020; 4(6): 23-53 (in Russian)]. https://dx.doi.org/10.24411/2411-8621-2020-14002
- ACOG Practice Bulletin No. 141. Obstet. Gynecol. 2014; 123(1): 202-16. https://dx.doi.org/10.1097/01.AOG.0000441353.20693.78
- Stuenkel C.A., Davis S.R., Gompel A., Lumsden M.A., Murad M.H., Pinkerton J.V. et al. Treatment of symptoms of the menopause: an endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2015; 100(11): 3975-4011. https://dx.doi.org/10.1210/jc.2015-2236
- Cobin R.H., Goodman N.F. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on menopause – 2017 update. Endocr. Pract. 2017; 23(7): 869-80. https://dx.doi.org/10.4158/EP171828.PS
- De Melo Pompei L., Machado R.B., Osório Wender M.C., Fernandes C.E., eds. Consenso Brasileiro de Terapêutica Hormonal da Menopausa. São Paulo: Leitura Médica; 2018. Available at: https://www.pfizer.com.br/files/libbs-2018-sobrac-1.pdf
- National Institute for Health and Care Excellence. Menopause: diagnosis and management. Available at: https://www.nice.org.uk/guidance/ng23
- Meeta M., Digumarti L., Neelam A., Nirmala V., Rashmi S., Sonia M. Clinical practice guidelines on menopause: *an executive summary and recommendations. Journal of Mid-Life Health. 2020; 11(2): 55-95. https://dx.doi.org/10.4103/jmh.JMH_137_20
- Hamoda H., Panay N., Pedder H., Arya R., Savvas M. The British Menopause Society & Women's Health Concern 2020 recommendations on hormone replacement therapy in menopausal women. Post Reprod. Health. 2020; 26(4): 181-209. https://dx.doi.org/10.1177/2053369120957514
- Lambrinoudaki I., Armeni E., Goulis D., Bretz S., Ceausu I., Durmusoglu F. et al. Menopause, wellbeing and health: a care pathway from the European Menopause and Andropause Society. Maturitas. 2022; 163: 1-14. https://dx.doi.org/10.1016/j.maturitas.2022.04.008
- Menopause Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. [The 2023 Chinese menopause symptom management and menopausal hormone therapy guidelines]. Zhonghua Fu Chan Ke Za Zhi. 2023; 58(1): 4-21. (in Chinese). https://dx.doi.org/10.3760/cma.j.cn112141-20221118-00706.
- Genazzani A.R., Divakar H., Khadilkar S.S., Monteleone P., Evangelisti B., Galal A.F. et al. Counseling in menopausal women: how to address the benefits and risks of menopause hormone therapy. A FIGO position paper. Int. J. Gynaecol. Obstet. 2024; 164(2): 516-30. https://dx.doi.org/10.1002/ijgo.15278
- Manson J.E., Aragaki A.K., Rossouw J.E., Anderson G.L., Prentice R.L. , LaCroix A.Z. et al. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the women’s health initiative randomized trials. JAMA. 2017; 318(10): 927-38. https://dx.doi.org/10.1001/jama.2017.11217
- Stevenson J.C., Ren M., Kahler E., Nappi R.E., Tatarchuk T., Simoncini T. et al. Ultra-low dose estradiol and dydrogesterone for the treatment of menopausal symptoms in a pooled, multi-ethnic population. Maturitas. 2024; 190: 108117. https://dx.doi.org/10.1016/j.maturitas.2024.108117
- Ren M., Yu Q., Custodio M.G., Simoncini T., Nappi R.E., Tatarchuk T. et al. Low-dose and ultra-low-dose estradiol and dydrogesterone in postmenopause: an analysis by body mass index. Climacteric. 2025;28(1): 21-7. https://dx.doi.org/10.1080/13697137.2024.2418497
- Simoncini T., Ren M., Tatarchuk T., Kahler E., Yu Q., Stevenson J. et al. Impact of low and ultra-low dose estradiol and dydrogesterone on health-related quality of life of postmenopausal women: outcomes from two Phase 3 studies. Gynecological and Reproductive Endocrinology and Metabolism. 2024; 5(2): 74-9. https://dx.doi.org/10.53260/grem.245022
- Yu Q., Stevenson J.C., Tatarchuk T., Nappi R.E., Custodio M.G., Kahler E. et al. Ultra-low-dose estradiol and dydrogesterone for treatment of vasomotor symptoms in Europe and China. Climacteric. 2024; 27(5):494-500. https://dx.doi.org/10.1080/13697137.2024.2380364
- Tatarchuk T., Stevenson J.C., Yu Q., Kahler E., Custodio M.G., Ren M. et al. Ultra-low-dose continuous combined estradiol and dydrogesterone in postmenopausal women: a pooled safety and tolerability analysis. Gynecol. Endocrinol. 2024; 40(1): 2375577. https://dx.doi.org/10.1080/09513590.2024.2375577
Поступила 22.07.2025
Принята в печать 29.08.2025
About the Authors
Аntonina А. Smetnik, PhD, Head of the Department of Gynecological Endocrinology, Associate Professor at the Department of Obstetrics and Gynecology, Institute of Postgraduate Education, V.I. Kulakov National Medical Research Center for Obstetrics and Gynecology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4; President of the Russian Society of Specialists in Gynecological Endocrinology and Menopause (ROSGEM), +7(495)531-44-44, a_smetnik@oparina4.ru,https://orcid.org/0000-0002-0627-3902
Ilya A. Ivanov, PhD, Researcher, Department of Gynecological Endocrinology, V.I. Kulakov National Medical Research Center for Obstetrics and Gynecology,
Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4; Member of the Executive Committee of the Russian Society of Specialists in Gynecological Endocrinology and Menopause, +7(962)980-00-18, doctor.i.ivanov@yandex.ru https://orcid.org/0000-0003-0751-7566
Elena I. Ermakova, PhD, Senior Researcher, Department of Gynecological Endocrinology, V.I. Kulakov National Medical Research Center for Obstetrics and Gynecology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4; Vice President of the Russian Society of Specialists in Gynecological Endocrinology and Menopause, +7(916) 848-37-46, e_ermakova@oparina4.ru, https://orcid.org/0000-0002-6629-051X
Gyuzyal I. Tabeeva, PhD, Senior Researcher, Department of Gynecological Endocrinology, V.I. Kulakov National Medical Research Center for Obstetrics and Gynecology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4; Scientific Secretary of the Russian Society of Specialists in Gynecological Endocrinology and Menopause, +7(903)199-72-82, doctor.gtab@gmail.com, https://orcid.org/0000-0003-0206-5679