Tissue thermometric characteristics in the intervention area during electrosurgical vaginal hysterectomy
Safe and effective hemostasis is one of the most important factors in minimally invasive surgery.Plekhanov A.N., Bezhenar V.F., Epifanova Т.A., Bezhenar F.V., Shishkina Yu.S, Tatarova N.A.
Objective. To measure the maximum temperature of the working branches of bipolar tools used for hemostasis during vaginal hysterectomy (VH).
Subjects and methods. The investigation enrolled 29 patients who had undergone VH. The female patients were divided into three groups according to the tool used for tissue coagulation. A BiClamp was used in Group 1 (n = 10); a TissueSeal Plus clamp was applied in Group 2 (n = 10), and a Thunderbeat clamp was employed in Group 3 (n = 9). The maximum temperature was measured using a Fluke FLK TiS 40 9HZ infrared imaging camera.
Results. The median maximum temperature of the branches on electroligation with a BiClamp was 113.20°С; that at the coagulation boundary was 71.65°С. On ligation with a Thunderbeat clamp, the temperature of the branches was 165.49°С; that at the coagulation boundary was 54.59°С. On ligation with a TissueSeal Plus clamp, the temperature of the branches was 84.63°С; that at the coagulation border was 47.78°С (p = 0.0001). The median maximum temperature of tool branches on electroligation and that at the border of coagulation with intact tissue were much lower than that with TissueSeal Plus than with BiClamp and Thunderbeat (H value, 24.9; p ≤ 0.0001).
Conclusion. The possibility of lateral heat transfer varies with the type of a tool and the maximum temperature on its branches. This investigation demonstrates that electrosurgical hemostasis using the TissueSeal Plus bipolar forceps shows a number of advantages over that with the BiClamp bipolar forceps and Thunderbeat for VH. TissueSeal Plus has demonstrated the safest coagulation with the lowest branch temperatures.
Keywords
In most countries of the world, hysterectomy is the most common gynecological operation performed for benign uterine diseases and for genital prolapse. According to various researchers, the rate of hysterectomy ranges from 25 to 38% of all gynecological operations [1, 2, 3]. Due to the relevance and importance of this operation, it is necessary to continue improving surgical approaches and methods of hemostasis. Safe and effective hemostasis is one of the most important factors in minimally invasive surgery [4, 5]. Intraoperative hemostasis may be achieved by using conventional suture ligation, as well as the electroligation. The main difficulties in performing vaginal hysterectomy (VH) without genital prolapse are associated with ligation of uterine vessels, as well as cardinal and uterosacral ligaments, since the clamping of these structures and their ligation is accompanied by certain difficulties due to the limited space for manipulation. Adequate visibility in the limited space for manipulation is an important factor for achieving successful hemostasis. The advantages of electrosurgical hemostasis using bipolar instruments (forceps, tweezers) include shorter operating time, ease of handling, reduced blood loss, and reduced postoperative pain [5]. These methods are more cost-effective due to the decrease in suture material and reduction in a bed-day which results from the reduced time and intensity of pain when using electrosurgical hemostasis.
Currently, electrosurgical energy is used for tissue coagulation, which occurs when the temperature exceeds a threshold of 42°C. Above this temperature, protein denaturation and subsequent tissue necrosis occur. Therefore, the temperature of the tissue heated to more than 42°C by electrosurgical instruments can cause damage to adjacent sensitive structures by expanding the zone of lateral thermal damage (LTD) [6]. In addition to hemostasis, bipolar coagulation also causes thermal damage to tissues. LTD probably occurs after each type of coagulation. The optimal method would be the one that provides good hemostatic results and prevent heat energy from extending the anatomical area where it is applied [7]. Modern bipolar electrosurgical instruments use a lower voltage and higher amperage than conventional bipolar instruments, and usually in energy pulsation mode, which makes it possible to cool tissues during the activation of the instrument and helps reduce lateral spread [8, 9]. More specifically, an electrosurgical generator has a feedback loop that monitors and calculates the impedance of tissues so that the voltage is constantly regulated. The feedback control system automatically stops the flow of energy to the branches of the instrument as soon as the coagulation cycle is completed. These advanced bipolar instruments are designed to reduce LTD, excessive charring and sticking of tissue to the branches of the instrument, and also to use lower temperatures for vascular coagulation in comparison with the conventional bipolar instruments. The Autostop function gives an audible alarm signal after the optimal coagulation is achieved. A significant advantage of this procedure is that the area of coagulation is limited by the area grasped with the instrument. LTD is minimized and thus the surrounding tissues must be protected. In many spheres, for example in gynecology, this aspect is beneficial in terms of safety. However, it necessary to seek the ways to improve electrosurgical hysterectomy and know the limitations to its use due to some specific complications that occur after this procedure (thermal burn of adjacent tissues and organs) [9, 10].
The purpose of this study was to study the risk of LTD by measuring the maximum temperature of branches of bipolar instruments used for hemostasis during VH.
Materials and Methods
In our study, three different electrosurgical instruments were used for surgical coagulation during VH. A comparative analysis of three types of surgical forceps for bipolar coagulation was conducted: the BiClamp with electric generator Erbe Vio (Germany), TissueSeal Plus Comfort with electric generator ARC–400 (BOWA, Germany) and Thunderbeat with generator Olympus (Japan). The temperature achieved by the instrument depends on a number of variables, including tissue type, tissue thickness, use of energy, and the power of instrument. These generators use active feedback to optimize output power. High-frequency coagulation instruments were used with a power of 40W, effect 3. The generated temperature was measured on the branches of instruments in the surgical area during coagulation of uterine vessels using Fluke TiS40 Infrared Camera with a resolution of 160×120 pixels.
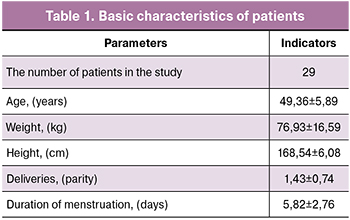 The study included 29 patients who underwent VH. The patients were randomly divided into three groups using the sealed envelope system: TissueSeal Plus Comfort was applied in 10 patients, the BiClamp instrument was used in 10 patients, and Thunderbeat was used in hemostasis of 9 patients. The basic characteristics of patients are presented in Table 1. Indications for hysterectomy were symptomatic uterine fibroids up to 15 weeks in size, adenomyosis, endometrial hyperplastic processes.
The study included 29 patients who underwent VH. The patients were randomly divided into three groups using the sealed envelope system: TissueSeal Plus Comfort was applied in 10 patients, the BiClamp instrument was used in 10 patients, and Thunderbeat was used in hemostasis of 9 patients. The basic characteristics of patients are presented in Table 1. Indications for hysterectomy were symptomatic uterine fibroids up to 15 weeks in size, adenomyosis, endometrial hyperplastic processes.
Patients with malignant diseases of the genital tract, symptomatic uterine fibroids for more than 15 weeks, and pelvic inflammatory diseases were not eligible for inclusion in the study.
The main indications for the operation were symptomatic uterine fibroids (48.43%), menstrual disorders in myoma and adenomyosis (28.57%), endometrial hyperplasia (28.57%), adenomyosis (17.86%), cervical elongation accompanied by uterine disease (fibroids, adenomyosis) (17.86%).
Statistical analysis
Statistical processing of the obtained data was performed using SPSS Statistics 17.0 software package. The distribution of quantitative indicators in the sample was estimated using the graphical method and the Shapiro-Wilk criterion, due to the small sample size. The equality of variances was assessed using Levene’s test. The distribution of quantitative indicators was different from normal, so nonparametric methods were used to describe them, the obtained data are presented as a median and quartile range Me (Q1; Q3). Qualitative indicators are presented in the form of absolute and relative values, n (%). The nonparametric Kruskal-Wallis test was used to compare temperatures recorded using an infrared camera. The obtained values of the Kruskal-Wallis criterion were compared with the critical value of Pearson’s chisquared distribution with the number of degrees of freedom df=2. The results were considered statistically significant at a significance level of p<0.05. In subsequent posteriori pairwise comparison of samples using the nonparametric MannWhitney test, the level of statistical confidence was adjusted (Bonferroni correction): p < 0.017.
Operative technique
VH consisted of conventional stages: radial dissection of the vaginal mucosa at the level of the vaults of the vagina, displacement of the bladder and rectum cranially, dissection of the vesico-uterine fold, performing anterior colpotomy. After performing posterior colpotomy, cardinal and uterosacral ligaments and uterine vessels were gradually severed using electroligation. The uterus was removed through the colpotomy opening after electroligation, ovarian ligaments and fallopian tubes were severed. If necessary, the uterus was fragmented. Morcellation, bisection and coring were performed for fragmentation of the myomatous uterus. All patients underwent bilateral salpingectomy; oophorectomy was performed according to indications. Next, hemostasis was monitored and the surgical wound closure was performed.
Results
The BiClamp instrument is cost-effective and can be used repeatedly; the electroligation procedure saves time and suture material. Effective and fast coagulation is provided by optimal synchronization of the instrument and the VIO generator [10]. The Autostop function is easy to use and gives optimal results. Tissue structures can be coagulated over a large area. Separate dissection of vessels is usually not necessary. The maximum temperature for effective hemostasis during ligation with the BiClamp instrument was 115.13°C. The minimum temperature when using BiClamp was 34.77°C. The temperature on the border of coagulation with the BiClamp instrument during electroligation of uterine vessels was 71.41°C. Interpretation of the obtained results shows that the use of bipolar coagulation with BiClamp has a maximum median temperature of 113.20°C. The median temperature on the border with coagulation was 71.65°C, and the minimum median temperature was 35.76°C.
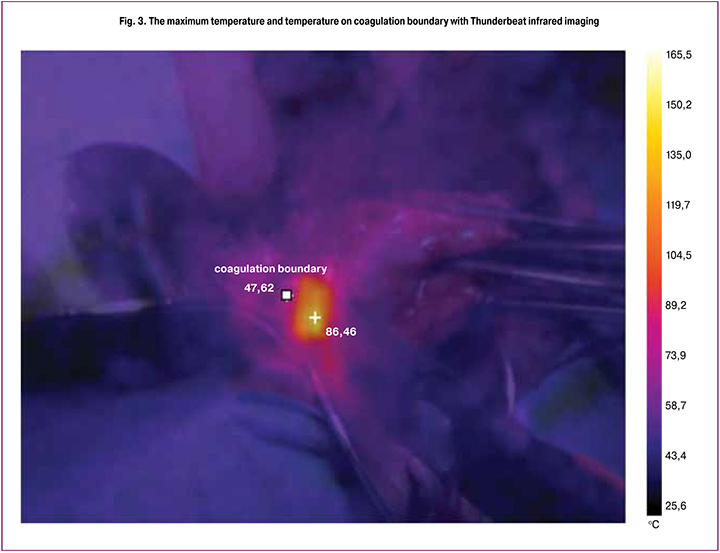
The maximum temperature on the branches during coagulation in the surgical area and on the border with coagulation in the study groups is shown in Fig. 1–3.

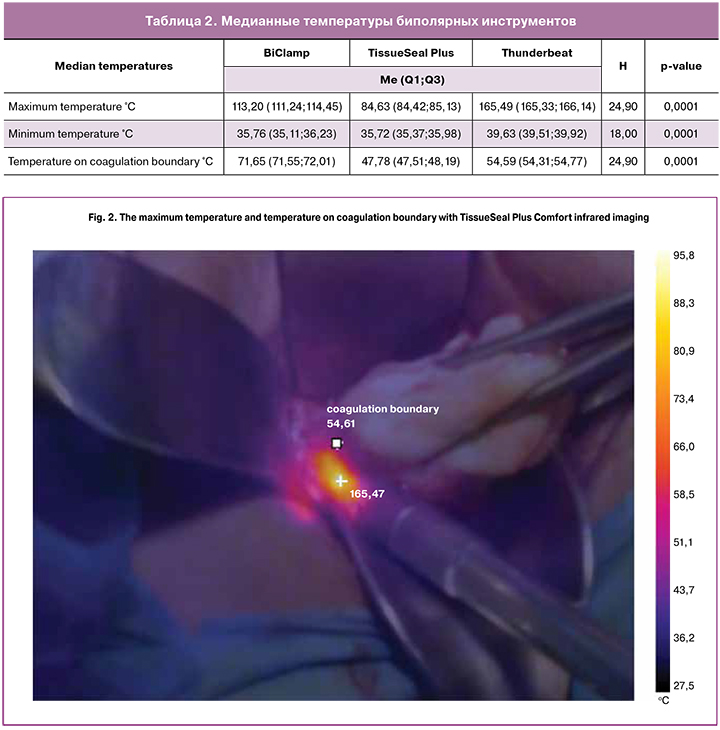
TissueSeal Plus Comfort is also a reusable instrument used in open surgery for ligation and characterized by minimal thermal spread due to the multi-layer construction of the working part of the branch, the socalled ‘sandwich’. Arteries, veins and tissue arrays up to 7 mm in diameter are quickly and safely coagulated by the clamp, special non-stick coating prevents the tissues from sticking to the working surface. The maximum temperature during ligation with TissueSeal Plus Comfort was 86.46°C (Fig. 2). The minimum temperature when using the TissueSeal Plus Comfort clamp was 35.88°C. Thus, the maximum median temperature was 84.63°C. The median temperature on coagulation boundary was 47.78°C, and the minimum median temperature was 35.72°C. During electroligation of uterine vessels, the temperature of the wound on coagulation boundary with the TissueSeal Plus Comfort instrument was 47.62°C.
Thunderbeat is an instrument that combines rapid tissue cutting and reliable vessel sealing. bipolar energy provides fast and secure hemostasis for vessels up to and including 7 mm in diameter. The maximum median temperature on branches of the instrument was 165.49°C, and the minimum median temperature in the area of coagulation spread was 39.63°C (Fig. 3). The maximum temperature of about 165°C can cause LTD and potential injury to adjacent organs. The device combines two energy modalities, ultrasonic energy and bipolar energy simultaneously and is used in the mode “seal and cut”. We used this device only in sealing mode, and tissue dissection was performed in the same way as in previous groups, that is with scissors. The temperature on coagulation boundary zone was 54.61°C. The median temperature on coagulation boundary was 54.59°C
Hemostasis with bipolar energy is characterized by three interdependent variables: compression, heating, and coagulation time. The purpose of this study was to investigate whether there are differences between bipolar methods of coagulation in VH, regarding the effectiveness of hemostasis and LTD. The present study demonstrates that the use of electrosurgical hemostasis using bipolar instrument TissueSeal Plus has a number of advantages over BiClamp and Thunderbeat in performing VH. Thus, the median maximum temperature of branches during electroligation with the BiClamp instrument was 113.20°C, and it was 71.65°C on coagulation boundary. During ligation with the Thunderbeat instrument, the temperature of branches was 165.49°C, and it was 54.59°C on coagulation boundary. When ligating with the TissueSeal clamp, the temperature of branches was 84.63°C, it was 47.78°C on coagulation boundary (p = 0.0001). Thus, the maximum median temperature on the branches of the instrument during electroligation and on coagulation boundary with intact tissue was significantly lower when using TissueSeal Plus than the BiClamp and Thunderbeat instruments (H value is 24.9, p ≤ 0.0001). The median temperature on coagulation boundary was also statistically significantly lower when using TissueSeal Plus than its analogs (H value is 24.9, p ≤ 0.0001). All three instruments demonstrated excellent hemostasis. The temperature values measured by infrared camera are shown in Table 2.
The advantages of the combined bipolar ultrasonic instruments include the decrease in movement of the instrument due to the combination of coagulation and simultaneous tissue cutting. Among disadvantages, there is a risk of LTD, as well as higher and longer temperatures at the tip of the instrument than other bipolar power sources, which can lead to lateral damage. LTD of adjacent anatomical structures can occur due to the spread of thermal energy outside the branches of the instrument. However, a lower heating temperature of the instrument reduces the likelihood of lateral damage to adjacent structures. The TissueSeal Plus instrument reduces the possibility of lateral damage due to the multi-layer sandwich-type construction.
Conclusion
An adequate electrosurgical instrument should be safe, fast, and effective to increase the efficiency of coagulation and reduce LTD. The balance between the temperature of the working part of the instrument and its effectiveness is of interest to both developers of medical equipment and surgeons.
References
- Ailamazyan E.K., Bezhenar V.F., Savitsky G.A., Niauri D.A., Popov E.N., Tsypurdeyeva A.A. et al. The rational choice of surgical approach for hysterectomy. J. Gynecol. Surg. 2006; 3 (Suppl. 1): S95-6.
- Беженарь В.Ф., Новиков Е.И., Василенко Л.В., Комличенко Э.В. Влагалищные операции. СПб.: Изд-во Н-Л; 2013. 151 с. [Bezhenar V.F., Novikov E.I., Vasilenko L.V., Komlichenko E.V. Vaginal surgery. Saint Petersburg: Publishing House N-L, 2013. 151 p. (in Russian)].
- Высоцкий М.М., Беженарь В.Ф., Овакимян М.А. Тотальная и субтотальная гистерэктомия: время развеивать мифы. Эндоскопическая хирургия. 2016; 6: 52-6. [Vysotsky M.M., Bezhenar V.F., Ovakimyan M.A. Total and subtotal hysterectomy: time to explode myths // Endoskopicheskaya Khirurgiya (Endoscopic Surgery). 2016; 6: 52-6. (in Russian)].
- Плеханов А.Н., Епифанова Т.А. Использование электрохирургии при влагалищной гистерэктомии. Ученые записки Санкт-Петербургского государственного медицинского университета им. акад. И.П. Павлова. 2017; 24(3): 22-7. [Plekhanov A.N., Epifanova T.A. The use of electrosurgery during hysterectomy// Uchenye Zapiski Sankt-Peterburgskogo Gosudarstbennogo Meditsinskogo Universiteta im. Akad. I.P. Pavlova (Transactions of the Acad. I.P. Pavlov Saint Petersburg State Medical University). 2017; 24 (3): 22-7. (in Russian)].
- Pogoreli Z., Kati J., Mrkliс I., Jeronci A., Susnjar T., Juki M. et al. Lateral thermal damage of mesoappendix and appendiceal base during laparoscopic appendectomy in children: comparison of the harmonic scalpel (Ultracision), bipolar coagulation (LigaSure), and thermal fusion technology (MiSeal). J. Surg. Res. 2017; 212: 101-7. https://dx.doi.org/10.1016/j.jss.2017.01.014.
- Hefermehl L.J., Largo R.A., Hermanns T., Poyet C., Sulser T., Eberli D. Lateral temperature spread of monopolar, bipolar and ultrasonic instruments for robot-assisted laparoscopic surgery. BJU Int. 2014; 114(2): 245-52. https://dx.doi.org/10.1111/bju.12498.
- Jun Liang, Huimin Xing, Yali Chang. Thermal damage width and hemostatic effect of bipolar electrocoagulation, LigaSure, and Ultracision techniques on goat mesenteric vessels and optimal power for bipolar electrocoagulation. BMC Surg. 2019; 19(1): 147. https://dx.doi.org/10.1186/s12893-019-0615-4.
- Amruta Jaiswal, Kuan-Gen Huang. Energy devices in gynecological laparoscopy – archaic to modern era. Gynecol. Minim. Invasive Ther. 2017; 6 (4):147-51. https://dx.doi.org/10.1016/j.gmit.2017.08.002.
- Zhu Q., Ruan J., Zhang L., Jiang W., Liu H., Shi G. The study of laparoscopic electrosurgical instruments on thermal effect of uterine tissues. Arch. Gynecol. Obstet. 2012; 285(6): 1637-41. https://dx.doi.org/10.1007/s00404-011-2207-0.
- Zubke W., Hornung R., Wässerer S., Hucke J., Füllers U., Werner C. et al. Bipolar coagulation with the BiClamp® forceps versus conventional suture ligation: a multicenter randomized controlled trial in 175 vaginal hysterectomy patients. Arch. Gynecol. Obstet. 2009; 280(5): 753-60. https://dx.doi.org/10.1007/s00404-009-1010-7.
Received 30.12.2019
Accepted 07.02.2020
About the Authors
Andrey.N Plekhanov, Doctor of Medicine of the I. P. Pavlov St. Petersburg State Medical University, Leading gynecologist of the Clinical Hospital of Russian Academy of Sciences. Tel. +7 (921)969-18-72. E-mail: a_plekhanov@mail.ru.6-8 Lev Tolstoy str., St. Petersburg, 197022, Russian Federation; 72 Morisa Toreza str., St. Petersburg, 194017, Russian Federation.
Vitaly. F Bezhenar, Professor, Doctor of Medicine, Head of the Gynecological Department of the I. P. Pavlov St. Petersburg State Medical University, Chief Specialist of the Health Ministry of Russia in the North-Western Regio, Chief Specialist of the Health Committee of Saint-Petersburg. E-mail: bez-vitaly@yandex.ru.
6-8 Lev Tolstoy str., St. Petersburg, 197022, Russian Federation.
Tatiana. A Epifanova, postgraduate student of the I. P. Pavlov St. Petersburg State Medical University, Gynecologist of the Clinical Hospital of Russian Academy of Sciences. Tel. +7(962)703-39-69. E-mail: epifanova-tatiana@mail.ru.
6-8 Lev Tolstoy str., St. Petersburg, 197022, Russian Federation; 72 Morisa Toreza str., St. Petersburg, 194017, Russian Federation.
Fedor. V Bezhenar. Gynecologist of the Clinical Hospital of Russian Academy of Sciences. E-mail: fbezhenar@gmail.com.
72 Morisa Toreza str., St. Petersburg, 194017, Russian Federation.
Yulia. S Shishkina, Gynecologist of the «SM – Clinic». E-mail: shyulia07@mail.ru.
47 Dunaiskii prospect, St. Petersburg, 192281, Russian Federation.
Nina A. Tatarova, Professor, Doctor of Medicine of the I. P. Pavlov St. Petersburg State Medical University. E-mail: Nina-tatarova@yandex.ru.
6-8 Lev Tolstoy str., St. Petersburg, 197022, Russian Federation
For reference: Plekhanov A.N., Bezhenar V.F., Epifanova Т.A.,
Bezhenar F.V., Shishkina IU.S., Tatarova N.A. Tissue thermometric characteristics in the intervention area during electrosurgical vaginal hysterectomy.
Akusherstvo i Ginekologiya/ Obstetrics and Gynecology. 2020; 5: 98-104 (In Russian).
https://dx.doi.org/10.18565/aig.2020.5.98-104