Antenatal and intrapartum periods in singleton pregnancy after assisted reproductive technology
Objective: To investigate the antenatal and intrapartum periods in singleton post-ART pregnancies according to the type of infertility and the method of assisted reproductive technology (ART).Kinsht D.A., Marinkin I.O., Soboleva M.K.
Materials and methods: The study group included 409 newborns from women with singleton post-ART pregnancy; all children were born from 2007 to 2017 at the Avicenna Medical Center (Novosibirsk). The control group consisted of 210 newborns from women with spontaneous pregnancy (SP) without a history of infertility, with equal gravidity and parity, and born in the same period. The study group was divided into 2 subgroups according to the predominant type of infertility and the ART method. Group I (n=205) consisted of women who conceived by IVF and predominantly had female causes of infertility in the parents' history. Group II (n=204) included women conceived by IVF+ICSI and mainly had male factor infertility. A retrospective analysis included outpatient and antenatal care cards of pregnant women and the developmental histories of the newborns. The main parameters of the health status were evaluated using clinical and anamnestic methods.
Results: Patients in in the post-ART group were more likely to have threatened miscarriage than those in the spontaneous pregnancy group, but only with the predominance of female causes of infertility (IVF group, OR=1.12). ART does not increase the risk of preterm labor and pathological conditions of the intrauterine fetus.
Conclusion: A personalized plan for antenatal care and childbirth in women with post-ART pregnancy should take into account the predominant type of infertility and the ART method.
Keywords
The birth of healthy offspring in infertile couples is the only convincing evidence of the effectiveness of infertility treatment [1, 2]. Advances in assisted reproductive technology (ART) and the variety of techniques aimed at conceiving singleton pregnancy have significantly improved perinatal outcomes [3–5] in post-ART pregnancy. As a result, infants born after ART do not differ from those conceived naturally in the main parameters [6, 7].
In evaluating the outcomes of post-ART pregnancy, more attention is now paid to factors related to not only to ART technologies but also to the reproductive and somatic health of the parents [8, 9]. In recent studies, infertility is considered a factor that may independently influence perinatal outcomes [10]. Since by the time of pregnancy, most parents have a mature reproductive age and a history of severe somatic diseases, doctors' concerns about the course of post-ART pregnancy, maternal and child health are well founded [11–15].
The high prevalence of infertility [16, 17] requires concurrent consideration of the factors associated with the health of parents and their children [18, 19], and continuing to search for optimal ways to improve the effectiveness of its treatment and management of post-ART pregnancy to obtain healthy offspring [20–22].
Given the prevalence of infertility and the increasing number of pregnancies conceived by ART, this study aimed to investigate antenatal and intrapartum periods in singleton post-ART pregnancies according to the type of infertility, somatic comorbidities, and ART method.
Materials and methods
The study analyzed the outpatient and antenatal care cards of pregnant women managed at the Avicenna Medical Center (Novosibirsk), the course of their post-ART pregnancies, pregnancy outcomes, and newborn development histories.
The retrospective analysis included all available medical records reflecting the process of treatment of parents, the course of post-ART pregnancy, and early neonatal health status. At all stages, of treatment was provided to ensure continuity of care from the moment of referral of parents with infertility to the clinic up to the birth of the child. Infertile couples were treated with different ART methods according to the underlying causes. Female infertility was usually treated by in vitro fertilization (IVF); as a result, 205 children were born, which constituted subgroup I. The ICSI (Intra-Cytoplasmic Sperm Injection) was used for predominantly male factor infertility, resulting in the birth of 204 children in subgroup II. The 210 children born of a spontaneous pregnancy, whose parents did not have a complicated reproductive history and whose gravidity and parity were equal, made up the control group (the children were randomly selected in proportion to the year of birth in the study group).
Inclusion criteria for the study group was completed singleton pregnancy between 2007 and 2017. Exclusion criteria were children from multifetal post-ART pregnancies and from singleton spontaneous pregnancies that occurred after parental infertility treatment without ART. All couples included in the study were metropolitan residents, without nutritional deficiencies and of a homogeneous social group, which allowed for a uniform assessment of most factors influencing perinatal outcomes. Clinical and anamnestic methods with evaluation of the main parameters of maternal and child health status were used. The first stage was a comparison between the groups with post-ART pregnancy and spontaneous pregnancy. The second stage was aimed at identifying the characteristics of the post-ART pregnancy and labor course according to the initial type of infertility and the ART method.
Statistical analysis
Statistical analysis was performed using Microsoft Excel spreadsheets and R software [23]. The distribution of continuous variables was tested for normality using the Kolmogorov-Smirnov test with Lilliefors correction. Since the continuous variables distribution, showed a nonnormal distribution they were reported as the median (Me) and interquartile range (Q1; Q3). The groups were compared using the Mann–Whitney test and Fisher's exact test; For contingency tables larger than 2×2, its asymptotic method was used [24]. A logistic regression model was used to identify factors associated with threatened miscarriage and fetal pathology. The first step of predictor selection involved univariate analysis; the second step involved a multivariate algorithm with stepwise variable selection. The quality of the constructed models was evaluated by the sensitivity and specificity, AUC, and the Hosmer–Lemeshow test.
The critical level of significance when testing statistical hypotheses was considered at p<0.05. (when the p-value was less than 0.001, p<0.001 was reported).
The study was reviewed and approved by the Research Ethics Committee of the Novosibirsk State Medical University (Ref. No: 39 of 29.12.2011).
Results
Analysis of medical history data showed that the age of women in the post-ART pregnancy group and the spontaneous pregnancy group was 34 (31; 37) and 28.5 (26; 31) years, respectively (p<0.001). There were significant differences in the proportions of comorbidities, the course of pregnancy, and the course of labor in women with post-ART pregnancy and spontaneous pregnancy (Table 1).
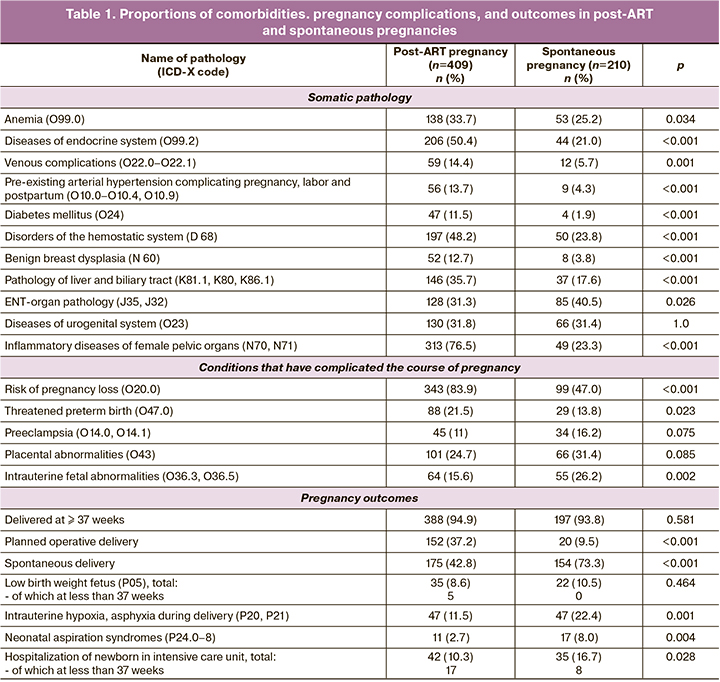
In the post-ART pregnancy group, a combination of pelvic inflammatory diseases was more common [103/409 (25.2%) vs 4/210 (1.9%) women in the spontaneous pregnancy group (p<0.001)], and microbial associations in chronic urogenital infection [130/409 (31.8%) women with post-ART pregnancy vs 32/210 (15.2%) in spontaneous pregnancy group (p<0.001)]. Threatened miscarriage during pregnancy was diagnosed more frequently in the post-ART pregnancy group [80/409 (19.6%) vs 16/210 (7.6%) women in the spontaneous pregnancy group (p<0.001)].
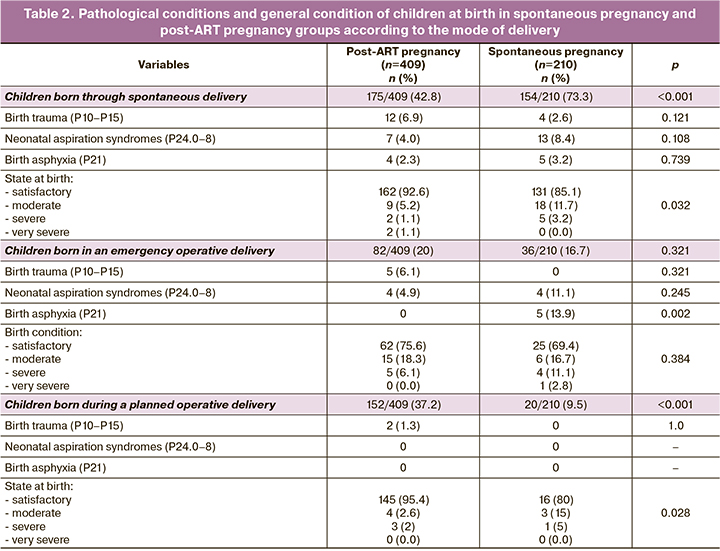
The primary plan of delivery was changed in favor of cesarean section due to emergency indications with a similar frequency in 82/409 (20%) women in the post-ART pregnancy group and in 36/210 (17.1%) women in the spontaneous pregnancy group (p=0.449). Acute intrauterine fetal hypoxia was detected less frequently in the post-ART pregnancy group in 20/409 (4.9%) cases and in 30/210 (14.3%) cases in the spontaneous pregnancy group (p<0.001). The delivery plan due to acute intrauterine hypoxia was changed in the 15/20 (75%) patients in post-ART pregnancy group and in 15/30 (50%) cases in the spontaneous pregnancy group (p=0.14). The predominance of elective operative delivery in the post-ART pregnancy group probably reduced the number of children born with asphyxia and aspiration syndromes compared to spontaneous pregnancy: 14/409 (3.4%) and 22/210 (10.5%) children, respectively (p<0.001). The data are presented in Table 2.
Certain features were also revealed in the study of somatic health, obstetric history, and the course of labor in women in the post-ART pregnancy group depending on the type of infertility and the ART method. The groups were comparable in terms of women's age [34 (31; 37) years in the IVF group and 35 (31; 39) years in the ICSI group, p=0.059)]. Women with different causes of infertility and ART methods had differences in somatic, obstetric history, and pregnancy course (Table 3).
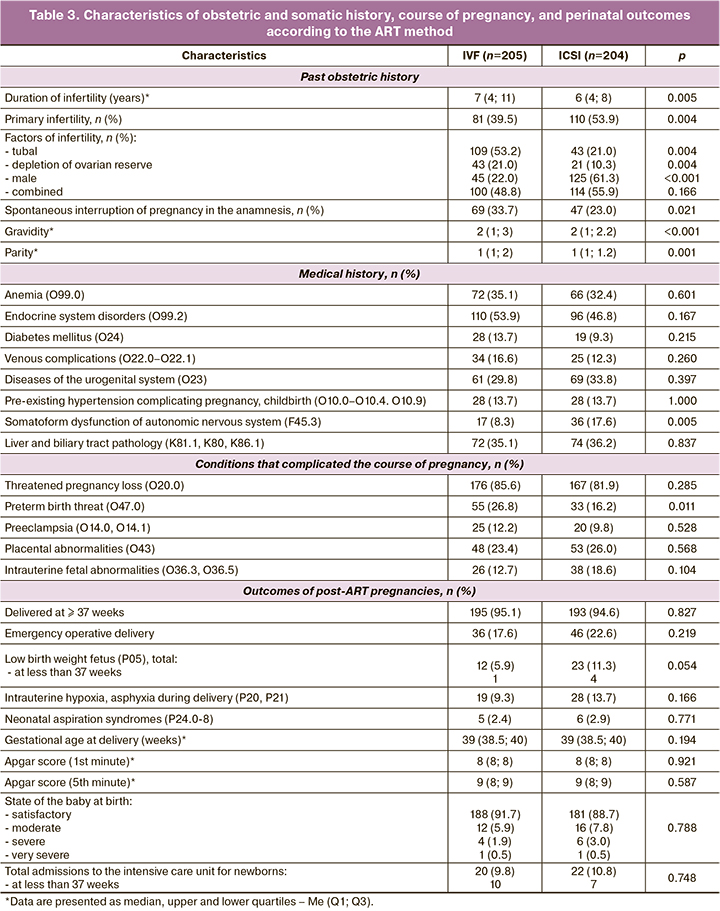
Inflammatory diseases of the female pelvic organs (N70, N71) and their combination were frequent in both groups [165/205 (80.5%) and 148/204 (72.5%)]. However, their combination was more common in the IVF group [66/205 (32.2%) vs 37/204 (18.1%) in the ICSI group (p=0.001)]. Vaginal dysbiotic processes also predominated in the IVF group [127/205 (61.9%) vs 62/204 (30.4%) in the ICSI group (p<0.001)].
Women in the IVF group were more likely to have threatened miscarriage during pregnancy [49/205 (23.9%) vs 31/204 (15.2%) women in the ICSI group (p=0.034)].
Taking into account the above comparisons, we searched for predictors of conditions that threaten maternal and child health, including threatened pregnancy loss and the pathological state of the fetus.
The multivariate logistic regression model identified the following predictors of pregnancy loss, adjusted for maternal age: type of ART, history of spontaneous miscarriage, myocardial pathology, and acute respiratory infections in the first trimester. Characteristics of the obtained model included AUC=0.67, sensitivity=0.67, and specificity=0.61. The obtained odds ratios (OR) characterize the risk of threatened miscarriage as follows (all other factors are equal):
- risk is 1.12-fold higher in the IVF group compared to spontaneous pregnancy [OR=1.12, confidence interval (CI) (1.03; 1.21)];
- risk was 1.03 times higher in the ICSI group [statistical significance level not reached, OR=1.03, CI (0.95; 1.11)];
- a history of spontaneous miscarriage increases the risk 1.15 times [OR=1.15, CI (1.05; 1.24)]
- the presence of myocardial pathology increases the risk 1.51 times [OR=1.51, CI (1.22; 1.86)];
- ARI in the first trimester increases risk by a factor of 1.11 [OR=1.11, CI (1.02; 1.21)].
For fetal pathological conditions, including acute and chronic hypoxia, growth and developmental delay, the following predictors were identified in the multivariate logistic regression model, adjusted for maternal age: type of ART, placental insufficiency, and number of previous births. Characteristics of the resulting model included AUC=0.81, sensitivity=0.66, and specificity=0.85. The obtained odds ratios (OR) characterize the risk of fetal abnormalities as follows:
- the risk is 0.93 times lower in the IVF group compared to spontaneous pregnancy [by 7%, OR=0.93, CI (0.87; 0.996)];
- risk is 0.996 times lower in the ICSI group compared to spontaneous pregnancy [statistical significance level not reached, OR=0.97, CI (0.90; 1.04)];
- placental insufficiency increases the risk by a factor of 1.46 [OR=1.46, CI (1.37; 1.56)];
- each previous birth in the patient reduces the risk by a factor of 0.94 [OR=0.94, CI (0.91; 0.99)].
In the group with the predominance of female causes of infertility (IVF), the risk of intrauterine pathological conditions (acute and chronic hypoxia, stunted growth and development) was lower by 7% compared to the spontaneous pregnancy group, probably in some cases due to elective surgical delivery. For the ICSI group, statistical significance was not reached.
Discussion
In this study, we compared prenatal factors associated with the initial reproductive health of the parents and maternal somatic health in single spontaneous and ART-induced pregnancies; we identified features of the course of post-ART pregnancy depending on the predominant infertility factors. These findings will allow consideration of the characteristics of the course of pregnancy and labor in decision making regarding a personalized treatment plan for women with post-ART pregnancy.
The results of the present study confirm the literature data that parents with a history of infertility have a mature reproductive age at the time of pregnancy, which is often associated with delay in healthcare-seeking [5, 13, 25]. According to our data, the duration of infertility was 7.2 (4; 10) years. Most of the children, 279/409 (68.2%), were born with five or more years of parental infertility. The duration of infertility in couples who had their first child born of their first pregnancy was 5 (4; 8.5) years, with a maximum of 20 years.
This is also responsible for the more complicated medical history of women in adulthood, which determines the development of complications of post-ART pregnancy. In post-ART pregnancy, women have a statistically significantly higher incidence of diseases and pathological conditions that can be the basis for infertility (endocrine system diseases, hemostasis system pathology, venous complications, arterial hypertension, diabetes mellitus, pelvic inflammatory diseases of female organs) and underlying pathology for the development of pregnancy complications, including preterm pregnancy loss. In the post-ART pregnancy group, compared to spontaneous pregnancy, threatened miscarriage and preterm birth were diagnosed more frequently, but only when female causes of infertility predominated (IVF group, OR=1.12). For the ICSI group with the predominance of male factors, the data were comparable to the spontaneous pregnancy group. Therefore, the predominance of male factor infertility that requires ICSI does not lead to an increased risk of loss of pregnancy.
No differences were found in the incidence of preeclampsia and placental abnormalities. The rate of intrauterine fetal pathological conditions was higher in the post-ART pregnancy group [OR=1.46, CI (1.37; 1.56)], which justifies choosing elective surgical delivery as first-line method in post-ART pregnancy. Comprehensive and interdisciplinary medical follow-up of post-ART pregnancy with timely detection and correction of emerging complications made it possible to complete post-ART pregnancy at gestational age comparable to spontaneous pregnancy. All babies in the singleton post-ART pregnancy group were born at gestational ages of 34 weeks or more. In spite of a more complicated parental history and higher rate of complications in post-ART pregnancy, the children were born mostly at full term and had similar characteristics to those of spontaneous pregnancies. The findings are inconsistent with studies that note an increase in the number of preterm births in any post-ART pregnancy, regardless of the type of infertility [16, 26].
The chosen delivery strategy for post-ART pregnancy (predominance of planned operative delivery and more frequent change of plan in favor of cesarean section due to emergency indications) reduces the number of babies born with neonatal aspiration syndromes and asphyxia. This also accounts for the higher number of babies born in satisfactory condition [369/409 (90.2%) vs 172/210 (81.9%) in spontaneous pregnancy, (p=0.005]. These data contradict the data of several studies in which babies from post-ART pregnancy are born in a more severe condition and have lower Apgar scores compared to babies from spontaneous pregnancy [2, 11].
In this study, women with different factors of infertility who underwent different ART methods were comparable in age [IVF group, 34 (31; 37) years; ICSI group, 35 (31; 39) years, (p=0.059]. There were no differences between the study groups in somatic pathology. But infertility and the problems of overcoming it affect the psycho-emotional state of women, which is confirmed by the literature data [27]. There is evidence of a higher prevalence of psycho-emotional disorders in women in the group with initially predominant male factor infertility (ICSI). Therefore, autonomic nervous system (F45.3) was diagnosed more frequently in this group compared to the IVF group (p=0.005). This factor should be considered in the treatment of infertility and in the preparation of women for ART programs.
There were also differences in the course of post-ART pregnancy depending on the causes of infertility in the parents' history and the selected ART method. In the IVF group, a long-lasting threat of preterm birth predominates (p<0.001), which agrees with the findings of a study that revealed an increased risk of preterm birth with the predominance of female causes of infertility [28]. Compensated forms of placental insufficiency were less common in the ICSI group, with no differences in placental abnormality rates depending on the type of infertility and ART methods. This is consistent with the data from several studies that did not reveal any association between placental abnormalities and the ART method [29, 30]. There were trends of fetal tolerance to labor in the ICSI group, but without statistical significance of differences: regardless of gestational age at the time of delivery, delivery plan was more often changed in favor of cesarean section surgery due to emergency indications and fewer children were born in satisfactory condition.
The existing unfavorable prenatal background in women with post-ART pregnancy has its own specific characteristics that affect the fetus in the antenatal and intrapartum periods and the condition of newborns. This determines the peculiarities not only in the choice of ART method, but also in antenatal care and labor management.
Conclusion
Any post-ART pregnancy is considered a high-risk pregnancy. However, the risks of preterm pregnancy loss and pathological fetal conditions include factors that do not depend on ART. Careful management of women in the context of specialized health care with sufficient experience with this category of patients allows prolongation of pregnancy and ensures the birth of children at full term, with the main characteristics at birth not differing from those of children in spontaneous pregnancy.
A personalized plan for antenatal care and childbirth in women with post-ART pregnancy should take into account the predominant type of infertility and the ART method. The risk of pregnancy loss is higher in couples with predominantly female causes of infertility (IVF). The predominance of male causes of infertility (ICSI) does not increase the risk of pregnancy termination; however, women in this group have a significantly higher incidence of autonomic somatoform dysfunction, which should be considered in the preparation for ART and in the treatment of pregnancy.
References
- Bhandari S., Ganguly I., Agarwal P., Munaganuru N., Gupta N., Singh A. Relationship of number of embryos transferred with perinatal outcome of singleton pregnancy. J. Reprod. Infertil. 2017; 18(1): 179-84.
- Пыхтина Л.А., Филькина О.М., Гаджимурадова Н.Д., Малышкина А.И., Назаров С.Б. Факторы риска и прогнозирование нарушений здоровья у детей первого года жизни, родившихся от одноплодной беременности после экстракорпорального оплодотворения. Анализ риска здоровью. 2017; 1: 55-65. [Pykhtina L.A., Filkina O.M., Gadzhimuradova N.D., Malyshkina A.I., Nazarov S.B. Risk factors and prediction of health disorders in children of the first year of life born from a singleton pregnancy after in vitro fertilization. Analiz riska zdorov'yu/Health risk analysis. 2017; 1: 55-65.(in Russian)]. https://dx.doi.org/10.21668/health.risk/2017.1.07.
- Регистр центров ВРТ России. Отчет за 2018 год. Российская Ассоциация Репродукции Человека. [Register of ART centers in Russia. Report for 2018. Russian Association of Human Reproduction. (in Russian)]. Available at:http://www.rahr.ru/d_registr_otchet/otchet2019.pdf
- Martin A.S., Chang J., Zhang Y., Kawwass J.F., Boulet S.L., McKane P. et al. Perinatal outcomes among singletons after assisted reproductive technology with single-embryo or double-embryo transfer versus no assisted reproductive technology. Fertil. Steril. 2017; 107(4): 954-60. https://dx.doi.org/10.1016/j.fertnstert.2017.01.024.
- Wyns C., Bergh C., Calhaz-Jorge C., De Geyter C., Kupka M.S., Motrenko T. et al. ART in Europe, 2016: results generated from European registries by ESHRE. Hum. Reprod. Open. 2020; 31(3): 1957-73. https://dx.doi.org/10.1093/hropen/hoaa032.
- Yeung E.H., Sundaram R., Bell E.M., Druschel C., Kus C., Xie Y. et al. Infertility treatment and children's longitudinal growth between birth and 3 years of age. Hum. Reprod. 2016; 31(7): 1621-8. https://dx.doi.org/10.1093/humrep/dew106.
- Bergh C., Wennerholm U.B. Long-term health of children conceived after assisted reproductive technology. Ups. J. Med. Sci. 2020; 125(2): 152-7.https://dx.doi.org/10.1080/03009734.2020.1729904.
- Berntsen S., Söderström-Anttila V., Wennerholm U.B., Laivuori H., Loft A., Oldereid N.B. et al. The health of children conceived by ART: 'the chicken or the egg?' Hum. Reprod. Update. 2019; 25(2): 137-58. https://dx.doi.org/10.1093/humupd/dmz001.
- Sun H., Liu Y., Huang S., Liu X., Li G., Du Q. Association between pre-pregnancy body mass index and maternal and neonatal outcomes of singleton pregnancies after assisted reproductive technology. Front. Endocrinol. (Lausanne). 2022; 12: 825336. https://dx.doi.org/10.3389/fendo.2021.825336.
- Sullivan-Pyke C.S., Senapati S., Mainigi M.A., Barnhart K.T. In vitro fertilization and adverse obstetric and perinatal outcomes. Semin. Perinatol. 2017; 41(6): 345-53. https://dx.doi.org/10.1053/j.semperi.2017.07.001.
- Баранов А.А., Намазова-Баранова Л.С., Беляева И.А., Бомбардирова Е.П., Смирнов И.Е. Медико-социальные проблемы вспомогательных репродуктивных технологий с позиции педиатрии. Вестник российской академии медицинских наук. 2015; 70(3): 307-14. [Baranov A.A., Namazova-Baranova L.S., Belyaeva I.A., Bombardirova E.P., Smirnov I.E. Medico-social problems of assisted reproductive technologies from the point of view of pediatrics. Vestnik rossijskoj akademii medicinskih nauk/Bulletin of the Russian Academy of Medical Sciences. 2015; 70(3): 307-14. (in Russian)].https://dx.doi.org/10.15690/vramn.v70i3.1326.
- Hwang S.S., Dukhovny D., Gopal D., Cabral H., Missmer S., Diop H. et al. Health of infants after ART-Treated, subfertile, and fertile deliveries. Pediatrics. 2018; 142(2): e20174069. https://dx.doi.org/10.1542/peds.2017-4069.
- Wennberg A.L., Opdahl S., Bergh C., Aaris Henningsen A.K., Gissler M., Romundstad L.B. et al. Effect of maternal age on maternal and neonatal outcomes after assisted reproductive technology. Fertil. Steril. 2016; 106(5): 1142-9. https://dx.doi.org/10.1016/j.fertnstert.2016.06.021.
- Kalayci H., Ozdemir H., Alkas D., Cok T., Tarim E. Is primiparity a risk factor for advanced maternal age pregnancies? J. Matern. Fetal Neonatal Med. 2017; 33(10): 1283-7. https://dx.doi.org/10.1080/14767058.2016.1211633.
- Pinheiro R.L., Areia A.L., Pinto A.M., Donato H. Advanced maternal age: adverse outcomes of pregnancy, A meta-analysis. Acta Med. Port. 2019; 32(3): 219-26. https://dx.doi.org/10.20344/amp.11057.
- Luke B. Pregnancy and birth outcomes in couples with infertility with and without assisted reproductive technology: with an emphasis on US population-based studies. Am. J. Obstet Gynecol. 2017; 217(3): 270-81.https://dx.doi.org/10.1016/j.ajog.2017.03.012.
- Fledderjohann J., Barnes L.W. Reimagining infertility: a critical examination of fertility norms, geopolitics and survey bias. Health Policy Plan. 2018; 33(1): 34-40. https://dx.doi.org/10.1093/heapol/czx148.
- Пыхтина Л.А., Филькина О.М., Гаджимурадова Н.Д., Маркова О.В. Прогнозирование наиболее частых нарушений здоровья у детей от одноплодной беременности после ЭКО. Российский вестник перинатологии и педиатрии. 2016; 61(4): 166. [Pykhtina L.A., Filkina O.M., Gadzhimuradova N.D., Markova O.V. Predicting the most common health disorders in children from singleton pregnancies after IVF. Russian Bulletin of Perinatology and Pediatrics. 2016; 61(4): 166. (in Russian)].
- Мурзаханова А.Ф., Ослопов В.Н., Хазова Е.В. Состояние здоровья детей, рожденных после экстракорпорального оплодотворения: вероятные риски и возможные осложнения. Практическая медицина. 2020; 18(3): 43-50. [Murzakhanova A.F., Oslopov V.N., Khazova E.V. The state of health of children born after in vitro fertilization: probable risks and possible complications. Practical medicine. 2020; 18(3): 43-50. (in Russian)].https://dx.doi.org/10.32000/2072-1757-2020-3-43-50.
- Qin J., Liu X., Sheng X., Wang H., Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil. Steril. 2016; 105(1): 73-85. https://dx.doi.org/10.1016/j.fertnstert.2015.09.007.
- Stern J.E., Liu C.L., Cabral H.J., Richards E.G., CoddingtonC.C., Hwang S. et al. Birth outcomes of singleton vaginal deliveries to ART-treated, subfertile, and fertile primiparous women. J. Assist. Reprod. Genet. 2018; 35(9): 1585-93. https://dx.doi.org/10.1007/s10815-018-1238-x.
- Velez M.P., Hamel C., Hutton B., Gaudet L., Walker M., Thuku M. et al. Care plans for women pregnant using assisted reproductive technologies: a systematic review. Reprod. Health. 2019; 16(1): 9. https://dx.doi.org/10.1186/s12978-019-0667-z.
- R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2022. Available at: https://www.R-project.org/
- Patefield W.M. Algorithm AS 159: An Efficient Method of Generating Random R × C Tables with Given Row and Column Totals. Appl. Stat. 1981; 30(1): 91-7.
- Bellver J., Donnez J. Introduction: infertility etiology and offspring health. Fertil. Steril. 2019; 111(6): 1033-5. https://dx.doi.org/10.1016/j.fertnstert.2019.04.043.
- Cavoretto P., Candiani M., Giorgione V., Inversetti A., Abu-Saba M.M., Tiberio F. et al. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: meta-analysis of cohort studies. Ultrasound Obstet. Gynecol. 2018; 51(1): 43-53. https://dx.doi.org/10.1002/uog.18930.
- Casu G., Zaia V., Montagna E., de Padua Serafim A., Bianco B., Parente C. et al. The infertility-related stress scale: validation of a brazilian-portuguese version and measurement invariance across Brazil and Italy. Front. Psychol. 2022; 12: 784222. https://dx.doi.org/10.3389/fpsyg.2021.784222.
- Sunkara S.K., Antonisamy B., Redla A.C., Kamath M.S. Female causes of infertility are associated with higher risk of preterm birth and low birth weight: analysis of 117 401 singleton live births following IVF. Hum. Reprod. 2021; 36(3): 676-82. https://dx.doi.org/10.1093/humrep/deaa283.
- Mortimer R., James K., Bormann C.L., Harris A.L., Yeh J., Toth T.L. et al. Male factor infertility and placental pathology in singleton live births conceived with in vitro fertilization. J. Assist. Reprod. Genet. 2021; 38(12): 3223-32.https://dx.doi.org/10.1007/s10815-021-02344-5.
- Stern J.E., Liu C.L., Hwang S.S., Dukhovny D., Farland L.V., Diop H. et al. Influence of placental abnormalities and pregnancy-induced hypertension in prematurity associated with various assisted reproductive technology techniques. J. Clin. Med. 2021; 10(8): 1681. https://dx.doi.org/10.3390/jcm10081681.
Received 21.04.2022
Accepted 08.08.2022
About the Authors
Darya A. Kinsht, Teaching Assistant at the Department of Pediatrics and Neonatology, Novosibirsk State Medical University, Ministry of Health of the Russian Federation, +7(913)-910-29-54, kinshtd@yandex.ru, https://orcid.org/0000-0001-6227-9893, 630099, Russia, Novosibirsk, Krasnyj prospect str., 52.Igor О. Marinkin, Dr. Med. Sci., Professor, Rector, Head of the Department of Obstetrics and Gynecology, Novosibirsk State Medical University, Ministry of Health of the Russian Federation, +7(383)222-22-04, rectorngmu@yandex.ru, https://orcid.org/0000-0002-9409-4823, 630099, Russia, Novosibirsk, Krasnyj prospect str., 52.
Мarya К. Soboleva, Dr. Med. Sci., Professor, Chair of Pediatrics of Medical Faculty, Novosibirsk State Medical University, Ministry of Health of the Russian Federation, +7(383)344-49-66, m.k.soboleva@gmail.com, https://orcid.org/0000-0003-2708-2264, 630099, Russia, Novosibirsk, Krasnyj prospect str., 52.
Corresponding author: Darya A. Kinsht, kinshtd@yandex.ru
Authors' contributions: Kinsht D.A. – review of the relevant literature, data analysis, manuscript drafting; Marinkin I.O. – design of the study, manuscript editing and publication approval; Soboleva M.K. – design of the study.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Novosibirsk State Medical University (Ref. No: 39 of 29.12.2011).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kinsht D.A., Marinkin I.O., Soboleva M.K. Antenatal and intrapartum periods
in singleton pregnancy after assisted reproductive technology.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 8: 63-70 (in Russian)
https://dx.doi.org/10.18565/aig.2022.8.63-70