Воспалительные заболевания органов малого таза (ВЗОМТ) у женщин, в особенности хронические, являются серьезной не только медицинской, но и социально-экономической проблемой, обусловленной частотой этих заболеваний и осложнениями, связанными с потерей репродуктивной функции и снижением качества жизни.
Заболеваемость ВЗОМТ в России не известна, тогда как, например, в США ежегодно регистрируется 1,2 млн новых случаев [1]. В структуре гинекологической заболеваемости число пациентов с инфекционно-воспалительными процессами различной локализации занимает первое место, составляя 60–65% как во всем мире, так и в России.
Социальная значимость ВЗОМТ обусловлена высоким риском спаечной болезни, которая приводит к бесплодию, внематочной беременности и хронической тазовой боли. Прогнозируемая частота этих осложнений, основанная на компьютерной модели и учитывающая тяжесть инфекции, количество эпизодов ВЗОМТ и лечение, в когорте из 100 000 женщин в возрасте 20–24 лет, составляет 8550 случаев внематочной беременности, 16 800 – бесплодия и 18 600 – хронической тазовой боли [2].
Частота отдаленных осложнений ВЗОМТ повышается с увеличением числа эпизодов обострения заболевания. После первого эпизода бесплодие развивается у 15% женщин, а хроническая тазовая боль и эктопическая беременность – у 10%. Повторные эпизоды ВЗОМТ ассоциируются с 4–6-кратным повышением риска бесплодия [3]. В исследовании когорты женщин с лапароскопически подтвержденным сальпингитом частота бесплодия составляет 16%, из которых 67% связано с трубным фактором по сравнению с 2,7% – у женщин без сальпингита. Среди женщин с сальпингитом, которые забеременели, у 9% беременность была внематочной по сравнению с 1,9% в контрольной группе [4]. У женщин, перенесших два эпизода заболевания, частота хронической тазовой боли повышается до 30%, а у перенесших три и более – до 67% [3].
Экономические затраты (прямые медицинские расходы), связанные с осложнениями ВЗОМТ, составляют 2,7 млрд долларов, несмотря на то что большинство женщин получают помощь амбулаторно [5].
Клиническое течение ВЗОМТ в современных условиях отличается от клинической картины прошлых лет: редко развиваются классические формы заболевания; преобладают хронические процессы и первично-хронические формы со стойким рецидивирующим течением; чаще имеет место стертая клиническая картина как в острой, так и в хронической стадии; наиболее часто воспалительный процесс локализуется в придатках матки; редко поражается параметральная клетчатка и развиваются гнойные процессы [6].
Основным пусковым механизмом в развитии ВЗОМТ является микробная инвазия, в первую очередь, ИППП: C. trachomatis (30–37%) и N. gonorrhoeae (40–50%). Нередко играют роль аэробные бактерии родов Staphylococcus (53–56%) и Streptococcus (33%), а также условно-патогенная флора (G. vaginalis, E. coli, U. urealyticum) и анаэробные бактерии (20–56%). Важной особенностью хронических инфекций, поражающих половой тракт, является наличие смешанной аэробно-анаэробной флоры, ассоциированной с цитомегаловирусом (20%), вирусами простого герпеса (22%), папилломавирусами (16%), представителями класса Mollicutes (M. genitalium, U. urealiticum, M.hominis – 27%). В 15–20% случаев возбудитель ВЗОМТ выявить не удается [7, 8].
Факторами риска для ВЗОМТ являются: контакт с половым партнером, у которого выявлена хламидийная инфекция; бактериальный вагиноз; наличие двух и более половых партнеров в течение последних 6 месяцев; возраст моложе 25 лет; внутриматочные манипуляции в анамнезе; низкий социально-экономический статус; употребление алкоголя и наркотиков [5, 9].
Проблема ВЗОМТ усугубляется тем, что, несмотря на особое внимание, уделяемое ей в научно-практической литературе и общественном здравоохранении, диагностика заболевания существенно ниже ее реальной распространенности (около 60% пациентов с ВЗОМТ имеют бессимптомную форму заболевания), а своевременную медицинскую помощь в соответствии с доказательными рекомендациями получают менее 50% [10].
Успехов в профилактике ВЗОМТ и их осложнений достичь не удается. Молодые женщины, лечившиеся от ВОЗМТ, подвергаются риску нового заражения ИППП и/или ВЗОМТ в течение 48-месячного периода. Учитывая необходимость предотвращения будущих инфекций у этих уязвимых категорий пациентов, необходимо использовать стратегии снижения риска после постановки диагноза в долгосрочной перспективе [11].
Предотвращение ВЗОМТ и его осложнений рекомендуется осуществлять на трех уровнях [12, 13]:
- Первичная профилактика: наиболее эффективной мерой является профилактика ИППП – изменение стиля небезопасного сексуального поведения и использование контрацепции.
- Вторичная профилактика: предотвращение восходящего распространения инфекции из нижнего отдела генитального тракта в верхний. Скрининг на хламидийную инфекцию уменьшает риск ВЗОМТ у женщин примерно на 30–50% в течение 1 года. Женщин, у которых обнаружены Chlamydia tr. и которым поставлен диагноз неосложненной инфекции шейки матки, вызванной Chlamydia tr., следует рассматривать как лиц с наличием субклинической инфекции верхних отделов репродуктивного тракта и начинать лечение незамедлительно. Задержки лечения могут приводить к осложнениям (ВЗОМТ, внематочная беременность, бесплодие). В профилактических целях возможно селективное (превентивное или эпидемиологическое) лечение на основании эпидемиологических показаний пациентам с высоким риском. Лечение сексуальных партнеров имеет решающее значение в предотвращении повторного заражения.
- Третичная профилактика: предусматривает своевременное адекватное лечение инфекции верхних половых путей лекарственными средствами с доказанной эффективностью и тем самым предотвращение функционального и структурного повреждения маточных труб и других тазовых органов. Скрининг на реинфекции должен выполняться в период от 3 до 6 месяцев. Сексуальные партнеры женщин с ВЗОМТ должны быть обследованы на ИППП, в том числе партнеры за предыдущие 2 месяца.
Образование женщин, особенно подростков, имеет решающее значение. Консультирование должно включать информацию о преобладании бессимптомных инфекций и возможности возникновения эпизодов ВЗОМТ в результате будущих инфекций. Кроме того, врачи могут влиять на риск заражения путем предоставления консультирования о сексуальном поведении мужчин и женщин, необходимости своевременного обращения за медицинской помощью, соблюдении правил приема антибактериальных и других лекарственных средств во время лечения, выявлении других инфицированных лиц и о контрацептивной практике [14, 15].
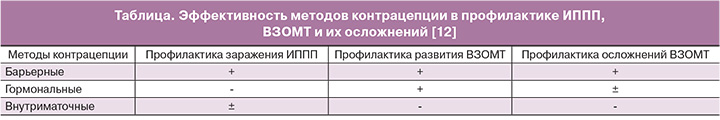
Использованию противозачаточных средств как методу предотвращения не только нежеланной беременности, но и профилактики ИППП, ВЗОМТ и их осложнений, должно уделяться особое внимание.
Существующие методы контрацепции в разной степени эффективны для этих целей (таблица) [12].
Барьерные методы
В настоящее время существует только один метод – презерватив, который, несмотря на свою тысячелетнюю историю, является современным методом контрацепции и формой многоцелевых профилактических технологий, защищая не только от беременности, но и многих ИППП, включая ВИЧ. Контрацептивная эффективность его достаточно высока при правильном использовании (индекс Перля – 2), защита от ИППП также высока, хотя и не в 100% случаев.
S. Weller и K. Davis (база данных Кокрейна) дали оценку заболеваемости ВИЧ, относительный риск которой составил 1,14 (95% ДИ: 0,56–2,04) на 100 человеко-лет среди обследуемых, которые «всегда» использовали презерватив, что соответствует общей эффективности (пропорциональному снижению ВИЧ-сероконверсии) около 80% [16].
Среди последовательных пользователей презерватива у 13,3% была диагностирована C. trachomatis по сравнению с 34,4% использовавших их нерегулярно [17]. В исследовании W. Lee и соавт. среди участников, которые использовали презервативы постоянно и без погрешностей, никто не приобрел гонореи или хламидиоза против 13,3% участников, которые приобрели инфекцию и сообщили о проблемах в процессе применения [18].
R.L. Winer и соавт. сообщают, что инфицирование женщин ВПЧ при постоянном использовании презерватива наступала у 37,8 %, а у женщин, его не использовавших – 89,3% [19]. R.A. Crosby и соавт. приводят данные, что 31,1% случаев заражение половыми инфекциями связано с механическими повреждениями мужских презервативов и/или его соскальзыванием [20].
В связи с вышеизложенным не вызывает сомнений, что защитные свойства презерватива напрямую зависят от правильности его использования.
Пероральные гормональные контрацептивы
Современные данные по использованию комбинированных оральных контрацептивов (КОК) свидетельствуют о более низком риске клинически выраженного ВЗОМТ по сравнению с данными прошлых лет [21]. В 1980 г. опубликована обзорная работа, в которую было включено 10 исследований, на основании которых был сделан вывод, что КОК оказывают защитное влияние в отношении ВЗОМТ [22]. В дальнейшем многоцентровое исследование, выполненное P. Wolner-Hanssen и соавт., продемонстрировало, что прием КОК снижает риск ВЗОМТ почти на 50% (ОР=0,51) и даже при наличии хламидийной инфекции – на 78% (ОР=0,22). КОК оказались эффективными в предотвращении ВЗОМТ по сравнению с отсутствием контрацепции (ОР=0,17), с другими методами (ОР=0,22, p=0,1) и с барьерными методами (ОР=0,24, p=0,09) [23]. Другими авторами также отмечено снижение риска ВЗОМТ на 50–76% на фоне приема КОК [24, 25].
По обобщенным данным эпидемиологических исследований, риск сальпингоофоритов снижается на 50–80% в сравнении с женщинами, использующими барьерные методы контрацепции или не использующими контрацепцию, а риск эктопической беременности – на 90% [26]. При этом риск госпитализации по поводу развития осложненного ВЗОМТ, хирургического вмешательства, эктопической беременности и бесплодия снижается в 2 раза [26, 27]. Если на фоне приема КОК развивается ВЗОМТ, то имеется высокая вероятность снижения его степени тяжести и развития осложнений, но при этом возможно наличие субклинических форм [23, 28, 29].
Установлено, что у пользовательниц КОК ВЗОМТ, вызванные гонококковой инфекцией, развиваются гораздо реже, чем у тех, кто их не использовал – 32 против 76% (ОШ=0,42) [30].
К настоящему времени накоплено значимое количество эпидемиологических и клинико-микробиологических данных, свидетельствующих о протективной роли КОК в отношении БВ, обобщенных в трех метаанализах. По данным C. Bradshaw и R. Brotman [31], использование гормональной контрацепции коррелирует с достоверно более низкой распространенностью БВ (ОР=0,73). В другом метаанализе был сделан вывод, что среди женщин, использовавших гормональные методы (КОК, чистые прогестины и др.), риск БВ был снижен на 20% (ОР=0,82), а вероятность его рецидива – на 30% (ОР=0,69) [32].
Протективный эффект наблюдается сразу, а максимальный достигается через 12 мес. приема КОК, при этом защита ограничивается текущим использованием препарата и погрешностями его применения [33].
Один из авторов исследований, проф. G. Rubin, медицинский эпидемиолог CDC, признал защиту от ВЗОМТ одним из наиболее важных неконтрацептивных преимуществ оральных контрацептивов [25] и заявил, что они обеспечивают протекцию от системного воспалительного ответа.
По мнению исследователей, основой протективного эффекта КОК в отношении ВЗОМТ является препятствие восходящему инфицированию и проникновению патогенов в матку за счет следующих механизмов [15, 24, 26, 28, 32–35]: изменение анатомических пропорций шейки матки (уменьшение диаметра, увеличение длины) и сгущение цервикальной слизи; уменьшение вероятности ретроградного заброса крови (и инфектов) в брюшную полость вследствие прекращения перистальтики маточных труб и снижения объема менструальной кровопотери; отсутствие периовуляторного колебания выработки противомикробных дефензинов (катионных антимикробных пептидов), обладающих прямым противомикробным, антиэндотоксиновым, иммуномодулирующим действием, обеспечивающих хемотаксис, протеазную активность, опсонизацию и фагоцитоз микробных агентов; усиление барьерных свойств нижнего отдела урогенитального тракта путем прямого или косвенного влияния на микробиом и/или локальный иммунитет.
Кроме того, при генерализации инфекции уменьшается избыточность воспалительного ответа вследствие системного противовоспалительного и иммуномодулирующего действия прогестагенного компонента КОК [36].
С учетом описанных механизмов становится очевидно, что протективный эффект КОК в отношении ВЗОМТ будет выше при отсутствии менструальноподобных кровотечений. С этой точки зрения для женщин из группы риска наиболее предпочтительными могут быть пролонгированные режимы использования КОК, позволяющие сократить их количество.
Инновационный КОК, содержащий 20 мкг этинилэстрадиола и 3 мг дроспиренона (ЭЭ/ДРСП) во флекс-картридже, сочетает в себе высокий контрацептивный эффект и уникальную возможность увеличения длительности менструального цикла с учетом собственных предпочтений пользователей. Такая возможность обеспечивается гибким режимом контроля кровотечений на протяжении вариабельного числа циклов (минимум – 3, максимум – 13 за 1 календарный год). При описанном режиме после обязательной фазы (24 дня – прием, 4 дня – перерыв) прием препарата продолжают от 24 дней (минимум) до 120 дней (максимум) по выбору самой женщины благодаря входящему в комплект дозатору «Клик (Clyk)» и, таким образом, уменьшают частоту менструальноподобной реакции [37]. Кроме того, благодаря звуковой системе оповещения женщины почти в 3 раза реже пропускают прием таблеток.
Разработка препарата ЭЭ/ДРСП во флекс-картридже связана с социокультурным феноменом постиндустриального мира: в высокоразвитых странах до 59% женщин в возрасте 15–49 лет заинтересованы в применении режима, позволяющего избежать ежемесячных менструальных кровотечений [38]. Так, согласно опросу большинство респондентов отмечают, что менструальные кровотечения оказывают влияние на их половую жизнь (75,6%), работу (28,2%) и занятия спортом (48,4%) [39]. При этом до 46% женщин предпочли бы, чтобы менструаций вообще не было [40]. Среди россиянок около 30%, принимающих КОК, хотя бы раз пользовались пролонгированным режимом, а 15% планируют его использовать [41].
С терапевтической позиции это выгодно для обеспечения надежной контрацепции, профилактики восходящего инфицирования и достижения более выраженного эффекта в отношении дисменореи и предменструального синдрома, чем при использовании стандартных режимов [41, 42].
Согласно результатам международного многоцентрового (37 центров) открытого рандомизированного контролируемого исследования применение гибкого пролонгированного режима сопровождается достоверным снижением числа дней кровотечений отмены и кровянистых выделений по сравнению с приемом той же комбинации КОК в стандартном 28-дневном режиме (41,0 против 65,8 дней соответственно, р<0,0001) и той же комбинации в фиксированном пролонгированном 124-дневном режиме (60,9 дня). Гибкий пролонгированный режим приводит к снижению доли дней с кровотечением или кровянистыми выделениями на одну треть по сравнению с указанными выше режимами – 13,3, 23,1 и 20,4% соответственно [37].
ВЗОМТ являются одной из частых причин хронической тазовой боли, которая характеризуется как боль в области таза в течение не менее 6 месяцев с достаточной интенсивностью, чтобы повлиять на нормальную повседневную деятельность и требующая медицинской помощи. Такая боль может усиливаться во время менструаций. Боли в этих случаях появляются перед началом менструации, а с ее появлением интенсивность их снижается. Менструальная кровь может иметь неприятный запах, а в области придатков определяется болезненность. С другой стороны, первичная дисменорея может усиливаться при присоединении ВЗОМТ. В обоих случаях симптоматическое лечение, направленное на сокращение количества менструаций будет иметь положительное влияние.
Действительно, эффективность режима ЭЭ/ДРСП во флекс-картридже, оцененная в открытом рандомизированном контролируемом многоцентровом исследовании у женщин 18–40 лет с первичной дисменореей от умеренной до тяжелой степени тяжести, по сравнению с обычным режимом 24/4 была выше (11 дней против 15 дней; разница -4,2 дня [95% ДИ: -6,5 – -2,0]; р=0,0003). Применение ЭЭ/ДРСП во флекс-картридже позволяет уменьшить количество дней с тазовой болью, ассоциированной с кровотечением отмены (разница в -4,1 дня; 95% ДИ: -5,8 – -2,4). Снижается также количество дней с тазовой болью независимо от возникновения кровотечения (разница -3,4 дня; 95% ДИ: -5,9 – -0,9) и дней, в течение которых тазовая боль мешает повседневной активности (разница -2,2 дня; 95% ДИ: -4,2– -0,1) [43].
Таким образом, при пролонгированном режиме приема КОК удлинение «менструального цикла» с отсутствием периовуляторных структурно-функциональных изменений, снижение интенсивности менструальной кровопотери и увеличение суммарного действия прогестагенного компонента как средства с потенциальными противовоспалительными свойствами повышает протективный потенциал в отношении риска ВЗОМТ.
Внутриматочные средства
В литературе последних лет имеются сведения о снижении риска ВЗОМТ при использовании последнего поколения ВМС (левоноргестрел-содержащие и медь-содержащие с максимальным содержанием меди – T-Cu 380A) без существенной разницы между ними по сравнению с типами ВМС, использовавшимися в предыдущие годы [44, 45].
Проведение скрининга на наличие ИППП в момент введения ВМС по сравнению со скринингом перед проведением этой процедуры не показало существенной разницы в риске ВЗОМТ [46]. Введение ВМС у женщин с недиагностированной хламидийной инфекцией или гонореей увеличивало абсолютный риск ВЗОМТ незначительно (0–5% для лиц с ИППП и 0–2% – без них) [47]. Наличие ВМС в момент постановки диагноза острого ВЗОМТ не влияет на результаты лечения, и удаление ВМС не требуется [48, 49].
Обобщенные результаты исследований были представлены на Конгрессе Европейского общества по контрацепции в Праге в 2008 году, на основании которых сделаны следующие рекомендации [50]: перед введением ВМС рутинный скрининг на ИППП во всех случаях и профилактическое применение антибиотиков не рекомендуется (уровень доказательств II-3); диагностические тесты должны быть сделаны, если выявлен высокий риск ИППП или присутствуют клинические симптомы инфекции; при выявленной инфекции введение ВМС необходимо отложить до выздоровления (II-2); женщины с туберкулезом тазовых органов, послеродовым сепсисом и септическим абортом относятся к категории 3–4 (высокий риск) по критериям приемлемости методов контрацепции ВОЗ как для начала, так и для продолжения использования ВМС.
Заключение
Профилактические меры, направленные на предотвращение заражения ИППП и распространение микроорганизмов в верхние отделы полового тракта, могут существенно снизить последствия инфекционно-воспалительных заболеваний половых органов у женщин. Препарат с гибким пролонгированным режимом, содержащий ЭЭ/ДРСП, во флекс-картридже имеет преимущество в профилактике ВЗОМТ по сравнению с другими уже доказавшими свою эффективность гормональными препаратами, заключающееся в меньшем количестве дней кровотечения, что повышает его протективный потенциал в отношении риска ВЗОМТ.