Optimizing management strategy in women with pelvic varicose veins
Objective. To optimize management strategy in women with pelvic varicose veins (PVV).Gus A.I., Kolesnikova L.I., Semendyaev A.A., Stupin D.A., Shcherbatykh A.V., Kalyagin A.N., Chukhman A.V., Kolesnikov S.I.
Material and methods. The study comprised 74 women with grade I PVV, who underwent laparoscopic injection sclerotherapy (IST) of the refluxogenic pelvic veins. Depending on the type of additional therapeutic and preventive measures, the patients were divided into 3 study groups. Group 1 received IST followed by traditional conservative therapy with phlebotropic and disaggregant agents. Patients in group 2 underwent IST followed by a retrograde hemodynamic test (RHT) and postoperatively were given traditional therapy. Group 3was administered complex therapy, including a combination of IST and RGP followed by drugs with antioxidant and antiangiogenic therapeutic effects in combination with traditional therapy.
Results. The study findings showed that PVV recurrence rate, uterine pregnancy rate and quality of life were better in the patients in group 3.
Conclusion. The management of patients with PVV should include the following stages: 1- the combined use of IST and RHT; 2 - the use of drugs with antioxidant and antiangiogenic effects in combination with traditional therapy.
Keywords
Despite significant advances in surgical management of varicose veins, an estimated recurrence rate after previous surgery is 5–80% of cases [1-4], which is due to hidden (silent) sources of reflux blood flow and the absence of treatments aimed at some links of pathogenesis [5, 6].
Currently, the correction of venous outflow from the small pelvis in women with pelvic varicose veins (PVV) using endovascular techniques has an obvious advantage in comparison with other treatment modalities [7-10]. Occluding devices or agents (spirals, particles, balloons) and endovenous thermal obliteration (radiofrequency or laser) are used to block retrograde flow in the ovarian vein and its tributaries. However, these treatments are not always justified, because they can worsen the outflow from the pelvic venous bed and consequently promote the spread of local venous congestion from the ovarian vein pool to the adjacent venous plexuses and regional vascular network in general, causing damage to the blood vessels and pelvic tissues.
Besides, in this widely anastomosing regional venous network, the above procedures may be associated with technically difficult insertion of a catheter or guide-wire into the sources of reflux, located in the distal veins, as well as with the risk of perforation of the vascular wall. Occluding devices and agents may migrate into the renal veins or inferior vena cava, in the direction of the pulmonary blood flow.
Optimal treatment of PVV should involve the elimination of all sources of reflux flow in the pelvic venous bed. This problem can be solved if laparoscopic injection sclerotherapy (IST) for pelvic congestion is guided by a retrograde hemodynamic test (RHT). Also, the use of RHT during diagnostic laparoscopy may help identify hidden (silent) refluxogenic veins, clarify the location of pelvic varices and estimate the volume of IST (which is not possible using other diagnostic modalities), and intraoperatively identify defects of phlebosclerosis [11–13].
However, even with quality IST, the varicose disease may not be completely cured. Reasons for this include lipid peroxidation abnormalities and an increase in local angiogenic activity, which are linked to the pathogenesis of PVV [14].
Based on the above, this study aimed to optimize management strategy in women with PVV.
Material and methods
The study comprised 74 women with grade I PVV who underwent IST of the refluxogenic sites of the pelvic veins from 2009 to 2013. The severity of the disease was classified based on the results of the clinical and instrumental examination. Depending on the type of additional therapeutic and preventive measures, the patients were divided into 3 study groups: group 1 included 21 women who were administered traditional conservative treatment after IST, group 2 comprised 23 women who were given a combination of IST and RHT followed by traditional conservative treatment, and group 3was formed of 30 women receiving complex therapy including a combination of IST and RGP and drugs with antioxidant and antiangiogenic therapeutic effects in combination with traditional conservative treatment.
Grade 1PVV was diagnosed based on the following sonographic characteristics of the main trunk of the ovarian veins: internal diameter> 5.0 - ≤ 7.0 mm, linear blood flow velocity> 7.0 - ≤ 10.0 cm/sec, reflux duration> 0.3 - ≤ 1.5 sec; pelvic varicose veins were localized around the ovarian veins.
Clinical examination included the identification of clinical manifestations of PVV: pelvic pain, dysmenorrhea, dyspareunia, menorrhagia, and infertility. At baseline and every 3-6 months after IST, all patients underwent Duplex sonography with the determination of regional phlebohemodynamic parameters of the small pelvis using multi-frequency transducers (6 –12 MHz) and Voluson E10 ultrasound system (USA).
IST of refluxogenic zones and RHT were performed under 3D laparoscopic control using the Laser optic system (USA-Germany) and endoscopic equipment of the CooperSurgical (USA) and Karl Storz (Germany).
IST was used as a baseline PVV therapy. Sclerotherapy was performed using a 1–3% Aethoxysklerol, the volume of which was determined based on the volume of evacuated blood (from 0.5 to 2.0 ml) from the limited varicose vein area. The sclerosant volume can also be calculated using the formula for the volume of a cylinder: L (where r is the radius, L is the length of the sclerosed vein). To lower the concentration (to 0.5–1%) and reduce the dose (more than 4-fold) of the detergent, the foam-form technology was used. Improving the drainage of the pelvic vascular bed (obtaining a «dry» vessel) was achieved by placing the patient in the Trendelenburg position (lower body is raised to 15 degrees).
The indications for IST included ineffectiveness (maintaining stable venectasia) of traditional conservative treatment with the phlebotropic drug (detralex) and disaggregant (trental) in the standard therapeutic dosage: 500 mg once daily for 2 months and 100 mg 3 times daily for over 10 days, respectively. The course of treatment was repeated every 3-4 months.
Pathogenetic therapy of PVV included vitamin-mineral complex Vitrum-antioxidant with antioxidant effect and drugs with high antiangiogenic pharmacological activity, Indinol, and Epigallat, which were used in a standard therapeutic dosage: 1 tablet once daily for 3 months and 1 capsule twice daily for 2 months, respectively.
The mechanism of action of RHT involves two factors: the position of the patient on the operating table in the Fowler’s position (feet are lowered to 15 degrees) and the creation of a 2.5-liter pneumoperitoneum that is necessary for laparoscopy. These factors contributed to the additional inflow of venous blood from the upper abdominal cavity into the pelvis. If vein walls and the valvular apparatus of regional veins are incompetent, an additional blood flow increases intravascular pressure. With the inability of the vein wall to maintain hydrostatic pressure, the vein dilates, which leads to valve failure and blood reversal, which allows for accurate topical diagnosis of reflux blood flow foci - pathogenic factors of the progression of the pathological process, including «silent» zones, represented by «n» vessels, which appeared due to activation of angiogenesis.
To evaluate the effectiveness of PVV treatment and preventive measures in women, quality of life (QOL) was measured using the MOS SF-36 questionnaire, which was revised by including questions adapted to the specifics of the disease and reflected the following criteria: bodily pain, physical functioning, the perception of one’s own health, social functioning, the state of the menstrual cycle and reproductive function.
The patients’ responses were scored on a 10-point scale (from 0 to 10) and then summed up. The maximum score is 100, which corresponds to «complete health», 91–99 – «close to complete health», 71–90 – «good health», 51–70 – «satisfactory health», 0–50 – «poor health».
Statistical analysis was performed using the Statistica 6.1 statistical package (Stat-Soft Inc., USA; the license holder is the Scientific Centre for Family Health and Human Reproduction Problems). Differences between groups were assessed using Student’s t-test; the relationship between the variables was assessed with a Spearman correlation coefficient. Statistical significance was assumed for p < 0.05.
Results
Outcomes of the various treatments and preventive measures for PVV patients were followed for three years from the time of IST in 68 (91.9%) of 74 women. Evaluation of the treatment results in the study groups was carried out according to the following criteria: recurrence rate (the resumption of the clinical manifestations of the disease and disorders of regional phlebohemodynamics), the onset of uterine pregnancy, and the dynamics of the quality of life.
The results of the treatment in the study groups are summarized in the table.
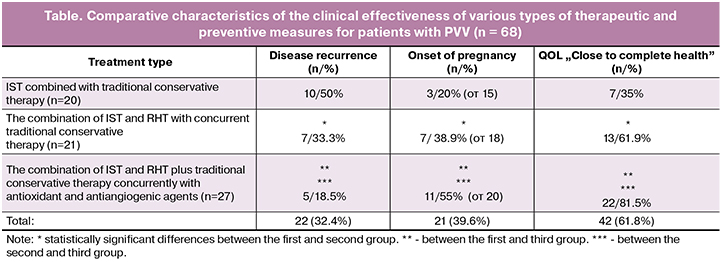
A comparative analysis of the studied parameters showed an obvious advantage of two-stage complex therapy for patients with the PVV. At the first stage, endoscopic RHT was performed to identify the sources of reflux blood flow, assess the degree of varicose vein expansion and determine the scope of sclerotherapy. After that, the IST of reflux sources was carried out, and the RHT was repeated to assess the adequacy of sclerotherapy. At the second stage, patients with PVV received drugs with antioxidant and antiangiogenic therapeutic effects in combination with traditional conservative treatment.
Comparative analysis of the treatment results of the PVV patients, depending on the treatment and preventive measure types, made it possible to establish the following patterns: the total recurrence rate in the late postoperative period was 32.4%. Recurrence rates after IST with traditional conservative treatment, after the combined use of IST and RHT with traditional conservative treatment, and after complex therapy, which included the combined use of IST and RHT with concurrent use of drugs with a targeted antioxidant and antiangiogenic therapeutic effects in combination with traditional conservative treatment were 50%, 33.3%, and 18.5%, respectively.
Analysis of the diagram (Fig. 1) indicates a significant difference (p <0.05) in the recurrence rates between the study groups after 12 months of follow-up. Between 12 and 36 months after sclerotherapy in group 1, recurrences were observed in1 (5%), 3 (15%), 5 (25%), 8 (40%), and 10 (50%) patients after 12, 18, 24, and 30 months, respectively. For similar periods in group 2, recurrences were observed in 2 (9.5%), 4 (19%), and 7 (33.3%) patients after 24, 30, and 36 months, respectively. Among the patients of group 3, these figures were 1 (3.7%), 3 (11.1%), and 5 (18.5%) after 24, 30, and 36 months, respectively. Moreover, there was a statistically significant difference (p <0.05) between the study groups during the analyzed periods.
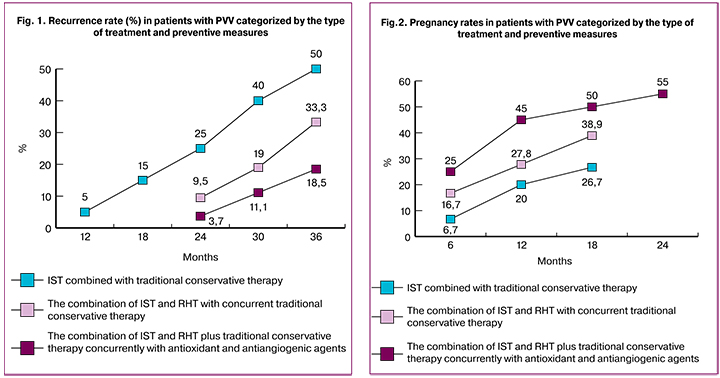
By the end of the 3-year follow-up, 22 of 53 patients with PVV became pregnant. Of them, 26.7%, 38.9%, 55%. Among women receiving IST with traditional conservative treatment (n = 15), combined use of IST and RHT with traditional conservative treatment (n = 18), and the combined use of IST and RHT concurrently with drugs with a targeted antioxidant and antiangiogenic therapeutic effects in combination with traditional conservative treatment (n = 20), pregnancy onset was registered in 26.7%, 38.9%, and 55%, respectively.
A significant difference in pregnancy rates between the study groups undergoing different treatments and preventive measures was observed between 6-month and 2-year follow-up (Fig. 2).
Changes in QOL in patients with PVV categorized by the type of treatment and preventive measures are presented in Figure 3.
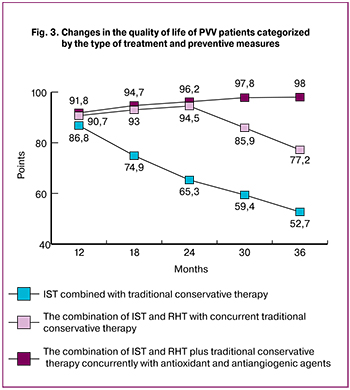 In all groups of patients with PVV, during the first year of observation, there was a progressive increase in QOL regardless of the type of therapy. The diagram (Fig. 3) shows the change in QOL scores in the study groups between 12 and 36 months after IST.
In all groups of patients with PVV, during the first year of observation, there was a progressive increase in QOL regardless of the type of therapy. The diagram (Fig. 3) shows the change in QOL scores in the study groups between 12 and 36 months after IST.
In the group of women who received IST and subsequently received several courses of traditional conservative therapy, the QOL scores reached 80–90 (mean 86.8) by the first year, remained at this level for a short time and began to rapidly decline to 50–70 (mean 52.7) 1.5 years after IST, which corresponded to the baseline findings.
In the group of women who received a combination of IST and RHT with traditional conservative therapy, QOL tended to increase even 1.5 years after the operation, reaching a maximum score of 94.5 by 24 months, with a gradual decrease to 68.5 points by the 3rd year.
In the group of women, who received the combination of IST and RHT concurrently with drugs with targeted antioxidant and antiangiogenic therapeutic effects in combination with traditional conservative treatment, QOL tended to increase even after 2.5 years of follow-up, reaching a maximum score of 95 by the 3d year, which indicated a persistent clinical effect of the therapeutic and prophylactic measures.
Thus, the complex management of patients with PVV has significantly improved the studied parameters, which indicates the optimal use of therapeutic and preventive measures. Traditional treatment of women suffering from PVV should also include IST and RHT with concurrent use of antioxidant and antiangiogenic drugs, which can be viewed as pathogenetically substantiated.
Discussion
To date, the question of the effectiveness of PVV treatment aimed to eliminate pelvic congestion using occlusion and thermal destruction remains open [6]. To achieve an adequate therapeutic effect, it is necessary to remove all sources of reflux blood flow in the pelvis [15, 16]. In our opinion, the management of PVV, especially with an extensive varicose veins, should include the combined use of RHT and IST guided by 3D endoscopy that allows precise topical diagnosis of the refluxogenic zones, clarify the degree of varices expansion, eliminate the refluxogenic zones, assess the result of IST, and timely detect and eliminate defects of sclerotherapy [11-13].
The clinical effectiveness of the combined use of IST and RHT concurrently with adjuvant therapy in the late postoperative period may be insufficient due to the persistence of the mechanisms that initiate the progression of the pathological process. Studies of lipid peroxidation and angiogenic activity under various conditions [15, 16] have resulted in the development of treatments that normalize the processes of lipid peroxidation and local angiogenic status in patients with PVV [14]. However, the combined use of IST, RHT, antioxidants and antiangiogenic therapy concurrently with traditional conservative treatment has been scarcely investigated.
The assessment of the clinical effectiveness of various types of treatment and preventive measures in patients with PVV within three years after IST showed a significant difference in the studied parameters when using complex therapy, in comparison with other types of rehabilitation. The obtained results suggest the high effectiveness of the combined use of IST and RHT concurrently with drugs with antioxidant and antiangiogenic pharmacological activity, the use of which can be considered pathogenetically justified.
Conclusion
The findings of our study suggest that the management of patients with PVV should include the following stages: 1. The combined use of IST and RHT to eliminate the sources of reflux blood flow as a factor initiating the progression of the pathological process; 2. The use of therapeutic agents aimed at normalizing the impaired lipid peroxidation and angiogenic status. These measures help restore reproductive function, improve QOL and reduce the recurrence rates in patients with PVV.
References
- Kistner R.L.., Eklöf B. Classification and etiology of chronic venous disease. In: Gloviczki P., ed. Handbook of venous disorders. 3rd ed. London: Hodder Arnold; 2009: 37-46.
- Daniels J.P., Champaneria R., Shah L., Gupta J.K., Birch J., Moss J.G. Effectiveness of embolization or sclerotherapy of pelvic veins for reducing chronic pelvic pain: a systematic review. J. Vasc. Interv. Radiol. 2016; 27(10): 1478-86. e8. https://dx.doi.org/10.1016/j.jvir.2016.04.016
- Лахно И.В. Ведение пациенток гинекологического профиля с варикозной болезнью. Здоровье женщины. 2017; 2: 103-5. [Lakhno IV. The management of gynecological patients with varicose veins disease. Zdorov_e zhenshchiny. 2017;(2):103−105. (in Russian)].
- Гус А.И., Семендяев А.А., Ступин Д.А., Бачурина С.М., Черепанова М.А. Значение перекисного окисления липидов в развитии варикозной болезни вен малого таза у женщин.Сибирский медицинский журнал (Иркутск). 2015; 133(2): 122-5. Gus A.I., Semendyayev A.A., Stupin D.A., Bachurina S.M., Cherepanova M.A. The significance of lipid peroxidation in the development of pelvic varicose veins in women. Siberian Medical Journal (Irkutsk). 2015; 133 (2): 122-5.(in Russian)].
- Фомин В.С., Фомина М.Н. Варикозное расширение вен малого таза как причина синдрома хронических тазовых болей: взгляд на проблему. Фарматека. 2017; 18: 14-9. [Fomin VS, Fomina MN. Pelvic varicies as a cause of the syndrome of chronic pain. Pharmateca. 2017;(18):14−19. (in Russian)].
- Богачев В.Ю., Стойко Ю.М., Гаврилов С.Г., Золотухин И.А., Кириенко А.И. Варикозная болезнь. В кн.: Савельев В.С., Кириенко А.И., ред. Сосудистая хирургия. Национальное руководство. М.: ГЭОТАР-Медиа; 2014: 405-38. [Bogachev V.Yu., Stoyko Yu.M., Gavrilov SG, Zolotukhin IA, Kirienko A.I. Varicose veins In the book: Saveliev, VS, Kirienko, AI, ed. Vascular surgery. National leadership. M .: GEOTAR-Media; 2014: 405-38. (in Russian)].
- Khatri G., Khan A., Raval G., Chhabra A. Diagnostic evaluation of chronic pelvic pain. Phys. Med. Rehabil. Clin. North Am. 2017; 28(3): 477-500. 10.1016/j.pmr.2017.03.004.
- Патент на изобретение № 26465, Российская Федерация. Cпособ определения функционального состояния венозной системы малого таза у женщин. А.А.Семендяев, Д.А.Ступин, М.А.Черепанова, В.М. Бачурина, А.Н.Селецкий, Л.И.Колесникова. Заявлено 20.06.2016; опубл. 5.03.2018. Бюл. № 7. [Patent for invention No. 26465, Russian Federation. Method for determining the functional state of the pelvic venous system in women. A.A. Semendyaev, D.A. Stupin, M.A. Cherepanova, V.M. Bachurin, A.N. Seletsky, L.I. Kolesnikova. Stated 20.06.2016; publ. 03/05/2018. Bul No. 7. (in Russian)].
- Патент на изобретение № 2295301, Российская Федерация. Способ лечения тазовой боли при варикозном расширении придатков матки. Н.В.Протопопова, А.С.Коган, А.А.Семендяев, В.В.Бочков, М.А. Семендяева. Заявлено 31.01.2006; опубл. 20.03.2007. [Patent for invention No. 2295301, Russian Federation. A method for the treatment of pelvic pain with varicose expansion of the uterus. N.V.Protopopova, A.S.Kogan, A.A. Semendyaev, V.V. Bochkov, M.A. Semendyaeva. Declared Jan. 31, 2006; publ. 03/20/2007. (in Russian)].
- Патент на изобретение № 2665625, Российская Федерация. Способ лечения варикозной болезни вен малого таза у женщин. А.А. Семендяев, Д.А.Ступин, М.Черепанова, С.М. Бачурина, Л.И. Колесникова. Заявлено 06.23.2017; опубл. 09.03.2018. [Patent for invention No. 2665625, Russian Federation. A method for the treatment of varicose veins of the pelvis in women. A.A. Semendyaev, D.A.Stupin, M.Cherepanov, S.M. Bachurina, L.I. Kolesnikov. Stated 06.23.2017; publ. 03/09/2018. (in Russian)].
- Гус А.И., Семендяев А.А., Ступин Д.А.,Черепанова М.А., Бачурина С.М., Селецкий А.Н., Колесникова Л.И. Профилактика рецидива варикозной болезни вен малого таза у женщин. Акушерство и гинекология. 2016; 10: 103-8. [Gus A.I., Semendyaev A.A., Stupin D.A., Cherepanova M.A., Bachurina S.M., Seletsky A.N., Kolesnikova L.I. Prevention of reccurent varicose veins of the small pelvis in women. Akushersnvo i Ginekologiya/Obstetrics and Gynecology. 2016; 10: 103-106. (in Russian)].
- Гус А.И., Бачурина С.М., Хамошина М.Б., Семендяева М.А., Самчук П.М., Семендяев А.А. Алгоритм обследования женщин с синдромом тазовых болей при подозрении на варикозную болезнь вен малого таза. Сибирский медицинский журнал (Иркутск). 2011; 105(6): 83-5. [Gus A.I., Bachurina S.M., Khamoshina M.B., Semendyayeva M.A., Samchuk P.M., Semendyayev A.A. Algorithm for examining women with pelvic pain syndrome when a pelvic varicose vein is suspected. Siberian Medical Journal (Irkutsk). 2011; 105 (6): 83-5. (in Russian)].
- Бачурина С.М., Гус А.И., Хамошина М.Б., Семендяева М.А., Семендяев А.А., Самчук П.М. Тазовая боль, ассоциированная с бесплодием у женщин: Пути решения проблемы. Сибирский медицинский журнал (Иркутск). 2011; 105(6): 252-5. [Bachurina S.M., Gus A.I., Khamoshina M.B., Semendyayeva M.A., Semendyayev A.A., Samchuk P.M. Pelvic pain associated with infertility in women: Ways to solve the problem. Siberian Medical Journal (Irkutsk). 2011; 105 (6): 252-5. (in Russian)].
- Гус А.И., Хамошина М.Б., Черепанова М.А., Бачурина С.М., Семендяев А.А., Ступин Д.А. Диагностика и лечение варикозной болезни вен малого таза у женщин. Новосибирск: Наука; 2014. Gus A.I., Chamochina M.B., Cherepanova M.A., Bachurina S.M., Semendyaev A.A., Stupin D.A. Diagnostics and treatment pelvic varicose in women. Novosibirsk: Nauka; 2014,136 p (in Russian)].
- Колесникова Л.И., Колесников С.И., Даренская М.А., Гребенкина Л.А., Никитина О.А., Лазарева Л.М., Сутурина Л.В.. Данусевич И.Н., Дружинина Е.Б., Семендяев А.А. Активность процессов ПОЛ у женщин с синдромом поликистозных яичников и бесплодием. Бюллетень экспериментальной биологии и медицины. 2016; 162(9): 300-3. [Kolesnikova L.I., Kolesnikov S.I., Darenskaya M.A., Grebenkina L.A., Nikitina O.A., Lazareva L.M., Suturina L.V., Danusevich I.N., Druzhinina E.B., Semendyaev A.A. Activity of POL processes in women with polycystic ovary syndrome and infertility. Bulletin of experimental biology and medicine. 2016; 162 (9): 300-3. (in Russian)].
- Kolesnikova L.I., Kolesnikov S.I., Darenskaya M.A., Grebenkina L.A., Nikitina O.A., Lazareva L.M., Suturina L.V., Danusevich I.N., Druzhinina E.B., Semendyaev A.A. Activity of LPO processes in women with polycystic ovarian syndrome and infertility. Bull. Exp. Biol. Med. 2017;162(3): 320-2.
Received 14.06.2018
Accepted 22.06.2018
About the Authors
Gus, Alexander I., MD, Head of Functional Diagnostics at the Department of Diagnostic Imaging, National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. eLibrary SPIN code: 1464-2786Kolesnikova, Lubov I., MD, Academician of the RAS, Professor, Research Administrator at the Scientific Center for Problems of Family Health and Human Reproduction. 664003, Russia, Irkutsk, Timiryazev str. 16. Tel: +73952207367. E-mail: iphr@sbamsr.irk.ru. eLibrary SPIN code: 1584-0281 ORCID ID - 0000-0003-3354-2992
Semendyayev, Andrei A., MD, professor, Department of Obstetrics and Gynecology with the Course of Pediatric and Adolescent Gynecology,
Irkutsk State Medical University.
664003, Russia, Irkutsk, Krasnogo Vosstaniya str. 3. Tel.: +73952207367. Mobile: + 79148950592. E-mail: stupindima@rambler.ru.
eLibrary SPIN code: 3598-8817 ORCID ID - 0000-0002-4107-6285
Stupin, Dmitriy A., PhD, student, Scientific Center for Family Health and Human Reproduction; teaching assistant, Department of Obstetrics and Gynecology with the Course of Pediatric and Adolescent Gynecology, Irkutsk State Medical University.
664003, Russia, Irkutsk, Timiryazev str. 16. Tel.: +73952243825. Mobile: +79021782430. E-mail: stupindima@rambler.ru.
eLibrary SPIN-code: 6459-1703 ORCID ID - 0000-0002-0687-4804
Shcherbatykh, Andrey V., MD, professor, head of the Department of Surgery, Irkutsk State Medical University.
664003, Russia, Irkutsk, Krasnogo Vosstaniya str. 1. Tel.: +73952207367. Е-mail: stupindima@rambler.ru
eLibrary SPIN-code: 5056-2573 ORCID ID - 0000-0003-1990-1207
Kalyagin, Aleksey N., MD, professor, head of the Department of Propedeutics of Internal Diseases, Irkutsk State Medical University.
664003, Russia, Irkutsk, Krasnogo Vosstaniya str. 1. Tel.: +73952207367. Е-mail: akalagin@yandex.ru
eLibrary SPIN-code: 6737-0285 ORCID ID – 0000-0002-2708-3972
Chukhman, Andrei V., anesthesiologist of the Highest Qualification Category, Clinical Hospital at the Irkutsk-Passazhirskiy Railway Station of JSC RZD.
664005, Russia, Irkutsk, Botkina str. 10. Tel.: +73952638800. E-mail: referent_1@dkb.irk.ru
Kolesnikov, Sergey I., MD, professor, academician of the RAS, scientific secretary of the RAS, Scientific Center for Problems of Family Health and Human Reproduction. 664003, Russia, Irkutsk, Timiryazev str. 16. Tel: +73952207367. E-mail: iphr@sbamsr.irk.ru. eLibrary SPIN code: 1752-6695 ORCID ID - 0000-0003-2124-6328
For citation: Gus A.I., Kolesnikova L.I., Semendyaev A.A., Stupin D.A., Shcherbatykh A.V., Kalyagin A.N., Chukhman A.V., Kolesnikov S.I. Optimizing management strategy in women with pelvic varicose veins. Akusherstvo i Ginekologiya/Obstetrics and Gynecology.2019; (4): 58-64. (in Russian)
https://dx.doi.org/10.18565/aig.2019.4.58-64