VULVOSCOPY IN PRACTICE OF OBSTETRIAN-GYNECOLOGIST
Apolichina I.A., Malyshkina D.A
Vulvoscopy is a diagnostic method in which, using a special optical technique, and examining of the vulva, vestibule of the vagina, the labia minora and majora and the clitoris is performed.
 In 1925 the German scientist Hans Ginselman created the world's first device – a colposcope, with which you can examine in detail the cervix, vagina and vulva. The device quickly gained popularity among doctors, became an integral part of the gynecological examination of women of all age categories with the entire spectrum of diseases of the genitourinary tract. Hans Ginzelman said thuring each colposcopic examination you must first examine the vulva, especially if the woman has complaints of itching.
In 1925 the German scientist Hans Ginselman created the world's first device – a colposcope, with which you can examine in detail the cervix, vagina and vulva. The device quickly gained popularity among doctors, became an integral part of the gynecological examination of women of all age categories with the entire spectrum of diseases of the genitourinary tract. Hans Ginzelman said thuring each colposcopic examination you must first examine the vulva, especially if the woman has complaints of itching.
Simple and advanced vulvoscopy is distinguished. The latter involves the use of special solutions to improve the visualization of suspicious areas. However, it must be remembered that the reaction to acetic acid is not always comparable with the reaction on the cervix, therefore, it does not always reliably reflect the degree of damage. In this regard the doctor should be especially wary of any suspicious areas in the vulva [1].
 Vulvoscopy requires a highly qualified doctor, as it has a number of important features. Firstly, the vulva area is extremely individual and rich in all kinds of formations, folds, age spots, which is often taken by a doctor for pathology, in this regard, the opposite situation is possible, and the doctor may miss a pathological formation. Secondly, in the area of the vulva there is a junction of the mucous membrane of the vulva and perineal skin, and as you know, any transition zone is most susceptible to cancer, which requires special on-alertness from the doctor.
Vulvoscopy requires a highly qualified doctor, as it has a number of important features. Firstly, the vulva area is extremely individual and rich in all kinds of formations, folds, age spots, which is often taken by a doctor for pathology, in this regard, the opposite situation is possible, and the doctor may miss a pathological formation. Secondly, in the area of the vulva there is a junction of the mucous membrane of the vulva and perineal skin, and as you know, any transition zone is most susceptible to cancer, which requires special on-alertness from the doctor.
Thirdly, as we already wrote, the standard solutions used in classical colposcopy do not give reactions comparable to those that we used to see when conducting colposcopy.
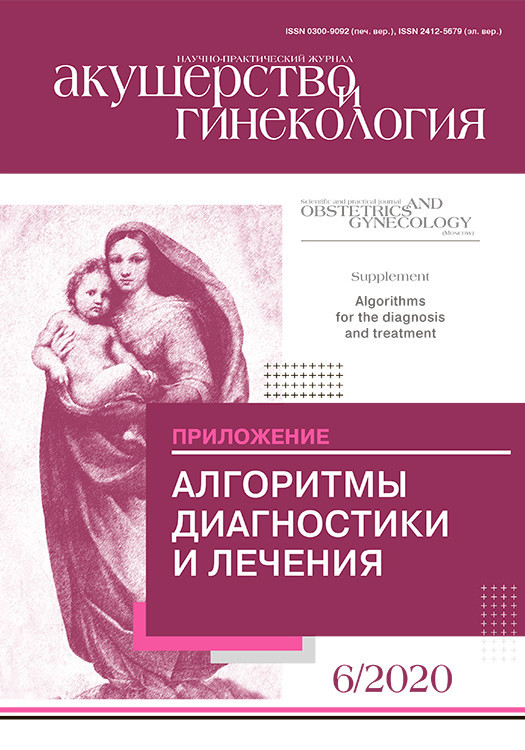
For example, when processing is done with Lugol's solution normally on the labia minora, the vulvovaginal Hart line (Fig. 1) is determined.
The Hart line is the medial border of the labia minora, this is the zone of transition into the mucous membrane [1].
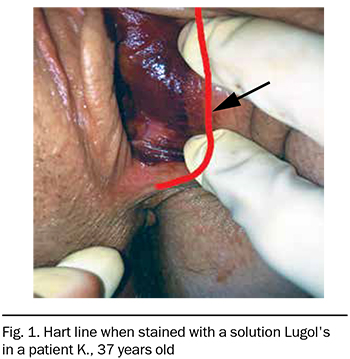
And finally, the vulva is an aesthetic zone with a large number of nerve endings that determine the quality of the sexual life of our patients (Fig. 2).
Indications for vulvoscopy [1-3]:
- complaints of itching or burning in the vulva;
- vulvodynia;
- chronicinflammatorydiseasesofthevulva(recurrent candida vulvovaginitis, aerobic vulvovaginitis);
- discomfort during urination and bowel movements, urinary incontinence, ammonium dermatitis;
- genitourinar menopausal syndrome and other conditions accompanied by atrophy of the vulva (sclerosing lichen);
- neoplasms in the area of the external genitalia (papillomas, adhesions, scars, erosion);
- copious discharge from the genital tract with an unpleasant odor;
- potting that is not related to the menstrual cycle;
- genital cancer in anamnesis;
- suspicion of VIN;
- monitoring the effectiveness of conservative and surgical treatment of vulvar diseases;
- dubious result of smears on cytology;
- abnormalities of the development of the genital organs;
- postradiation dermatitis in the vulva.
 As part of cancer awareness and as a screening of vulval diseases, it is desirable that vulvoscopy always precedes colposcopy. There are no contraindications to simple vulvoscopy. Contraindications to extended vulvoscopy are allergic reactions to solutions that are used to visualize pathogenic foci, vulvar injuries, and acute inflammations with abundant exudation.
As part of cancer awareness and as a screening of vulval diseases, it is desirable that vulvoscopy always precedes colposcopy. There are no contraindications to simple vulvoscopy. Contraindications to extended vulvoscopy are allergic reactions to solutions that are used to visualize pathogenic foci, vulvar injuries, and acute inflammations with abundant exudation.
It is best to perform vulvoscopy 1–3 days before menstruation or 1–3 days after it ends due to minimal secretion in the area of interest to us. 3–4 days before the examination, the woman should exclude sexual contact and other irritating effects: the use of intimate hygiene products (except for hypoallergenic ones), douching, vaginal candles, ointments. Remove the hair (it should be cut with scissors, it is undesirable to cause irritation of the vulva area by epilation or shaving). On the day of reception you should not use soap or simple shower gel as a means of intimate hygiene, you can only use a special hypoallergenic gel for intimate hygiene, for example, Pleyana® professional, Lactacyd® new.
Before starting the procedure, the necessary medical devices are prepared. The patient is explained the purpose and method of the procedure, it is necessary to obtain written informed consent, to clarify whether the woman is allergic to medications and solutions that will be used during the procedure. Vulvoscopy should be performed in sterile medical gloves.
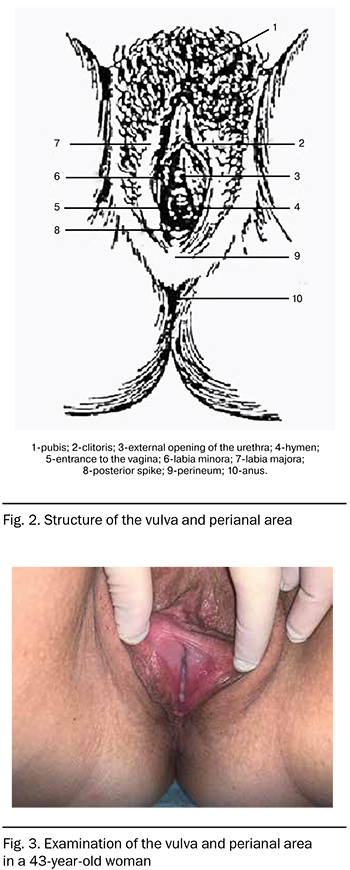
First, the doctor carefully examines the area of the external genitals without optical equipment (Fig. 3). Then begins the examination with a minimum magnification (7.5 times) to be able to assess the overall condition of this area.
It should be remembered that the most frequent location of the affected areas is the inner surface of the lower third of the labia minora, up to 50% of cases are multifocal lesions throughout the vulva, 35% are multicentric lesions of the vulva together with the cervix and vagina, the clitoris is affected only in 9% of cases. 75% of foci are located outside the hairline [4].
Then, if necessary, the doctor accurately assesses suspicious areas and captures them using a special function provided by modern digital colposcopes, or using a camera or smartphone camera.
Advanced vulvoscopy involves special tests, as described above.
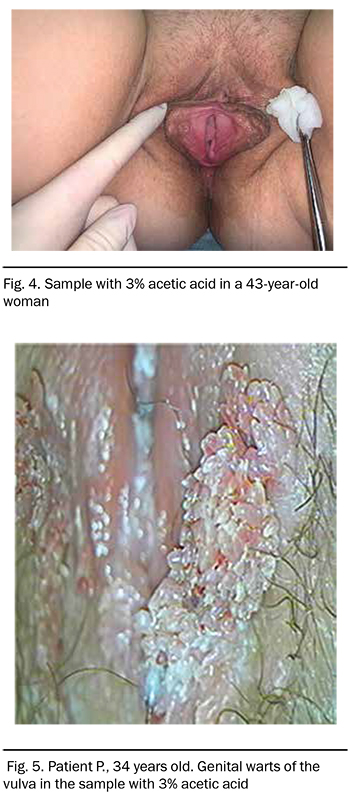
 Sample with acetic acid [5]
Sample with acetic acid [5]
A 3% solution of acetic acid is applied to the surface of the vulva (Fig. 4, 5). Pathological tissues acquire a whitish hue due to a specific vascular reaction. It should be noted that the exposure to acetic acid solution increases to 3-5 minutes compared to that on the cervix and vaginal mucosa. At this stage it is possible to use color-coded techniques (DySIS map), which allow us to use modern colposcopes, but they, unfortunately, are not sufficiently informative and specific, since they were originally developed for the diagnosis of the degree of damage to the cervix.
The Schiller test [5]
The Schiller test is not specific to vulvoscopy. It consists in applying a solution of Lugol to the vulva mucosa (Fig. 6). The Test is based on the ability of glycogen, which is contained in healthy epithelial cells, to be stained with iodine, while in pathological cells there is little glycogen, and they practically do not change color.
The Collin test
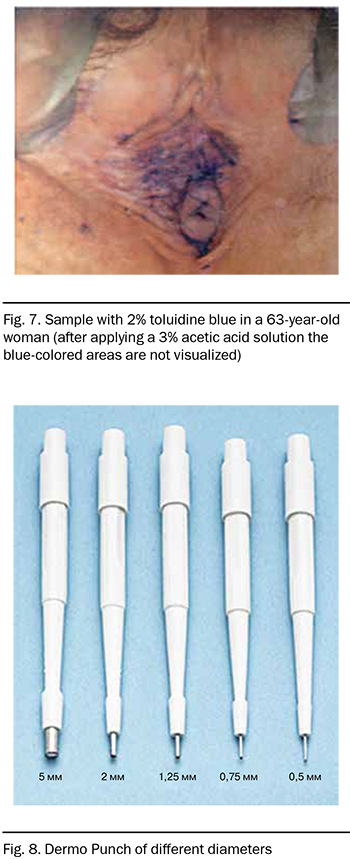
A sample with 2% toluidine blue, a nuclear dye that fixes the nuclei, is also used. It is applied with a cotton swab for 2-3 minutes, and then removed with a 3% solution of acetic acid (Fig. 7). With normal tissues, the dye is easily washed off, on the affected tissues from cells with abnormal nuclei, the dye remains and gives a blue staining. However, in parakeratosis immature cells can provide a false positive result.
All the tests described above help the doctor choose the location for the biopsy, but do not reflect the extent and depth of the lesion [6].
Vulvar biopsy
This is an extremely painful procedure due to very good innervation and high sensitivity of the vulva, so anesthesia is necessary. Most often used subcutaneous administration of 2% lidocaine solution using insulin syringes, as the most atraumatic. Sometimes analgesics are also used in the form of a cream, gel, or aerosol, for example, EMLA cream (eutectic mixes of local anastatic).
The biopsy itself is quite a traumatic procedure, and it must be performed carefully and accurately, especially in patients with atrophy, whose tissues are characterized by extreme fragility and thinning
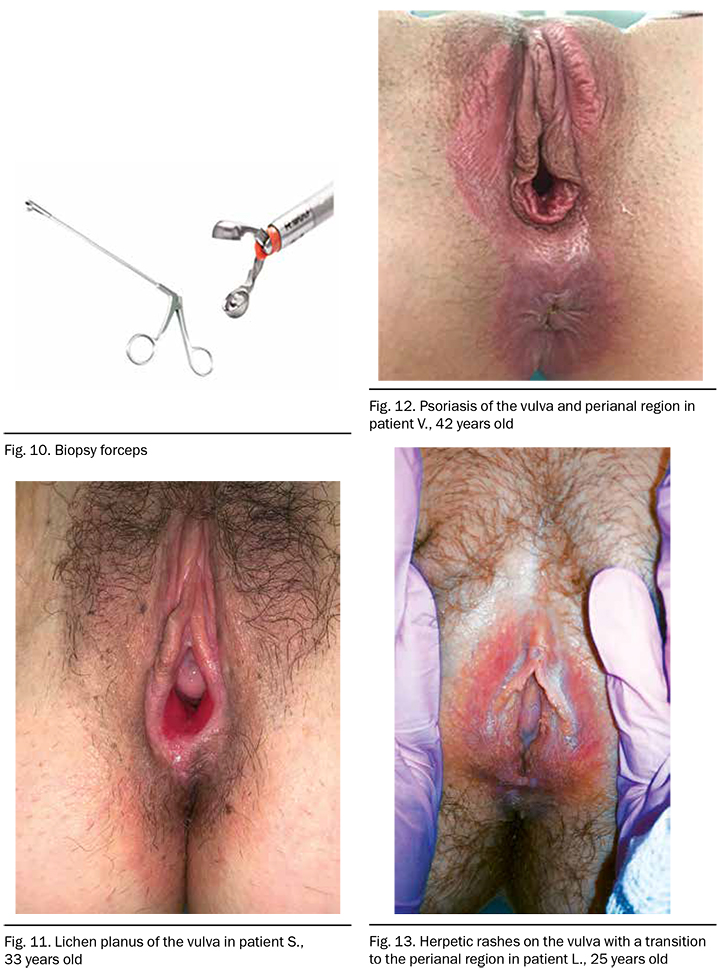
 There are many methods of conducting a biopsy: using a scalpel, special forceps, or an electric needle. The most sparing method is a circular biopsy using a Keyes punch, which has different diameters for sections of different sizes (Fig. 8). The Scalpel is placed in the place of the intended biopsy, cut in with a slight pressure, then the section is lifted with tweezers and cut off (Fig.9).
There are many methods of conducting a biopsy: using a scalpel, special forceps, or an electric needle. The most sparing method is a circular biopsy using a Keyes punch, which has different diameters for sections of different sizes (Fig. 8). The Scalpel is placed in the place of the intended biopsy, cut in with a slight pressure, then the section is lifted with tweezers and cut off (Fig.9).
When the vulva is biopsied using a radio-wave loop after subcutaneous injection of an anesthetic when the tissue to be biopsied is lifted with the needle of the same syringe. Next the radio-wave loop of the electrode is wound under the needle, and with its help, the necessary area of tissue is taken, necessarily with the subject stroma. The resulting wound surface is treated with a solution of brilliant green.
There are also 2 methods of using biopsy forceps (Fig. 10): the first method is similar to the method of performing a biopsy using an electric needle, when the tissue section of interest is lifted on the needle of the syringe that was used for anesthesia, the working part of the forceps is brought to this area, and there is a targeted collection of tissue with a section of stroma. In the second method, the opened forceps are immersed in the tissue so that the biopsy site is between the working branches of the forceps, after which it is also easily biopted. The wound surface is also treated with a solution of diamond green.
It should be remembered that only a full histological examination can confirm the diagnosis.
Vulvoscopic classification
Currently, there is no generally accepted vulval classification of vulval lesions, but the International society for the study of vulval and vaginal diseases (ISSVD) suggests using the classification of abnormal vulval lesions according to the color of the lesion: white, red, dark [7].
Red lesions of the vulva (Red Lesion)
Causes hyperemia of the vulva may be:
- expansion of blood vessels due to immune or inflammatory reaction (dermatitis, eczema);
- thinning of the epithelium (atrophy of the vulva);
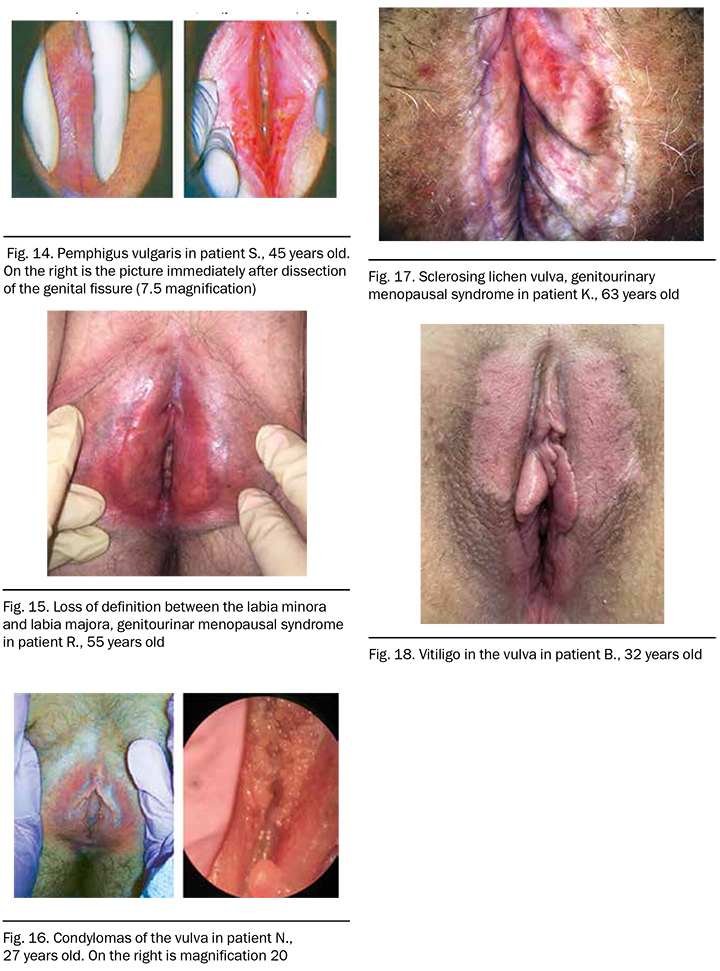
- dermatoses (red lichen planus (Fig. 11), psoriasis (Fig. 12), etc. (Fig. 13–15));
- neovascular neoplasia (VIN, Paget's disease, vulvar cancer).
Diffuse hyperemia is more typical for benign processes, while focal localized lesions may indicate malignant lesions.
White lesions of the vulva (White Lesion)
The causes of white vulva lesions can be:
- keratinization (physiological reaction in response to any stimulus, vulvar leukoplakia);
- weak vascularization and acetobelic reaction (HPV infection (Fig. 16) , sclerosing lichen (Fig. 17), VIN);
- depigmentation (vitiligo (Fig. 18), leucoderm on the background of the scar)
Dark lesions of the vulva (Dark Lesion)
Causes of vulva hyperpigmentation can be:
- increased concentration of melanin after trauma, local use of estrogens, while taking hormones;
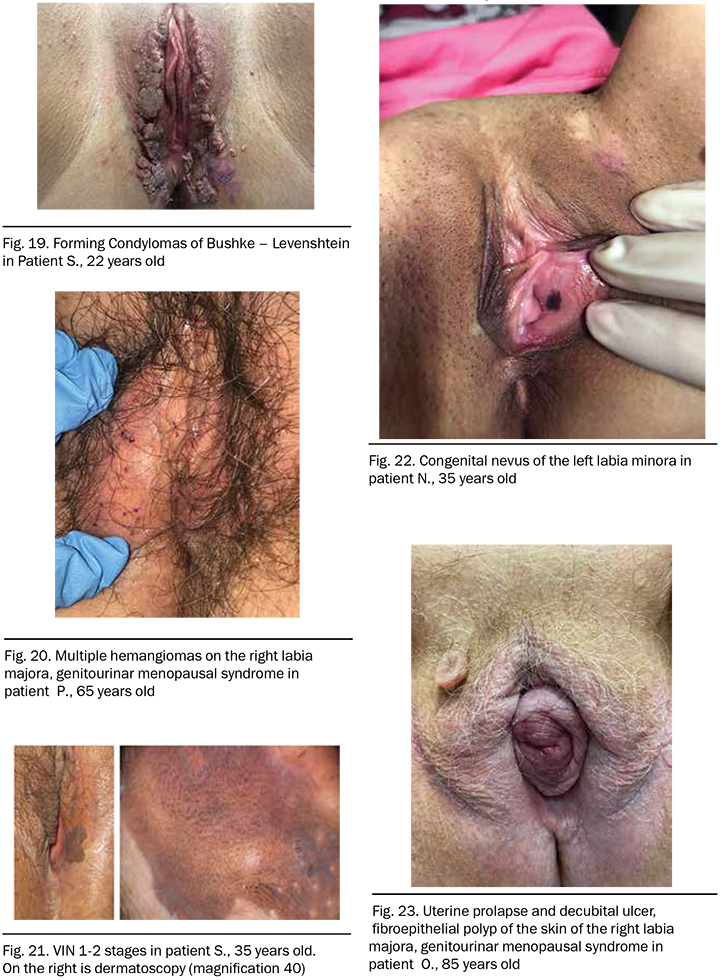
- exophytic warts (Fig. 19);
- hemangiomas (Fig. 20);
- VIN (Fig. 21);
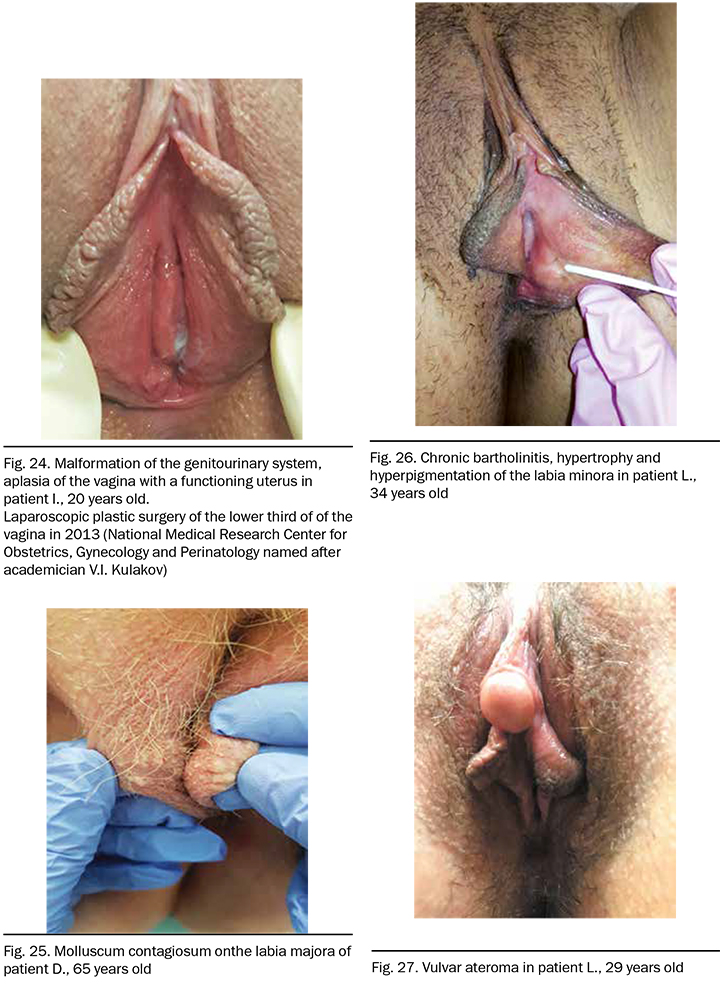
Other pathology of the vulva (Fig. 23–27)
Vulvoscopy is an important part of the diagnostic process, the first stage of colposcopy. Every obstetrician- gynecologist should know the technique of vulvoscopy and be able to diagnose vulval pathology.
Note. All photographs are part of the archive of the Department of Aesthetic Gynecology and Rehabilitation of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after academician V.I. Kulakov.
References
1. Rogovskaya S.I. Practical colposcopy. 3rd ed., Rev. and add. M .: GEOTAR-Media, 2013.240 s.
2. Manukhin I.B., Kondrikov N.I., Kraposhina T.P. External genital diseases in women. M .: MIA, 2002.330 s.
3. Federal clinical guidelines. Dermatovenerology, 2015: Diseases of the skin. Sexually transmitted infections. M., 2016. 5th ed., Revised. and add. M.: Delovoy Express,2016.768 s.
4. Fambrini M., Penna C., Pieralli A., Fallani M.G., Andersson K.L., Lozza V., Scarselli G., Marchionni M. Carbon-dioxide laser vaporization of the Bartholin gland cyst: a retrospective analysis on 200 cases. J. Minim Invasive Gynecol. 2008 May-Jun; 15 (3): 327-31.
5. EAGC Course Book on Colposcopy. Edited by P. Bocze, D.M. Luesley. Primed-x Press, Budapest, 2003.
6. Singer А., Monaghan J.M. Lower Genital Tract Precancer. Colposcopy. 1994.
7. ISSDV – International Society for Study Vulvar Disease (Международное общество по исследованиям заболеваний вульвы).