Medical and social factors of infertility in Russia
Objective: Assessment of medical and social aspects of the prevalence and the structure of infertility causes in Russia.Korneeva I.Е., Nazarenko Т.А., Perminova S.G., Mityurina E.V., Cybizova T.I., Dashieva A.E.
Materials and methods: We used the data of questionnaire survey of 7004 infertile couples. The questionnaire included the questions about education, social and marital status, as well as information from medical documentation about the age, reproductive and medical history of partners. To perform comparative assessment of the studied characteristics, all participants of the study were divided into 2 groups, depending on the period of seeking treatment in fertility clinics. Group 1 consisted of 3509 couples who sought infertility treatment from January 1, 2010 to December 31, 2015. Group 2 comprised 3495 couples, who sought infertility treatment from January 1, 2016 to December 31, 2020.
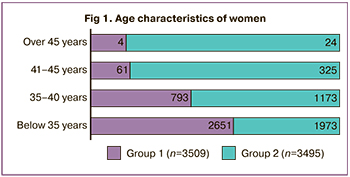
Results: Over the past 5 years, the age of infertile couples seeking treatment increased by 4 years on average and was 34 (4.8) years for women and 35.5 (5.9) years for men. At the same time, the proportion of women over 40 increased by 4 times. The proportion of rural residents increased. Introduction of the IVF program into Compulsory Medical Insurance (CMI) system has made it more accessible to a wide range of people with different incomes. The number of HIV-infected infertile couples planning treatment of infertility has increased.
Tubo-perioneal factor (24.2% and 23.5% in groups 1 and 2) ranked first as the only cause of infertility. The second most common factor of infertility was male infertility (17% and 19.4%). The third factor was endocrine origin of infertility (5.1% and 7.6%). Regardless of the estimated period of time, the combined types of infertility prevailed in the structure of infertility causes – 39.6% in group 1 and 39.5% in group 2.
Conclusion: The results of the study demonstrated the influence of medical and social factors on health-seeking behavior of patients with infertility, as well as the frequency of various causes of reproductive disorders.
Authors’ contributions: Korneeva I.Е., Nazarenko Т.А., Perminova S.G., Mityurina E.V., Cybizova T.I. – article editing and final approval; Dashieva A.E. – literature search and analysis, original data processing, article writing.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: The article was written without any sponsorship.
Ethical Approval: The study was approved by the local Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors’ Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Korneeva I.Е., Nazarenko Т.А., Perminova S.G., Mityurina E.V., Cybizova T.I., Dashieva A.E. Medical and social factors of infertility in Russia.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2023; (3): 65-72 (in Russian)
https://dx.doi.org/10.18565/aig.2022.279
Keywords
According to the World Health Organization (WHO), infertility is a disease of the reproductive system defined by the failure to achieve clinical pregnancy after 12 months of regular unprotected sexual intercourse due to a person’s inability to reproduce either individually, or both partners can’t reproduce [1, 2]. Infertility occurs due to various pathological processes in the reproductive system both in women and men. The diagnosis of the causes of infertility and treatment can be started earlier than 1 year, especially in women over 35 years old, based on medical and reproductive history, general examination and diagnostic tests [3].
The demographic indicators in Russia for the recent years are characterized by a stable negative population growth rate. Thus, according to the data of the Russian Federal State Statistics Service (Rosstat), in 2020, natural population decline was minus 6.1 per 1,000 population in the Central Federal District, and on the whole, minus 4.8 in the Russian Federation [4].
According to various estimates, 10–20% of the population of reproductive age is currently infertile in Russia, that is up to 5 million couples. At the same time, more than 70% of them have a combination of both female and male causes of infertility. The factors that influence the prevalence of infertility are woman's age, lifestyle, environment, sexually transmitted infections, medical abortions, as well as the quality of health care indirectly reflected in complications in the post- abortion and postpartum period [5].
Introduction of the IVF programs into Compulsory Medical Insurance (CMI) system in 2013 was a positive step taken by the government, that increased accessibility for infertility treatment and raised a sense of satisfaction in population. Nevertheless, lack of current objective data reflecting infertility problem in the country, namely the structure of the factors for infertility, the effectiveness of various diagnostics and therapeutic measures necessitate the need for further research in this field. The obtained information will make it possible not only to assess the quality of health care for infertile couples, but also to optimize the algorithms for medical examination and treatment tactics for this cohort of patients. Based on the data of age structure in infertile couples, prevalence of different factors for infertility, as well as treatment methods and their effectiveness, the system of health care for infertility can be improved and will contribute not only to increased number of wanted pregnancies and births, but also to a sense of patient satisfaction, as well as the rational use of the state funds.
According to the report of the Register of the Russian Association for Human Reproduction for 2020, 1 381 637 ART treatment cycles have been performed since 1995 in Russia. However, the increasing number of ART treatment cycles is accompanied not by increased number of pregnancies, but on the contrary, by their reduction, reflecting the trend to delayed child-bearing. Pregnancy rate per a cycle was 28.9% in 2020 (32.3% in 2019, 34.8% in 2016, 33.9% in 2015) [6]. Thus, according to monitoring specialists, in recent years, the women aged over 39 year increasingly frequently seek treatment in fertility clinics. This reflects worldwide tendency: the number of children born to a woman during her lifetime is decreasing, the number of women delaying their first child-bearing and nulliparous women is increasing. First of all, this phenomenon is based on social and economic reasons, due to the fact that since the 60s of the 20th century, motherhood has become a woman's personal choice. Education, profession, career were given first priority, and only then childbirth. Currently, the average age of a primiparous mother is 35 years and over [7].
However, deterioration of population health due to environmental changes, foods, high levels of distress leading to decline in fertility and to infertility appear to play an important role [8, 9].
Data review that was published in the domestic literature showed that there are few researches on the prevalence of infertility in different cities and regions of the Russian Federation (RF). The prevalence and infertility factors may have a specific regional character. This is very important in planning the activity of healthcare settings that provide fertility treatment for infertile couples. Thus, the study that was carried out by the group of authors from the Institute of Digital Medicine of I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the RF (Sechenov University), the Central Research Institute of Organization and Informatization of Healthcare of the Ministry of Health of the RF, the website UroWeb.ru and N.A. Lopatkin Research Institute of Urology and Interventional Radiology – the branch of the National Medical Research Radiologiсal Center of the Ministry of Health of the RF, showed that the total number of infertile men increased from 22348 to 47886 (+114%) in the period from 2000 to 2018. The number of patients with first diagnosed male infertility increased by 82%. The incidence of male infertility per 100,000 male population significantly differs in the regions of the Russian Federation. The highest number of infertile men was in the North Caucasian and Ural Federal Districts (FD), and 3 times exceeded the total number in Russia. In the Far Eastern FD, the prevalence of male infertility is almost 3 times lower than the average Russian indicators [10].
Currently, there are few researches devoted to the study of regional specific features of infertility in Russia. Due to this, it is impossible to answer exactly the the question about the prevalence and combination of major factors of infertility in different regions and FD of the country.
The objective of this study was assessment of medical and social aspects of the prevalence and the structure of infertility causes in Russia.
Materials and methods
A retrospective and prospective multicenter observational study was conducted. It was based on the data collected from the total of 7004 respondents, who sought fertility treatment in 17 medical clinics in 8 FD of Russia. For comparative analysis of study characteristics, all participants were divided into 2 groups depending on the period of seeking treatment in fertility clinics. Group 1 consisted of 3509 couples who underwent infertility treatment in the period from January 1, 2010 to December 31, 2015; group 2 comprised 3495 couples who underwent treatment from January 1, 2016 to December 31, 2020.
The sample size was determined using the Vaughan's formula (Vaughan and Morrow, 1989): n=p×(100-p)/(E/1,96)2, where n was a sample size, p signified the frequency of the studied characteristic (infertile couple) in percentage, E was a sampling bias (here 5%). The value of coefficient from table values was 1.96, and 95% confidence interval was used for assessment of the indicators. After substitution of the values into the formula, the equation was n=18×82/(5/1,96)2=227.
Thus, for comparative analysis of the obtained variables, it was necessary that there were 227 persons per each parameter in the comparison groups, namely in each FD per each studied parameter there was at least 227 respondents during the study period.
To maintain the statistical power of the study involving 16 medical centers in 8 FD of Russia, the study was performed taking into account retrospective data collection and possible data omission, the total number of participants at least 7000 persons, who were evenly distributed between the period 1 and period 2.
To achieve the objective, the questionnaire survey was conducted. The questionnaire contained the answers of the respondents to the questions about their education, social and marital status. Also, the information about age, reproductive and medical history of the partners was collected from their medical documentation.
The obtained data were entered into the electronic data base for statistical data processing.
Statistical analysis
Statistical analysis of the results of the study was performed in accordance with the methodological recommendations for assessment of the quality of statistical analysis in clinical studies. Regardless of the criterion type, the differences were considered to be statistically significant at р<0.05. Statistical software package R verson 3.x.x (A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria), and the version control package adapted and validated by Microsoft (Microsoft R Open. Microsoft and R Core Team. Microsoft, Redmond, Washington) were used in compliance with “A Guidance Document for the Use of R in Regulated Clinical Trial Environments”. The quantitative data were presented as mean with standard error of mean and standard deviation. For statistical analysis between the groups, the traditional approaches were used with choosing the null and alternative hypotheses, as well as the level of significance.
The study was conducted in accordance with the Federal Law No. 323-FZ of November 21, 2011 “On the basics of protecting the health of citizens in the Russian Federation, the National State Standard GOST R52379-2005 Good Clinical Practice, GCP), the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), the ethical principles of the Declaration of Helsinki (DoH) of the World Medical Association (last version) and all applicable local requirements (to the extent that the applicable law permits to conduct non-interventional observation studies). The study was approved by the Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation.
Results
The mean age of women in group 1 was 31 (4.2) years. Among the women who sought infertility treatment, 2651/3509 (75.5%) were aged below 35 years, 793/3509 (22.6%) were aged 35–40 years, 61/3509 (1.8%) were aged 41–45 years, and 4/3509 women (0.1%) were aged over 45 years. The mean age of women in group 2 was 34 (4.8) years. The data presented in Figure 1 demonstrate that in group 2, the number women aged 35–40 years increased by 2 times, 41–45 years – by 4 times, and over 45 years by 5 times. The mean age of male partners also increased: from 33.7 (6.1) years in group 1 to 35.5 (5.9) years in group 2.
The overwhelming majority of couples 3067/3509 (87.4%) and 2949/3495 (84.4%) in group 1 and 2, who sought treatment in fertility clinics were urban residents; 442/3509 (12.6%) and 546/3495 (16,6%) were rural residents. From 2016 to 2020 the proportion of rural residents who sought infertility treatment increased by 23.5%.
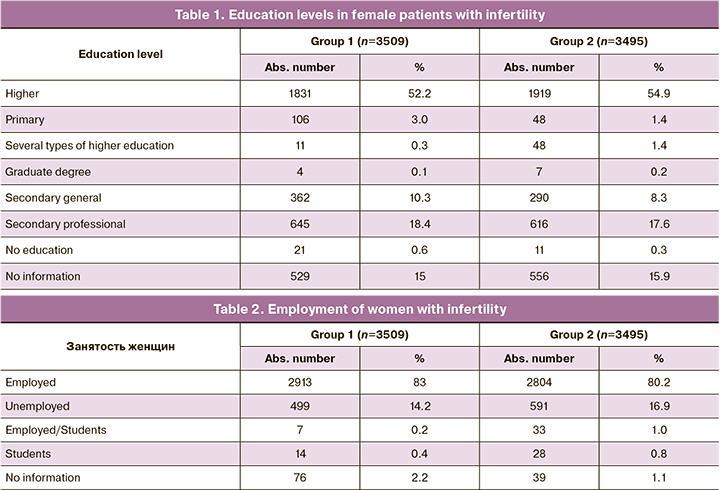
More than half of women in group 1 and 2 had higher education – 1831/3509 (52.2%) and 1919/3495 (54.9%), respectively; 645/3509 (18.4%) and 616/3495 (17.6%) women, respectively, had secondary vocational education. No information was obtained about education of 529/3509 (15%) and 556/3495 (15.9%) women (Table 1).
The mean age of tinitiation of sexual activity was 6 (3.4) years and 17.8 (4.3) years in group 1 and 2, respectively. The percentage of women using modern methods of contraception increased by 10.5% (from 634 to 701). The percentage of women having children was 13.7% (484/3509) in group 1, and 14.6% (512/3495) in group 2.
According to the opinion of 45.6% of respondents, the optimal age for the first childbirth was 21–25. The opinion of 41.3% of respondents regarding the age for the first childbirth was 26–30.
The data on marital status of infertile couples showed that 3055/3509 (87%) respondents in group 1 and 2918/3495 (83.6%) in group 2 were married couples; 397/3509 (11.3%) and 507/3495 (14,5%) were common law couples. In group 1, 55/3509 women (1.7%) were single, and 67/3495 (1.9%) women were single in group 2. Thus, the percentage of common law marriages increased by 3.2% in the period from 2016 to 2020.
At the time of seeking treatment in fertility clinics, the number of working women in group 1 was 2913/3509 (83%), and 2804/3495 (80.2%) working women were in group 2. Moreover, 82/3509 (2.3 %) patients in group 1 and 100/3495 (2.8%) in group 2 were occupied in hazardous industry. From 2016 to 2020, the number of unemployed women increased by 18.4% (from 499 to 591 women). The number of women, who combined work and study increased by 3 times, and the number of respondents who were students increased by 2 times (Table 2).
54.8% of respondents learned about infertility treatment using IVF from mass media, 33.2% of couples learned from the treating physician, and 11.7% from familiar persons. 0.15% of patients gave no answer to the question about the source of information.
It is of particular interest that more than half of women 3761/7004 (53.7%) participating in the study, responded that IVF could help to achieve pregnancy at any age.
Respondoing to the questionnaire regarding unhealthy lifestyle, 6975/7004 (99.6%) women gave a negative answer to the question about the use of narcotic drugs or psychotropic substances. 2 patients (0.38%) used narcotic drugs in the past. 147/7004 (2.1%) women were heavy smokers.
3/6871 (0.04%) men responded that they used narcotic drugs or psychotropic substances in the past; 6781/6871 (98.7%) men reported drinking alcohol sporadically; 563/6871 (82%) men were heavy smokers for about 9.5 years on average; 535/6871 (7.8%) men were engaged in hazardous occupations.
The data on blood-borne infections showed that from 2016 to 2020, the number of female carriers of hepatitis B antibodies increased from 32/3509 (0.9%) to 44/3495 (1.3%) women, while the frequency of hepatitis B antibodies in female carriers decreased from 60/3509 (1.7%) to 37/3495 (1.0%). The proportion of HIV-infected women increased from 3/3509 (0.08%) to 8/3495 (0.2%). 43/3509 (1.2%) women in group 1 and 32/3495 (0.9%) women in group 2 were seropositive for the presence of antibodies to Treponema Pallidum antigens.
The similar tendency was noted in male partners. From 2016 to 2020, the frequency of detection of hepatitis B antibodies increased from 0.8% (29/3455) to 1.2% (41/3416); the frequency of hepatitis B antibodies in male carriers decreased from 1.6% (55/3455) to 1.0% (33/3416); The percentage of HIV-infected male partners increased from 0.05% (2/3455) to 0.17% (6/3416). 1.2% (40/3455) of men in group 1 and 0.8% (27/3416) of men in group 2 were seropositive for the presence of antibodies to Treponema Pallidum antigens.
Almost half of the surveyed – 1645/3509 (46.9%) women in group 1 and 1596/3495 (45.6%) patients in group 2 reported past obstetric history. Only one third of pregnancies ended with birth in 484/3509 (29.4%) women in group 1 and 512/3495 (32%) in group 2. In both groups, 9% of women had complications in the post-abortion and postpartum periods.
The reasons for seeking treatment in IVF clinics were:
- inability to conceive naturally – 6715/7004 (95.9%) couples;
- previously performed gynecological surgery in history – 3474/7004 (49.6%) women;
- failed pregnancy in history – 2171/7004 (31.0%) women;
- no sexual partner – 133/7004 (1.9%) women.
The average duration of infertility at the time when the couples sought treatment in fertility clinics was 4.04 (0.6) years in group 1 and 4.6 (1.2) years in group 2. Only 53 couples (0.7%) of the total number of the surveyed indicated the presence of infertility in family history.
Failed IVF attempts in history were in 39.7% of patients in group 1 and in 41.1% in group 2, and the average number was 1.7 (0.2) and 1.8 (0.4), respectively. The live birth rate as the result of previous IVF attempts was 7.1%.
The expenses for the first IVF attempt in 51.8% of couples in group 1 and 56.9% of patients in group 2, the second IVF attempt in 59.1% and 60.3% of couples and the third IVF attempt in 70.1,% and 69.8% of couples, respectively, were covered by Compulsory Medical Insurance (CMI).
The patients’s own biological material was used in 89.7% of couples in group 1 and in 88.9% of couples in group 2. Donor sperm was used in 3.7% and 4.4% of patients, respectively. Donor eggs were used in 5.8% and 7.1% of women, respectively. Donor embryos were used in 0.8% and 0.9% of couples, respectively.
35% of women indicated the reason for using donated sperm in was that they had no sexual partners; 35.65% of women indicated mail partner’s reproductive system disorders that could not be treated as the reason for using donated sperm; 28.7% respondents refused to give an answer.
Frequency distribution of factors of infertility in couples according to IDC-10 is shown in Figures 2 and 3.
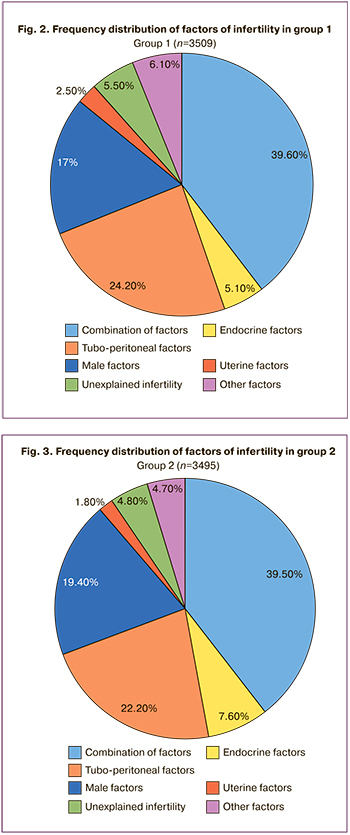
Tubo-peritoneal factor as only one factor of infertility was dominating in 849/3509 (24.2%) and 777/3495 (22.2%) patients in group 1 and 2, respectively, and male factor of infertility was in 598/3509 (17%) and 677/3495 (19.4%) patients respectively. Endocrine causes of infertility were in 180/3509 (5.1%) and 267/3495 (7.6%) women in groups 1 and 2. Other types of infertility (including ICD coded extragenital endometiosis) were in 213/3509 (6.1%) and 163/3495 (4.7%) women; unexplained infertility was in 191/3509 (5.5%) and 167/3495 (4.8%) women; uterine factors of infertility were in 88/3509 (2.5%) and 63/3495 (1.8%) women, respectively.
It is notable that 1390/3509 (39.6%) couples in group 1 and 1381/3495 (39.5%) patients in group 2 had a combination of factors of infertility.
Figure 4 presents the frequency of combination of male and female factors of infertility.
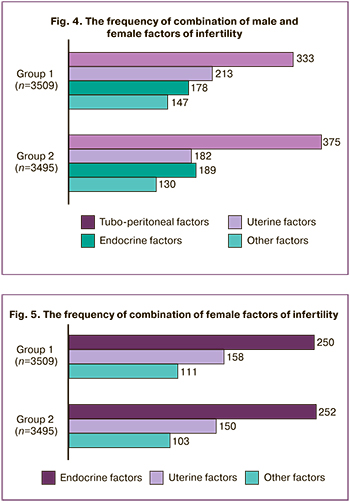
Male causes of infertility were most often combined with tubal factor in women – in 333/1390 (24%) couples in group 1 and 375/1381 (27.2%) in group 2. Uterine pathology was less often – in 213/1390 (15.3%) and in 182/1381 (13.1%) women, and absence of ovulation was in 178/1390 (12.8%) and in 189/1381 (13.7%), as well as other factors were in 147/1390 (10.5%) and 130/1381 (9.4%), respectively.
A combination of female factors of infertility in the absence of male factors is presented in Figure 5.
In the absence of male factors, tubo-peritoneal factor was most often combined with the absence of ovulation in 250/1390 (18%) and 252/1381 (18.2%) women, with uterine factors in 158/1390 (11.4%) and 150/1381 (10.9%) women, and other factors of infertility in 111/1390 (8%) и 103/1381 (7.5%) women, respectively.
Discussion
The results of the study showed that social and economic factors form the circumstances that influence the demographic situation in the country, namely delayed childbearing and delay in seeking infertility treatment. Thus, over the past 5 years the age of infertile couples seeking treatment increased on average by 4 years, and was 34 (4.8) years for women and 35.5 (5.9) years for men. At the same time the proportion of women over 40 increased by 4 times.
It is quite natural that in 80% of cases, urban residents seek infertility treatment due to better awareness of possible methods of implementing the reproductive function and accessibility of this type of medical care. However, the tendencies in the recent 5 years demonstrate increasing awareness of the rural population in this field. So, the share of rural residents seeking treatment in fertility clinics increased by 23.5% in 2020. There is no doubt that CMI system considerably contributed to this indicator, due to the fact that IVF program has become more accessible to a wide range of people with different incomes.
Education level, as well as the number of women having 2 types of higher education and graduate degrees, increased. Nevertheless, more than half of respondents supposed that IVF could help to achieve pregnancy at any age.
Early sexual initiation was at the age of 16, and the percentage of civil law marriages increased by 3% for the last 5 years. The number of infertile HIV-infected couples planning infertility treatment using IVF program increased.
The average duration of infertility, that is the length of time during which a couple wanted to conceive did not change essentially, and was about 4 years. At the same time, the increasing age of infertile couples seeking treatment demonstrated the trend toward delayed childbearing.
Almost half of patients had 1–2 failed IVF attempts. At the same time, the expenses for the first IVF attempt in 60% of infertile couples, and for the second or the third attempt in 70% of patients were covered by CMI system.
Among the reasons for seeking treatment in fertility clinics, every second woman indicated previously performed gynecological surgery, and every third woman reported failed pregnancies in history.
The leading causes of infertility were combined factors (40%) in the structure of infertility causes. Most often male factors were combined with tubo-peritoneal infertility, uterine pathology and ovulatory dysfunction. In the absence of male factors, tubo-peritoneal factor was most often combined with ovulatory dysfunction and uterine pathology.
The analysis of the frequency of different factors of infertility showed that despite a certain reduction in the number of women with tubo-peritoneal factor of infertility, this factor remains the leading cause of infertility. Male causes rank second in the frequency of infertility, and ovulatory dysfunction rank third.
The structure of infertility presented in this study differs from similar indicators in European countries, where ovulatory dysfunction (30–32%) is the leading cause of infertility, and the frequency of tubo-peritoneal factor as the only cause or in combination with male factor does not exceed 27% [3, 11].
In our study, the frequency of male infertility in combination with or without female factors was comparable with the indicators in the developed countries (30–40%) [3].
The results of epidemiologic study on the prevalence of the causes of infertility in the West Siberian region were published in 1998, and showed that tubo-peritoneal factor was a leading factor of infertility [12].
Why does tubo-peritoneal factor of infertility prevail for more than 20 years on the territory of Russia [13]?
The causes of impaired patency of the fallopian tubes and pelvic adhesions are known: these are sexually transmitted infections, pelvic surgery, medical abortions, complications in the post-abortion and postpartum period. It should be recognized that these indicators indirectly reflect the quality of medical care for women of reproductive age. In this study, every second respondent in their answers to the question about the reason of seeking treatment in fertility clinics indicated gynecological surgery, and every third respondent indicated complications in the post-abortion and in the postpartum period.
Conclusion
The results of the study substantiated the need for a most thorough analysis of the obtained data to assess the quality of health care and improvement of management of infertile couples taking into account current trends in reproductive medicine.
References
- Zegers-Hochschild F., Adamson G.D., Dyer S., Racowsky C., de Mouzon J., Sokol R. et al. The international glossary on infertility and fertility care, 2017. Hum. Reprod. 2017; 108(3): 393-406. https://dx.doi.org/10.1016/j.fertnstert.2017.06.005.
- Vander Borght M., Wyns C. Fertility and infertility: definition and epidemiology. Clin. Biochem. 2018; 62: 2-10. https://dx.doi.org/10.1016/j.clinbiochem.2018.03.012.
- Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/nchs/nsfg/key_statistics/i-keystat.htm#infertility
- Федеральная служба государственной статистики. Доступно по:https://rosstat.gov.ru/folder/12781 [Federal State Statistics Service. Available at: https://rosstat.gov.ru/folder/12781 (in Russian)].
- Паскарь С.С., Калугина А.С., Боярский К.Ю., Губанов С.А. Клинико-анамнестические характеристики и прогностический анализ исходов ВРТ у пациентов молодого репродуктивного возраста. Проблемы репродукции. 2018; 24(6): 76-82. [Paskar S.S., Kalugina A.S., Boiarskiĭ K.Iu., Gubanov S.A. Clinical characteristics and prognostic analysis of ART treatment in young patients. Russian Journal of Human Reproduction. 2018; 24(6): 76 82. (in Russian)]. https://dx.doi.org/10.17116/repro20182406176.
- Отчет РАРЧ за 2020 год. Доступно по: https://www.rahr.ru/registr_otchet.php [RAHR Report 2020. Available at: https://www.rahr.ru/registr_otchet.php (in Russian)].
- Farquhar C.M., Bhattacharya S., Repping S., Mastenbroek S., Kamath M.S., Marjoribanks J., Boivin J. Female subfertility. Nat. Rev. Dis. Primers. 2019; 5(1): 7. https://dx.doi.org/10.1038/s41572-018-0058-8.
- Ходакова О.В., Дударева В.А. Социально-гигиеническая оценка состояния системы охраны материнства и детства на региональном уровне. Проблемы социальной гигиены, здравоохранения и истории медицины. 2020; 28(3): 423-9. [Khodakova O.V., Dudareva V.A. The social hygienic evaluation of condition of system of maternity and childhood care at the regional level. Problems of Social Hygiene, Public Health and History of Medicine. 2020; 28(3): 423-9. (in Russian)]. https://dx.doi.org/10.32687/0869-866X-2020-28-3-423-427.
- Садыков Р.М., Большакова Н.Л. Женское здоровье: состояние, причины ухудшения, меры по улучшению. Проблемы социальной гигиены, здравоохранения и истории медицины. 2022; 30(2): 247-52. [Sadykov R.M., Bolshakova N.L. The female health: status, causes of deterioration, measures of improvement. Problems of Social Hygiene, Public Health and History of Medicine. 2022; 30(2): 247-52. (in Russian)]. https//dx.doi.org/10.32687/0869-886X-2022-30-2-247-252.
- Лебедев Г.С., Голубев Н.А., Шадеркин И.А., Шадеркина В.А., Аполихин О.И., Сивков А.В., Комарова В.А. Мужское бесплодие в Российской Федерации: статистические данные за 2000-2018 годы. Экспериментальная и клиническая урология. 2019; 4: 4-12. [Lebedev G.S., Golubev N.A., Shaderkin I.A., Shaderkina V.A., Apokikhin O.I., Sivkov A.V., Komarova V.A. Male infertility in the Russian Federation: statistical data for 2000-2018. Experimental and Clinical Urology. 2019; (4): 4-12. (in Russian)]. https://dx.doi.org/10.29188/2222-8543-2019-11-4-4-12.
- Snow M., Vranich T.M., Perin J., Trent M. Estimates of infertility in the United States: 1995-2019. Fertil. Steril. 2022; 18(3): 560-7.https://dx.doi.org/10.1016/j.fertnstert.2022.05.018.
- Шмидт А.А., Замятнин С.А., Гончар И.С., Коровин А.Е., Городнюк И.О., Коцур А.В. Эпидемиология бесплодия в России и за рубежом. Клиническая патофизиология. 2019; 1: 9-14. [Shmidt A.A., Zamyatin S.A., Gonchar I.S., Korovin A.E., Gorodnyuk I.O., Kotsur A.V. Epidemiology of infertility in Russia and abroad. Clinical Pathophysiology. 2019; (1): 9-14. (in Russian)].
- Николенко В.Н., Ризаева Н.А., Оганесян М.В., Кудряшова В.А., Голышкина М.С., Павлюк П.А., Унанян А.Л., Геворгян М.М., Припутневич Т.В. Трубное бесплодие: медико-социальные и психологические аспекты проблемы. Акушерство и гинекология. 2020; 11: 213-24. [Nikolenko V.N., Rizaeva N.A., Oganesyan M.V., Kudryashova V.A., Golyshkina M.S., Pavlyuk P.A., Unanyan A.L., Gevorgyan M.M., Priputnevich T.V. Tubal infertility: sociomedical and psychological aspects of the problem. Obstetrics and Gynecology. 2020; (11): 213-24. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.11.213-224.
Received 23.11.2022
Accepted 26.01.2023
About the Authors
Irina Е. Korneeva, Dr. Med. Sci., Professor, Leading Researcher at the Scientific and Educational Center of Auxiliary Reproductive Technologies with a Clinical Department named after Frederick Paulsen, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, irina.korneeva@inbox.ru,4 Academician Oparin str., Moscow, Russian Federation, 117997.
Tatiana A. Nazarenko, Dr. Med. Sci., Professor, Head of the Institute of Reproductive Medicine, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, t_nazarenko@oparina4.ru, 4 Academician Oparin str., Moscow, Russian Federation, 117997.
Svetlana G. Perminova, Dr. Med. Sci., Leading Researcher at the Scientific and Educational Center of Auxiliary Reproductive Technologies with a Clinical Department
named after Frederick Paulsen, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, perisvet@list.ru,
4 Academician Oparin str., Moscow, Russian Federation, 117997.
Elena V. Mityurina, PhD, Senior Researcher at the Scientific and Educational Center of Auxiliary Reproductive Technologies with a Clinical Department
named after Frederick Paulsen, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, e_mityurina@oparina4.ru,
4 Academician Oparin str., Moscow, Russian Federation, 117997.
Tatyana I. Cybizova, Deputy Development Director, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
4 Academician Oparin str., Moscow, Russian Federation, 117997.
Ayuna E. Dashieva, graduate student, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(926)329-42-11, dr.dashieva@mail.ru,
4 Academician Oparin str., Moscow, Russian Federation, 117997.