В 2017 г. были опубликованы данные аудита критических акушерских состояний в учреждениях 8 федеральных округов Российской Федерации [1].
Помимо материнской смертности (МС) были проанализированы случаи тяжелых осложнений «near miss» (NM). Женщина NM – это беременная или родильница, которая оказалась в критическом состоянии, близком к смерти во время беременности, родов или в течение 42 дней после родов, но выжившая [2, 3]. Случаи NM и MС вместе относятся к тяжелым материнским исходам. Распространенность NM представляет собой соотношение несостоявшихся материнских смертей, ассоциированных с беременностью, к количеству беременных женщин. Также показатель NM является индикатором качества оказания акушерской помощи, которое может быть оценено по соотношению МС и осложненных случаев (МС/NM): Лондон – 1:118, Франция – 1:19, Россия – 1:18, Индия – 1:16, а также по индексу смертности (NM+МС/МС) – оба показателя обратно пропорциональны уровню помощи [4]. Во всем мире ведущими причинами случаев, едва не приведших к летальному исходу, являются преэклампсия (ПЭ) и эклампсия, акушерские кровотечения, сепсис, гипертензивные расстройства [5]. Поэтому глобальной целью современного акушерства является снижение МС за счет активного воздействия на предотвратимые факторы и управляемые осложнения (ПЭ и эклампсия, кровотечения, инфекционные осложнения), ассоциированные с беременностью и родами, – именно на них в мире приходится 50–80% в структуре факторов риска NM. К немедикаментозным (организационным) факторам риска NM относятся: нарушение маршрутизации пациентов (несоответствие степени тяжести состояния пациента и прогнозируемых рисков мощности учреждения), нарушение утвержденных алгоритмов действий в экстренной или неотложной акушерской ситуации, отсутствие возможности оказания высокотехнологичной диагностической и лечебной помощи, территориальная удаленность и отсутствие доступа к быстрой транспортировке в стационар более высокого уровня перинатальной помощи [6, 7].
Клиническое наблюдение
Пациентка Н., 25 лет, была доставлена в экстренном порядке в отделение анестезиологии и реанимации (ОАР) НМИЦ АГП им. акад. В.И. Кулакова 12.11 2018 г. из лечебного учреждения одного из регионов, с диагнозом: вторые срочные оперативные роды в сроке 37 недель 2 дня от 11.11.18 г. по поводу преждевременного излития околоплодных вод, несостоятельности рубца на матке после операции кесарева сечения (КС) в 2014 г. Тяжелая ПЭ. HELLP-синдром. Послеродовый метроэндометрит. Перитонит. Тромботическая микроангиопатия (ТМА). Анемия тяжелой степени.
Из истории родов и анамнеза заболевания. Данная беременность вторая, I триместр протекал без особенностей. Во II триместре наблюдалась анемия легкой степени, в 18–19 недель перенесла ОРВИ без лихорадки. В 26–27 недель – угроза преждевременных родов (ПР) (консервативное лечение в стационаре), в 34 недель были выявлены признаки маловодия, нарушения маточно-плацентарного кровотока 1а степени. 11.11.2018 г. в 2:30 у беременной появились жалобы на тянущие боли внизу живота и излитие околоплодных вод, она была госпитализирована в родильный дом по месту жительства. Учитывая наличие рубца на матке после операции КС, преждевременное излитие околоплодных вод, неготовность родовых путей, в 3:36 было произведено экстренное оперативное родоразрешение – лапаротомия по Джоэл–Кохену с иссечением кожного рубца, рассечение и лигирование спаек, КС в нижнем маточном сегменте по Дерфлеру. На 13-й минуте был извлечен живой доношенный мальчик массой 2900 г, длиной 49 см (оценка по шкале Апгар 6/7 баллов) и передан неонатологу. Интраоперационная кровопотеря составила 700 мл. В реанимационном отделении проводили системную антибактериальную терапию (цефалоспорин III поколения 2,0 г), инфузионную терапию 500 мл, выделено мочи 250 мл. С 11:00 пациентка отметила ухудшение состояния в виде нарастания слабости и появления боли в правом подреберье, снижения давления, отмечалась олигурия, подъем температуры тела до 38 °С. Данные обследования: шизоциты 2,2%; ЛДГ 1058 Ед/л; креатинин 186 мкмоль/л; ЩФ 168 Ед/л; АЛТ 16 Ед/л; АСТ 79 Ед/л. Гемоглобин 77 г/л, лейкоциты 25,4×109/л; тромбоциты 220×109/л. По данным ультразвукового исследовании (УЗИ) органов брюшной полости – гепатоспленомегалия, свободная жидкость в подпеченочном пространстве в объеме до 10 мл. При УЗИ почек обнаружены признаки диффузных изменений. По данным УЗИ органов малого таза, полость матки расширена до 10 мм. После консультаций хирурга, терапевта и нефролога в перечень дифференциально диагностического поиска вошли: тяжелая ПЭ, HELLP-синдром, холестаз, острое почечное повреждение 2 стадии, острый отечный панкреатит. Была начата антибактериальная терапия (меронем, метрогил внутривенно), инфузионная терапия, профилактика тромбоэмболических осложнений, стимуляция диуреза. В связи с отсутствием эффекта от проводимой терапии и ухудшением состояния в 23.30 12.11.2018 г. пациентка была экстренно госпитализирована в учреждение III уровня оказания акушерской помощи в ОАР НМИЦ АГП им. В.И. Кулакова.
Осмотр при поступлении в ОАР. Состояние родильницы тяжелое, обусловленное течением тяжелой ПЭ, HELLP-синдромом, септическим процессом, почечным повреждением (олигурия), анемическим синдромом, сроком и объемом оперативного вмешательства. Оценка по шкале SOFA (Sequential Organ Failure Assessment) составила 6 баллов (индекс оксигенации 254), тромбоциты 87×109/л, билирубин 11.8 мкмоль/л, шкала комы Глазго 15 баллов, креатинин 280,4 мколь/л, анурия), тяжесть HELLP-синдрома – 2 класс по шкале Mississippi (АСТ – 425,9 Ед/Л, AЛT – 104,2 Ед/Л, ЛДГ – 796,9 Ед/л) [8]. Пациентка в сознании, сонлива, на вопросы отвечает, в пространстве и времени ориентирована. Предъявляет жалобы на слабость, одышку, жажду, умеренную болезненность в области оперативного вмешательства и в правом подреберье (3 балла по визуально-аналоговой шкале – ВАШ). Матка при пальпации тестоватой консистенции, увеличена до 18–19 недель беременности. Перистальтика кишечника не выслушивается. Послеоперационная рана чистая. В мочеприемнике 25 мл светло-желтой мочи. Выделения из половых путей скудные, кровянистые, мутные. Артериальное давление составило 110/70 мм рт. ст. на обеих руках, пульс – 112 ударов за минуту, частота дыхательных движений – 22 за минуту, сатурация (SpO2) по монитору – 98%. Температура тела 37,5 0С.
На коже правого плеча и на передней брюшной стенке, груди единичные гематомы. В легких дыхание везикулярное, несколько ослаблено снизу, без крепитации. При получении данных лабораторных методов исследования: в общем анализе крови – лейкоцитоз до 45,19×109/л, эритроциты 2,86×1012/л, гемоглобин 70 г/л, тромбоциты 87×109/л, нейтрофилы 93,8%, шизоциты 2,2%; с нарастанием анемии (гемоглобин 60 г/л) и тромбоцитопении (51×109/л).
В биохимическом анализе крови – общий белок 45,1 г/л, альбумин 23,2 г/л, глюкоза 2,9 ммоль/л, мочевина 11,9 ммоль/л, креатинин 280,4 мкмоль/л, прямой билирубин – 7,9 мкмоль/л, АЛТ – 1042 Ед/л, АСТ – 425,9 Ед/л, ЛДГ – 796,0 Ед/л, С-реактивный белок – 181, 53 мг/л, K+ 4,5 ммоль/л, прокальцитонин > 200 нг/мл. Уровень активности эндотоксина (ЕАА) высокий – 0,8.
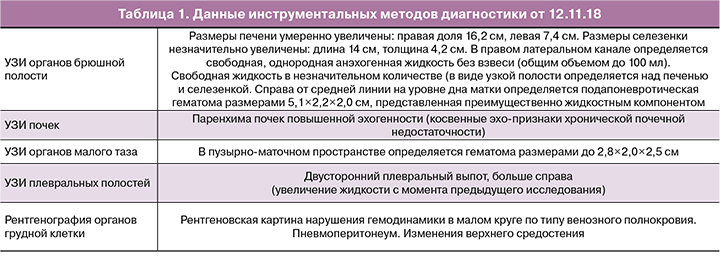
В общем анализе мочи – плотность <1,005, неизмененные эритроциты 50–60 в поле зрения; в гемостазиограмме Фибриноген – 2,12 г/л, протромбиновое время 18,4 с, протромбин по Квику – 48%, МНО 1,63, АЧТВ – 37,6, ТЭГ – прямая линия, D-димер – 73900 мкг/л. ADAMTS-13 10%. Антифосфолипидные антитела – не обнаружены. На посев взяты кровь, моча, слюна, кал, отделяемое из зева, трахеи, влагалища. Данные инструментальных исследований представлены ниже (табл. 1).
Родильница консультирована специалистами Центра: терапевтом, нефрологом, гематологом, трансфузиологом, хирургом, неврологом, офтальмологом, микробиологом. В результате обследования выставлен диагноз: вторые сутки после вторых оперативных родов на сроке 37 недель 2 дня по поводу преждевременного излития околоплодных вод, рубца на матке после операции КС в 2014 г. HELLP-синдром. Послеродовый эндометрит. Сепсис. ТМА. ДВС-синдром. Острое почечное повреждение 2 стадии. Анемия тяжелой степени. С 13.11.18 г. начата антибактериальная терапия препаратами широкого спектра, инфузионная терапия, проведен аппаратный плазмообмен с удалением 1,5 объема циркулирующей плазмы с замещением донорской лейкоредуцированной, карантинизированной свежезамороженной плазмы (СЗП) в эквивалентном объеме, выполнено переливание отмытых донорских эритроцитов в объеме 520 мл, начата процедура гемодиализа. Назначена нефропротективная, гастро- и гепатопротективная, ноотропная терапия, профилактика тромботических осложнений; пациентка была переведена на продленную искусственную вентиляцию легких (ИВЛ), которая продолжалась в течение 7 дней.
В связи с наличием признаков метроэндометрита, перитонита и синдрома системной воспалительной реакции (температура 38 0С, тахикардия, лейкоцитоз, повышение прокальцитонина, ЕАА) 14.11.18 г. была произведена лапароскопическая ревизия органов брюшной полости, гистероскопия. При лапароскопии: в поддиафрагмальном пространстве обнаружено до 800 мл мутного выпота (взят посев), визуально тело матки увеличено до 25 недель беременности, дряблой консистенции, фиксировано рыхлыми сращениями с париетальной брюшиной в проекции рубца после КС – сращения разделены. Брюшная полость промыта 3000 мл озонированного физиологического раствора с концентрацией озона 5 мг/л. При гистероскопическом исследовании: полость матки увеличена, не деформирована, заполнена наложениями фибрина и остатками плацентарной ткани по передней стенке. Состоятельность рубца подтверждена введением под давлением раствора метиленового синего. Выполнено выскабливание стенок полости матки – соскоб обильный, проведена санация матки 800 мл озонированного физиологического раствора с концентрацией озона 3 мг/л. Матка сократилась. В позадиматочное пространство и область пузырно-маточной складки установлены дренажи.
14.11.18 получены данные микробиологических исследований: при исследовании биоматериала из трахеобронхиального древа, толстой кишки, крови обнаружена Candida tropicalis (титры: 1,0E+06 KOE, 1,0E+02 KOE и 1,0E+04 KOE соответственно). В посевах мочи, слюны и кала обнаружена Сandida nonalbicans tropicalis (титр 106), с промежуточной чувствительностью к миконазолу. В течение последующих двух недель пациентка получала антимикотики (вориконазол, микафунгин), противогрибковая терапия была дважды модифицирована, с достижением эффекта.
В результате обследования пациентки выявлено, что на первый план выходили имеющиеся признаки септического процесса, вторичной ТМА, почечного повреждения. В течение двух недель проводилась терапия с использованием различных методов экстракорпоральной гемокоррекции: проведено восемь процедур аппаратного плазмообмена с удалением 2000-3500 мл с замещением донорской СЗП в объеме к плазмоэксфузии 1:1. В связи с высоким уровнем ЕАА проведены четыре процедуры селективной сорбции липополисахаридов с использованием селективных колонок Альтеко, Токсипак. В связи с острым почечным повреждением проведено восемнадцать сеансов заместительной почечной терапии. В результате комплексной терапии с 24.11.18 появилась моча, далее темп диуреза увеличился, за сутки при однократной стимуляции объем мочи достиг 780–1200 мл. Заместительная почечная терапия была переведена в режим назначения по клиническим показаниям (общий отечный синдром, наличие абсолютных показаний по электролитному составу, кислотно-основному состоянию). С 26.11.18 были отменены антибиотики в связи со снижением маркеров воспаления (прокальцитонин менее 0,5 нг/мл, С-реактивный белок – 11 мг/л, ЕАА – 0,4). У пациентки в динамике терапии нормализовались показатели гемограммы, тромбоцитов.
В результате комплексной терапии с включением различных экстракорпоральных методов терапии нормализация показателей АЛТ и АСТ произошла к 5-му дню, билирубина – к 5–6-му, ЛДГ – к 19-му, тромбоцитов – к 7-м суткам терапии.
02.12.18 г. у пациентки появилась одышка, вынужденное положение тела с приподнятым изголовьем, снижение сатурации в покое до 87%, тахипноэ до 25–28 дыхательных движений, аускультативные признаки отека легких. Пациентка была переведена на CPAP; данные компьютерной томографии (КТ) также подтвердили наличие альвеолярного отека. Проведен сеанс гемодиафильтрации. При осмотре 03.12.18 г. одышки в покое нет, дыхание везикулярное, проводится во все отделы, некоторое ослабление в нижних отделах. Сатурация – 98–99%. Сохраняется слабость, сонливость. Диурез составил 2100 мл за истекшие сутки (стимуляция 100 мг лазикса выполнена однократно). По данным анализов: фибриноген – 2,5 г/л, протромбиновый индекс – 87%, альбумин – 38 г/л. Гемоглобин 86г/л, лейкоциты – 8,9×109/л; тромбоциты – 300×10 9/л, прокальцитонин – 0,17 нг/мл, С-реактивный белок – 17 мг/л.
По данным эхокардиографии (Эхо-КГ), глобальная сократимость левого желудочка была умеренно диффузно снижена (фракция выброса 42%), в связи с чем, по-видимому, и были связаны эпизоды отека легких. С целью коррекции сердечной недостаточности были добавлены ингибиторы ангиотензинпревращающего фермента и диуретики (верошпирон). Состояние стабилизировалось. Учитывая купирование признаков инфекционного процесса (клинические и лабораторные данные) 07.12.18 г. было принято решение о прекращении антимикотической терапии.
Осмотр на 29-е сутки пребывания в ОАР НМИЦ АГП (13.12.18): состояние пациентки средней степени тяжести, стабильное. Сознание ясное, контактна, жалоб не предъявляет. Лабораторные тесты: анемия средней степени тяжести (гемоглобин – 85 г/л) г/л, тромбоциты – 356×109/л, лейкоциты – 8,26×109/л, креатинин – 407,0 мкмоль/л, мочевина – 19,6 ммоль, ЛДГ – 462,6 ЕД/л, амилаза – 211,4 Ед/л, фибриноген – 5,46 г/л, D-димер – 2139 мкг/л, плотность мочи – 1,010, белок мочи – 0,3 г/л, бактериологическое исследование крови – роста флоры не выявлено. Мочеиспускание самостоятельное, моча светло-желтая, диурез за прошедшие сутки 2240 мл без стимуляции.
На момент перевода из ОАР в хирургическое отделение Центра, спустя 29 дней пребывания, состояние оценивалось как стабильное, средней степени тяжести, отсутствовала одышка в покое (дыхание везикулярное, проводилось с некоторым ослаблением в нижних отделах), сатурация на атмосферном воздухе 98–99%, уменьшилась слабость, диурез достаточный. Пациентка в удовлетворительном состоянии 19.12.18 была выписана с рекомендациями под наблюдение гинеколога, терапевта и нефролога по месту жительства.
Заключительный диагноз при выписке: 39-е сутки после 2-х оперативных родов. Послеродовый метроэндометрит. Перитонит. Сепсис: септицемия, вызванная C. tropicalis, с преимущественным поражением почек (Острое повреждение почек 2 степени, стадия восстановления диуреза), легких (Острый респираторный дистресс-синдром взрослых от 13.11), сердца (миокардит со сниженной сократительной способностью миокарда). Вторичная ТМА в стадии разрешения. Анемия средней степени.
При контрольной консультации через два месяца после выписки: состояние женщины удовлетворительное, жалоб не предъявляет. Лабораторные показатели: анемия легкой степени (гемоглобин 91 г/л), тромбоциты 232×109/л, лейкоциты 4,9×109/л без сдвига влево, креатинин 222.0 мкмоль/л, калий 4,2 ммоль/л, С- реактивный белок 2,15 мг/л, Д-димер 185 мкг/л, отсутствие РКМФ, фибриноген 3,7г/л, протромбиновый индекс 86%, АЧТВ 34 с. Общий анализ мочи: белок 0,3г/л, удельный вес 1010 г/л. Диурез 1600–1800 мл в сутки.
Обсуждение
Последние годы в клинической практике большое внимание уделяется показателю, характеризующему критические акушерские состояния, при которых в результате тяжелых осложнений при беременности, в родах, после родов, женщина едва не погибает, но выживает (NM). В современной отечественной и зарубежной литературе опубликованы данные частоты развития этих состояний при акушерских кровотечениях, ПЭ и эклампсии, сепсисе, экстрагенитальных заболеваниях, указаны факторы, которые надо учитывать, и меры, необходимые для предотвращения развития состояний NM. Частота критических акушерских состояний в 2016 г. составила в целом по Центральному федеральному округу 8,6 на 1000 родов, в том числе в медицинских организациях родовспоможения I уровня – 3,4‰, II уровня – 6,7‰, III – 14,8‰ [9]. Во многих работах представлена терминология критических состояний, дана оценка NM. Критерии NM изложены в документах ВОЗ «Идентификационные критерии случаев тяжелых акушерских осложнений, едва не завершившихся летальным исходом» [10–13], которыми пользуются практические врачи в диагностике этих состояний.
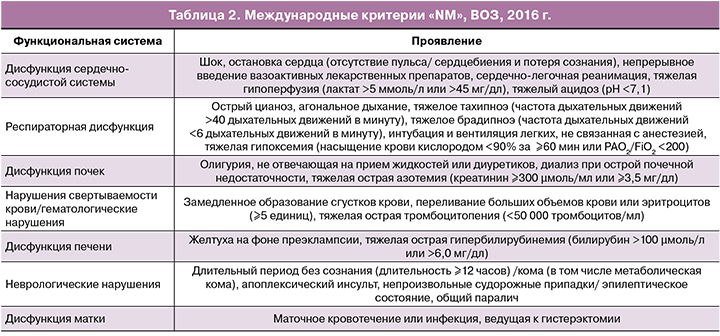
В статье представлено клиническое наблюдение развития критического состояния у повторно родящей женщины Н. 25 лет. При поступлении в НМИЦ АГП состояние родильницы соответствовало критериям ВОЗ «NM», что потребовало интенсивной комплексной терапии: у пациентки присутствовала сердечная, дыхательная, почечная, печеночная, неврологическая, маточная дисфункции, коагулопатия (табл. 2).
Шкала SOFA (Sequential Organ Failure Assessment), которая является более точной для оценки полиорганной недостаточности, составила 6 баллов, что характеризовало степень органной недостаточности и вероятность развития сепсиса у пациентки, что имело важное значение для соответствующего объема и длительности лечения, предотвращения грозных осложнений [14–16].
Следует сказать, что во всех исследованиях по анализу критических состояний в акушерстве подчеркнута важность быстрой маршрутизации такой пациентки в учреждение III уровня оказания лечебной помощи. Пациенка Н. была госпитализирована в НМИЦ АГП фактически на вторые сутки после манифестации патологического процесса, что позволило быстро и своевременно начать диагностический поиск и интенсивную терапию. Следует подчеркнуть, что, несмотря на сложности интерпретации клинических и лабораторных данных, у пациентки был установлен диагноз «Вторичная ТМА». Ассоциированная с беременностью и родами ТМА, независимо от срока ее развития, ставит перед врачом вопрос о необходимости постановки диагноза в кратчайшие сроки, так как от скорости начала патогенетической терапии зависит исход заболевания. Известно, что ТМА представляет собой гетерогенную группу заболеваний, проявляющихся клинико-морфологическим микроангиопатическим синдромом, в основе которого лежит повреждение эндотелия сосудов микроциркуляторного русла, представленное воспалением и тромбозом [17, 18]. В первую очередь в круг дифференциально диагностического поиска у данной пациентки был включен HELLP-синдром, атипичный гемолитико-уремический синдром (аГУС), тромботическая тромбоцитопеническая пурпура (ТТП) и катастрофический антифосфолипидный синдром (КАФС), сепсис. Несмотря на сходство клинико-лабораторных проявлений этих видов патологии, подходы к их лечению различны, в связи с чем своевременно и четко установленный диагноз является основным фактором, который определяет исход для пациентки [19–21]. У пациентки в родильном доме по месту жительства по данным кардиотокографии (КТГ) и УЗИ был выявлен синдром задержки роста плода (ЗРП) 2 степени, симметричная форма, маловодие и нарушения маточно-плацентарного кровотока, угроза преждевременных родов, по поводу которого она получала лечение в стационаре. После операции КС отмечено быстрое ухудшение состояния. При обследовании выявлен высокий уровень печеночных ферментов, билирубина, значительное повышение ЛДГ, снижение уровня тромбоцитов, анемия, нарушение функции печени и почек. Выставлен диагноз HELLP-синдром с поражением почек и начата инфузионная и антибактериальная терапия. Но следует подчеркнуть, что у пациентки было отмечено снижение артериального давления, подъем температуры тела до 38 °С, что может свидетельствовать о развитии септического процесса в сочетании с HELLP-синдромом. В течение одних суток родильница была переведена в НМИЦ АГП им. акад. В.И. Кулакова.
При поступлении в НМИЦ АГП для исключения первичных ТМА был проведен анализ уровня ADAMTS-13 (табл. 3), который составил более 10%, что не дало повода в данной ситуации рассматривать ТТП. Для исключения КАФС как причины острой полиорганной недостаточности, развивающейся в короткие сроки (от нескольких часов до нескольких дней) вследствие тромботической окклюзии сосудов органного микроциркуляторного русла, было проведено исследование серологических маркеров – в связи с отсутствием антифосфолипидных антител КАФС был исключен. Далее анализировались гипотезы относительно наличия ГУС. До развития симптомокомплекса острого почечного повреждения типичный ГУС манифестирует гастроинтестинальными симптомами острой кишечной инфекции (диарея, гемоколит), что было не характерно для анализируемой клинической картины [22].

Главный диагностический поиск был направлен на диагностику аГУС и сепсиса.
Беременность, и особенно ее осложненное течение, является комплемент-активирующим состоянием, что отчасти наделяет ее патогенетическим сходством с аГУС. Его основу составляет генетически обусловленный дефект регуляции альтернативного пути комплемента, результатом чего является его хроническая неконтролируемая активация и нарушение защиты эндотелиальных клеток вследствие образования на их поверхности мембрано-атакующего комплекса с последующим повреждением и обнажением субэндотелиального матрикса, трансформацией атромботического фенотипа в протромботический и последующим образованием тромбов, что приводит к полиорганной недостаточности (почек, печени, сердечно- сосудистой, дыхательной системы [23, 24]. Лабораторными методами диагностики, помимо ренального синдрома, были выявлены анемия, тромбоцитопения, элевация ферментов печени и маркеров воспаления (ЕАА, С-реактивный белок, прокальцитонин, лейкоцитоз) Анемия, а также наличие шизоцитов, количество которых в мазке периферической крови выше допустимых 0,1–1%, наряду с высокими показателями ЛДГ, свидетельствовали о механическом гемолизе эритроцитов образовавшимися тромбами, заполняющими сосуды микроциркуляторного русла, что приводит к тромбоцитопении потребления.
В динамике у нашей пациентки наблюдалось прогрессирование с генерализацией ТМА, которая проявилась вовлечением экстраренальных систем – двусторонний отек легких с развитием респираторного дистресс-синдрома взрослых, гемодинамические изменения и диффузное поражение миокарда с признаками постепенно нарастающей сердечной недостаточности, гидроперикард и поражение центральной нервной системы разной степени выраженности (сонливость, раздражительность). Верификация аГУС потребовала бы назначения антикомплементарных препаратов (экулизумаб), подтверждение другого диагноза – сепсиса, – иной тактики. Фульминантное развитие в течение менее 24 ч от момента операции до вовлечения нескольких систем органов было обусловлено сепсисом (острое изменение по шкале SOFA превысило 2 балла, в процессе ведения пациентки был верифицирован метроэндометрит, перитонит, высокие показатели С-реактивного белка, прокальцитонина, ЕАА. Обнаружены возбудители септического процесса: при посеве крови, биоматериала из трахеобронхиального древа и толстой кишки обнаружена Candida tropicalis. В посевах мочи, слюны и кала обнаружена Сandida nonalbicans (tropicalis). На первый план вышел диагноз сепсис, и было принято взвешенное решение о дальнейшем продолжении изложенной выше лечебной тактики с добавлением антимикотической терапии, которую проводили препаратами широкого спектра действия (вориконазол, микафунгин), проводили санацию очагов инфекции, экстракорпоральную детоксикацию различными методами, заместительную почечную терапию. Мероприятия, направленные на купирование проявлений развивающейся полиорганной недостаточности, продемонстрировали эффект, в первую очередь, благодаря комплексной терапии, при подборе этиопатогенетического лечения. Известно, что и сепсис может стать триггером аГУС как любой инфекционный процесс. Согласно российским и международным протоколам, при развитии ТМА, если она еще не дифференцирована, первой линией терапии является плазмообмен в объеме 30–40 мл/кг массы, который является патогенетической терапией при ТТП, подготовительной – при аГУС, дополнительной – при HELLP-синдроме, сепсисе. В случае неэффективности данной терапии следует пересмотреть диагноз и решить вопрос о своевременном назначении антикомплементарных препаратов [25–27].
Проведение процедур плазмообмена, сеансов селективного удаления эндотоксина при сорбции липополисахаридов, гемодиафильтрации в комплексе с вышепредставленной терапией было эффективно, что позволило исключить диагноз аГУС. Необходимо подчеркнуть, при проведении плазмообмена для замещения использовали только лейкоредуцированную донорскую СЗП, что позволяет значимо снизить риски трансфузионной терапии, в том числе и повреждение легких, связанное с трансфузией. Режимы плазмообмена составляли 30 мл/кг массы с эквивалентным объемом замещения СЗП, исходя из состояния сердечно-легочной деятельности, под ежедневным контролем количества тромбоцитов и уровня ЛДГ (как маркера прекращения гемолитической анемии). В результате терапии нормализация уровней АЛТ, АСТ произошла фактически к 5-м суткам терапии, тромбоцитов – к 7-м, уровня ЛДГ – к 19-м суткам в ОАР. С 13.11 по 06.12.18 г. пациентка находилась на заместительной почечной терапии, осуществляемой посредством гемодиализа и гемодиафильтрации. Положительная динамика отмечалась с 24.11.18 г. – постепенно увеличивался темп диуреза с достижением адекватного объема 1200–2200 мл за сутки. Об эффективности комплексной терапии с включением экстракорпоральных методов терапии в лечении сепсиса и его осложнений свидетельствуют многие работы последних лет [28–32].
Таким образом, настоящее наблюдение демонстрирует трудности диагностики этиологии вторичной ТМА, развившейся вследствие воздействия сочетания нескольких триггеров (ПЭ, HELLP-синдром, метроэндометрит, перитонит, сепсис, ДВС), а также возможности благоприятного исхода этого жизнеугрожающего состояния NM для матери в результате своевременно установленного диагноза и эффективной комплексной высокотехнологичной терапии. Анализ течения и исхода данного клинического наблюдения подтверждает правильность тактики госпитализации пациента с признаками ТМА в многопрофильный стационар с хорошо оснащенным отделением реанимации и интенсивной терапии, что обусловлено необходимостью применения гемодиализных методов лечения, плазмообмена, селективной сорбции липополисахаридов, продленной ИВЛ, а также хирургического лечения и экспертной консультации нефрологов, терапевтов, офтальмологов и других специалистов мультидисциплинарной команды, что позволило спасти жизнь женщины из категории NM. Важность своевременной маршрутизации критических больных, мультидисциплинарный подход в лечении этих пациенток, необходимость разработки единых четких критериев мониторинга и оценки акушерских критических случаев в зависимости от плотности населения и модели оказания перинатальной помощи подчеркивают работы многих зарубежных и отечественных исследователей [33–37]. Также необходимо подчеркнуть: лечение таких пациенток требует значительных материальных вложений. Так, общая стоимость терапии данной пациентки составила 15 240 000 рублей.
Заключение
В заключение следует сказать, что для снижения частоты развития состояний NM у акушерских пациенток, учитывая их известные лидирующие причины необходимo:
- Своевременная и быстрая маршрутизация беременных группы высокого перинатального риска в стационары IIIa и IIIb уровней.
- Четкое выполнение установленных порядков, протоколов лечения, клинических рекомендаций при ведении акушерских пациенток, утвержденных Минздравом России.
- Постоянное повышение квалификации врачей акушеров-гинекологов, анестезиологов-реаниматологов, трансфузиологов.
- Современное оснащение отделений реанимации лекарственными препаратами, аппаратурой с возможностью проведения высокотехнологических методов терапии
Тщательный клинический анализ случаев NM – это весомый резерв дальнейшего снижения уровня летальности в случаях предотвратимой материнской смерти.