В Российской Федерации (РФ) за время наблюдения количество случаев ВИЧ-инфекции среди женщин достигло 585 083. Причиной вовлечения женщин в эпидемию ВИЧ-инфекции является преобладание полового пути заражения (86,7%). В 2021 г. доля женщин среди всех живущих с ВИЧ россиян составила 37,6%, а в структуре новых случаев – 40,5%. За время наблюдения в РФ ВИЧ-инфицированными матерями рождено 244 092 живых детей, у 12 425 из них была подтверждена ВИЧ-инфекция. Известно, что женщины, живущие с ВИЧ, подвержены большему риску осложнений беременности, родов и смертности во время беременности и в послеродовом периоде, чем женщины без ВИЧ [1–3]. В мире на долю ВИЧ-инфицированных женщин приходится 6–20% всех случаев материнской смертности [4]. В Санкт-Петербурге доля женщин, живущих с ВИЧ, в структуре материнской смертности достигала 46% в 2015 г., и только с 2019 г. отмечается ее стойкое снижение до 3–7% [5]. Высокая частота коморбидности у ВИЧ-инфицированных женщин репродуктивного возраста определяет необходимость планирования беременности у пациенток, заинтересованных в ее наступлении, и применения безопасной и эффективной контрацепции, если рождение ребенка не планируется [6–9].
Предотвращение нежелательной беременности среди женщин, живущих с ВИЧ, путем обеспечения им доступа к целому ряду вариантов контрацепции и оказания поддержки в поиске метода, который наилучшим образом соответствует их предпочтениям, важно для дальнейшего снижения материнской смертности в условиях высокой распространенности ВИЧ и ликвидации детской ВИЧ-инфекции. Согласно Глобальной стратегии по СПИД на 2021–2026 гг. «Ликвидировать неравенство, покончить со СПИДом», к 2025 г. 95% женщин должны получать необходимые услуги по профилактике, диагностике и лечению ВИЧ-инфекции, а также услуги по охране сексуального и репродуктивного здоровья [10].
Всем ВИЧ-инфицированным женщинам рекомендуется проводить консультирование по планированию беременности, в ходе которого необходимо обсудить репродуктивное здоровье и намерение женщины в отношении беременности, а также предоставить информацию об эффективных и подходящих методах контрацепции для снижения вероятности незапланированной беременности [11, 12]. Важно отметить, что женщинам с состояниями, при которых незапланированная беременность представляет угрозу здоровью, включая ВИЧ-инфекцию, нельзя ограничиваться барьерными и ритмическими методами или прерванным половым актом из-за их низкой эффективности и повышенного риска осложнений беременности и родов [6]. В настоящее время ВИЧ-инфекция не является противопоказанием для любых методов контрацепции, однако следует учитывать лекарственные взаимодействия между гормональными контрацептивами и антиретровирусными препаратами [13].
Сегодня две трети женщин, живущих с ВИЧ, – это пациентки репродуктивного возраста, из которых половина не исключает наступления беременности в ближайшее время или в будущем; вторая половина не заинтересована в наступлении беременности и нуждается в эффективной и безопасной контрацепции [14, 15]. Наиболее высокий уровень защиты от нежеланной беременности обеспечивают гормональные методы планирования семьи, а их применение в течение 3 лет на 25–30% снижает материнскую и на 40% – детскую смертность [6].
Результаты большинства исследований не выявили связи между использованием гормональных контрацептивов и прогрессированием ВИЧ-инфекции (снижение количества CD4-лимфоцитов, увеличение вирусной нагрузки ВИЧ в крови и смертности), а также снижением эффективности антиретровирусной терапии (АРТ). Проспективное когортное исследование, проведенное в Санкт-Петербургском ГБУЗ «Центр по профилактике и борьбе со СПИД и инфекционными заболеваниями» (далее – Центр СПИД) совместно с CDC (Centers for Disease Control and Prevention) с участием 709 ВИЧ-инфицированных женщин репродуктивного возраста, показало, что использование депо медроксипрогестерона ацетата (ДМПА) не было связано со статистически значимым повышением риска прогрессирования заболевания по сравнению с использованием негормональных методов (AHR 1,28; 95% ДИ 0,71–2,31) [9]. Установлено, что применение чисто прогестиновых контрацептивов, включая пролонгированные методы контрацепции, не увеличивает восприимчивость к ВИЧ и контагиозность; поэтому ВИЧ-инфицированным женщинам следует предлагать гормональные методы контрацепции, которые наилучшим образом отвечают их потребностям [7, 9, 16, 17]. Интересные данные были получены в результате исследования MTN-020/ASPIRE, посвященного использованию методов обратимой контрацепции длительного действия у женщин, живущих с ВИЧ. Установлено, что пролонгированные методы контрацепции имеют самые высокие показатели продолжительности использования в течение 12 месяцев наблюдения. Наиболее частое и длительное применение отмечено у имплантатов и медьсодержащих внутриматочных средств (ВМС), в связи с чем данные методы рекомендуется предлагать для использования ВИЧ-инфицированным женщинам [18]. Систематический обзор по сравнению применения методов контрацепции у ВИЧ-инфицированных и не инфицированных ВИЧ женщин продемонстрировал более высокие показатели продолжения контрацепции среди ВИЧ-инфицированных, по сравнению с неинфицированными. Показано, что длительность использования высокоэффективных методов контрацепции является одним из показателей охраны репродуктивного здоровья у женщин с ВИЧ-инфекцией. Во всех исследованиях длительность применения контрацептивов различалась в зависимости от метода контрацепции: отмечена высокая частота продолжения применения имплантатов (≥86%) и медьсодержащих ВМС (51–91%). На основании проведенного анализа исследований сделан вывод о необходимости проведения дополнительных исследований по применению методов планирования семьи и увеличению интеграции концепции репродуктивного здоровья в систему оказания помощи людям, живущим с ВИЧ [19].
Согласно данным популяционного исследования, в Российской Федерации 85% женщин фертильного возраста используют тот или иной метод планирования семьи [6, 7]. Чаще всего в России в качестве метода контрацепции выбирают презервативы (45%), противозачаточные таблетки (30%) и прерванный половой акт (23%). Данные о частоте применения методов контрацепции у людей, живущих с ВИЧ, ограничены. Каждая пятая ВИЧ-инфицированная женщина (20%) и каждый четвертый ВИЧ-инфицированный мужчина (26%), имеющие регулярные половые контакты, не используют никаких методов контрацепции. Основной причиной отказа от планирования беременности и у мужчин, и у женщин являются неудовлетворительное материальное положение и наличие ВИЧ-инфекции. Несмотря на то что 80% женщин, живущих с ВИЧ, не исключают беременность в неопределенном будущем, а 16% совсем ее не планируют, только 8% применяют гормональную контрацепцию, что существенно реже, чем в группе женщин без ВИЧ. При этом частота использования барьерной контрацепции и прерванного полового акта как метода регулирования рождаемости сопоставима с неинфицированными ВИЧ (48 и 18% соответственно) [20]. Определяющим фактором в выборе метода предупреждения нежелательной беременности является консультирование, после которого 75% женщин, использовавших ранее негормональную контрацепцию, сделали выбор в пользу гормональной контрацепции. Высокую приверженность выбранному методу контрацепции обеспечивают такие свойства, как простота и удобство применения, отсутствие связи с половым актом, высокая эффективность и минимум побочных эффектов [6].
Согласно данным другого исследования, в РФ востребованность в получении услуг по планированию семьи определяется большой долей ВИЧ-инфицированных женщин (52,6%), не заинтересованных в наступлении беременности в ближайшей и отдаленной перспективе [17, 21]. В данной группе подавляющее большинство женщин (96,3%) имели опыт использования презервативов, каждая третья (29,4%) – оральных контрацептивов, ни одна не использовала ДМПА, и только 4% ранее применяли ВМС. Прерванный половой акт как метод контрацепции использовали ранее 41% респондентов. Важно отметить, что после проведенного обследования большинство женщин не имели противопоказаний к использованию комбинированных оральных контрацептивов (КОК) (89%) и ДМПА (94%) согласно Медицинским критериям приемлемости ВОЗ (табл. 1).
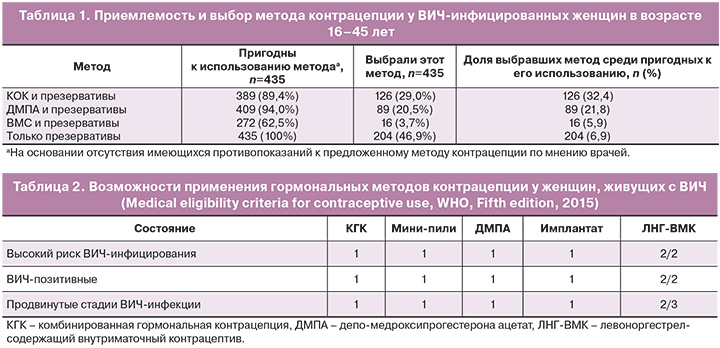
Более половины женщин (54,6%), не имевших противопоказаний к использованию высокоэффективной контрацепции (КОК, ДМПА или ВМС), выбрали один из этих методов в сочетании с презервативами. На основании проведенного мультифакторного анализа показано, что чаще выбирали высокоэффективные методы планирования семьи женщины, родившие двух и более детей (отношение коэффициентов распространенности (ОКР)=1,4), находившиеся в послеродовом периоде (ОКР=1,3), планировавшие или не исключавшие беременность в будущем (ОКР=1,4 и 1,3 соответственно), ранее использовавшие оральные контрацептивы (ОКР=1,3), в недавнем прошлом употреблявшие наркотические средства (ОКР=1,3), ни разу не использовавшие презервативы в течение последнего года (ОКР=2,3) или использовавшие изредка (ОКР=1,9). Выбор КОК ВИЧ-инфицированными женщинами связан с планированием беременности в будущем (ОКР=2,1), применением оральных контрацептивов в прошлом (ОКР=1,5), отсутствием использования барьерной контрацепции в течение предшествовавшего года (ОКР=3,7). Важным фактором выбора ДМПА вместе с презервативами в сравнении с выбором только презервативов было употребление инъекционных наркотиков в недавнем прошлом (ОКР=1,6) [17, 21, 22, 23].
Применение методов планирования семьи у пациенток с хроническими вирусными инфекциями, включая ВИЧ-инфекцию и хронические вирусные гепатиты С и В, определяется национальными медицинскими критериями приемлемости методов контрацепции, которые представляют собой адаптированный документ «Медицинские критерии приемлемости использования методов контрацепции ВОЗ, 5-е издание, 2015» [6, 7]. Рекомендации по использованию гормональной контрацепции женщинами с высоким риском ВИЧ-инфекции, ВИЧ-инфицированными женщинами и ВИЧ-инфицированными женщинами, получающими АРТ, были пересмотрены ВОЗ в 2015 г. и отражены в 5-м издании «Медицинских критериев приемлемости для использования методов контрацепции». Согласно медицинским критериями приемлемости методов контрацепции, женщины, живущие с ВИЧ, независимо от стадии заболевания, включая продвинутые, могут использовать следующие методы гормональной контрацепции без ограничений: КОК, комбинированные инъекционные контрацептивы (КИК), комбинированные контрацептивные пластыри и кольца, только прогестаген-содержащие таблетки (ПСТ), только прогестаген-содержащий инъекционный контрацептив (ПСИК: ДМПА и норэтистерона энантат – НЭТ-ЭН), а также имплантаты с левоноргестрелом (ЛНГ) (в настоящее время данный препарат не имеет регистрации на территории РФ) и этоногестрелом (ЭТГ). Все перечисленные методы относятся к первой категории приемлемости – состояние, при котором нет ограничений для использования данного метода контрацепции [6, 7] (табл. 2).
При выборе гормонального метода контрацепции ВИЧ-инфицированными женщинами, получающими АРТ, необходимо учитывать возможные межлекарственные взаимодействия. Женщины, принимающие любой из нуклеозидных ингибиторов обратной транскриптазы (НИОТ), могут использовать все методы гормональной контрацепции без ограничений: КОК, КИК, комбинированные контрацептивные пластыри и кольца, ПСТ, ПСИК (ДМПА и НЭТ-ЭН), а также имплантаты с ЛНГ и ЭТГ (категория 1). Женщины, принимающие ненуклеозидные ингибиторы обратной транскриптазы (ННИОТ) – эфавиренз или невирапин, обычно могут использовать комбинированные контрацептивные пластыри и кольца, ПСТ, НЭТ-ЭН, а также имплантаты ЛНГ и ЭТГ (категория 2 – состояние, при котором преимущества использования метода в целом превалируют над теоретическими или доказанными рисками). Женщины, принимающие эфавиренз или невирапин, могут использовать ДМПА без ограничений (категория 1). Женщины, принимающие новейшие ННИОТ, содержащие этравирин и рилпивирин, могут использовать все методы гормональной контрацепции без ограничений (категория 1) [6, 7]. Более подробно межлекарственные взаимодействия антиретровирусных препаратов и гормонов, входящих в состав гормональных контрацептивов, описаны в последней версии рекомендаций европейского общества по изучению ВИЧ-инфекции EACS (European AIDS Clinical Society, 12,0, 2023) [24]. Так, например, имплантат с ЭТГ не имеет значимых межлекарственных взаимодействий с препаратами, относящимися к группе ингибиторов интегразы, и с современными ННИОТ (рилпивирин – RPV). Бустированные ритонавиром ингибиторы протеазы и эфавиренц (EFV) могут уменьшить воздействие прогестина и тем самым снизить эффективность метода контрацепции; поэтому в таких случаях может потребоваться применение барьерной контрацепции дополнительно.
Настоящий этап эпидемии ВИЧ-инфекции характеризуется фазой тяжелых и коморбидных состояний, структура которых меняется во времени. Один из актуальных аспектов коморбидности – сочетание ВИЧ-инфекции и хронического гепатита С, особенно у женщин детородного возраста (30–40%) [25]. Кроме того, нельзя не учитывать высокий риск перинатальной передачи вируса гепатита С от матери к ребенку, особенно если у беременной женщины протекает коинфекция ВИЧ и хронический гепатит С, где риски перинатальной передачи вируса гепатита С возрастают до 14–16%. Возможности применения гормональной контрацепции у женщин с вирусными гепатитами также представлены в медицинских критериях приемлемости методов контрацепции ВОЗ и национальных медицинских критериях. Известно, что прогестиновые контрацептивы метаболизируются в печени, и их использование потенциально может негативно сказаться на функции печени; однако это в значительной степени меньше, чем при использовании КОК [7].
Большинство беременностей у ВИЧ-инфицированных женщин, наблюдающихся в Центре СПИД, являются желанными (93%). Низкое число нежеланных беременностей связано с реализацией программы по планированию семьи среди ВИЧ-инфицированных женщин в Санкт-Петербурге [22]. Она внедрена в оказание услуг Центра СПИД с 2007 г. при участии международного проекта по репродуктивному здоровью ВИЧ-инфицированных женщин, а с 2011 г. – в рамках территориальной программы, когда на основании фармакоэкономического обоснования начали закупаться современные средства контрацепции (КОК, ДМПА, имплантаты («Импланон НКСТ»), медьсодержащая ВМС, средства барьерной контрацепции) для предоставления ВИЧ-инфицированным пациентам, наблюдающимся в Центре СПИД. В настоящее время накоплен опыт применения различных методов контрацепции у женщин, живущих с ВИЧ, включая использование пролонгированного гормонального контрацептива с ЭТГ в форме имплантата.
В настоящее время в РФ разрешен к применению единственный подкожный контрацептивный имплантат (рентгенконтрастный имплантат, 68 мг ЭТГ, ЛП-000317) Импланон НКСТ. Данные по применению данного метода контрацепции у женщин, живущих с ВИЧ, в отечественных и зарубежных литературных источниках ограничены, в связи с чем, в рамках нашего исследования выполнен анализ применения препарата в данной группе пациенток.
Собственные данные
В исследование была включена 41 ВИЧ-инфицированная пациентка, наблюдавшаяся в Центре СПИД. Период исследования – 2016–2023 гг.
Все женщины соответствовали следующим критериям включения в исследование:
- репродуктивный возраст (18–45 лет);
- подтвержденный диагноз ВИЧ-инфекция;
- обследование на хронические вирусные гепатиты В и С;
- сексуально-активные в течение последнего года;
- отсутствие заинтересованности в наступлении беременности в течение 12 месяцев и более;
- отсутствие противопоказаний для использования имплантата с ЭТГ;
- подписанное информированное согласие для применения контрацептивного рентгеноконтрастного имплантата, содержащего 68 мг ЭТГ;
- диспансерное наблюдение в Центре СПИД на всех этапах исследования (консультирование по планированию семьи и выбору метода контрацепции, введение контрацептивного рентгеноконтрастного имплантата, содержащего 68 мг ЭТГ, наблюдение при его использовании, удаление контрацептивного рентгеноконтрастного имплантата, содержащего 68 мг ЭТГ, последующее наблюдение).
Все женщины до включения в исследование были консультированы гинекологами Центра СПИД по вопросам планирования семьи и выбора метода контрацепции. В ходе консультации пациенткам предоставлялась полная информация обо всех одобренных в РФ методах контрацепции, на основании которой женщины делали выбор наиболее предпочтительного контрацептива. Также были даны рекомендации по использованию презервативов для профилактики передачи ВИЧ и заражения инфекциями, передаваемыми половым путем. После консультации оценивались предпочтения в области контрацепции, женщин просили выбрать из предложенных методов все те, которые они хотели бы использовать, если бы они были предоставлены бесплатно. После изучения истории болезни, проведения физикального и гинекологического осмотров и получения результатов лабораторных исследований биологических образцов (клинический, биохимический анализы крови, уровень РНК ВИЧ в крови, количество CD4-лимфоцитов) клиницисты оценивали возможность пациентки использовать выбранный метод контрацепции на основании национальных медицинских критериев приемлемости методов контрацепции [6, 7]. В исследование включались пациентки, выбравшие с целью контрацепции имплантат с ЭТГ (Импланон НКСТ), который предоставлялся бесплатно за счет территориальной программы. После выбора метода контрацепции женщины были опрошены для сбора демографической, репродуктивной, поведенческой информации и информации, связанной с ВИЧ-инфекцией.
Анализ анамнестических данных проводился на основании информации, полученной из медицинских карт ВИЧ-инфицированных женщин.
Собраны данные:
- о социально-демографическом статусе (возраст, потребление психоактивных веществ);
- репродуктивном и гинекологическом анамнезе: количество беременностей в анамнезе, их исходы, применение контрацепции и гинекологические заболевания в анамнезе;
- эпидемиологическом анамнезе: путь инфицирования ВИЧ, наличие/отсутствие хронического вирусного гепатита С, ВИЧ-статусе полового партнера.
- анамнезе заболевания: длительность инфицирования ВИЧ, стадия ВИЧ-инфекции, АРТ.
Проводился физикальный осмотр с измерением АД, пульса, веса перед началом использования метода контрацепции и в динамике в период его применения, гинекологический осмотр. В ходе использования препарата Импланон НКСТ оценивались побочные эффекты и нежелательные явления на фоне применения, причины прекращения использования метода, осложнения при введении/удалении имплантата.
Лабораторное обследование включало:
- общий клинический анализ крови, выполненный на автоматическом 5-Diff гематологическом анализаторе Sysmex XN 1000 (Sysmex Europe GmbH, Германия);
- биохимический анализ крови (аланинаминотрансфераза (АЛТ), аспартатаминотрансфераза (АСТ), общий билирубин, глюкоза), выполненный на автоматическом биохимическом анализаторе Cobas c501 (Roche, Швейцария);
- определение уровня РНК ВИЧ в крови методом полимеразной цепной реакции проводили с помощью автоматизированного комплекса Abbott m2000 RealTimeSystem с использованием тест-систем Abbott RealTime HIV-1 методом полимеразной цепной реакции на обратную транскриптазу (RT-PCR) in vitro для определения уровня РНК ВИЧ-1 в диапазоне 20–10 млн. копий/мл.
- исследование абсолютного и относительного количества CD4-лимфоцитов осуществляли с использованием моноклональных антител фирмы Berhing в лимфоцитотоксическом тесте (NIH USA).
В процессе исследования клинических данных использовали систему STATISTICA for Windows (версия 10).
Результаты и обсуждение
Средний возраст женщин при введении «Импланон НКСТ» составил 36,2±0,7 (26–44) года. Большинство пациенток были социально-адаптированы, у 56% заражение ВИЧ произошло половым путем (табл. 3). Длительность инфицирования более 10 лет была у половины женщин (56%). Каждая вторая женщина была коинфицирована хроническим вирусным гепатитом С – 56,1%. Две пациентки являлись потребителями психоактивных веществ (4,9%). У подавляющего большинства женщин (88%) ВИЧ-инфекция находилась в продвинутой стадии (4А, 4Б, 4В), у 19,5% из них наблюдался иммунодефицит разной степени тяжести. Известно, что иммунодефицит является фактором риска перинатального заражения ВИЧ; причем степень иммунодефицита имеет обратную корреляционную зависимость с риском перинатальной передачи и частотой акушерских осложнений при беременности и в родах [26–28]. Пациентки данной группы начали АРТ незадолго до включения в исследование на фоне низкого количества CD4-лимфоцитов, поэтому применение эффективной пролонгированной контрацепции здесь является предпочтительным методом, как минимум до нормализации иммунного статуса, если пациентка заинтересована в беременности в будущем. Так как внутриматочные методы контрацепции не рекомендованы для начала использования у ВИЧ-инфицированных женщин, имеющих иммунный дефицит, остается возможность применения гормональных пролонгированных контрацептивов – имплантата с ЭТГ и инъекционного препарата с ДМПА [6, 7]. Четверть женщин на момент введения подкожного контрацептивного имплантата имели тромбоцитопению, почти половина – анемию, что может быть обусловлено хроническим ВИЧ-индуцированным воспалением костного мозга, приемом ряда антиретровирусных препаратов (зидовудин, фосфазид) или синдромом мальабсорбции, вызванным ВИЧ [29–31]. Так как анемии и тромбоцитопении у ВИЧ-инфицированных женщин связаны с увеличением частоты хронической плацентарной недостаточности, преждевременных родов, слабости родовой деятельности, высокой частотой кровотечений в родах и послеродовом периоде, материнской и младенческой смертностью, важно отложить наступление беременности до нормализации данных показателей с применением эффективной контрацепции [32–34]. Тяжелая тромбоцитопения или анемия может являться противопоказанием для прерывания нежеланной беременности или осложнить ее проведение. Таким образом, ВИЧ-инфицированные пациентки с тромбоцитопенией, анемией или их сочетанием также нуждаются в эффективной контрацепции.

Длительность и пути инфицирования ВИЧ, стадии заболевания и клинические характеристики пациенток представлены в таблице 3.
Все женщины, включенные в исследование, в течение последнего года жили регулярной половой жизнью. В зарегистрированном браке проживали половина женщин (n=21, 51%), табл. 3. Четверть пациенток (n=11, 26,8%) имели половые контакты с ВИЧ-инфицированным партнером, остальные проживали в серодискордантных по ВИЧ-инфекции парах или с партнером, ВИЧ-статус которого был неизвестен. При этом только четверть женщин (n=10, 24,4%) при половых контактах применяли барьерную контрацепцию (мужские презервативы), три пациентки ранее использовали внутриматочные медьсодержащие средства контрацепции (7,3%) и две – гормональные контрацептивы (инъекционный и комбинированный оральный). Следовательно, всего 37% женщин из группы исследования ранее применяли какие-либо контрацептивы, из них треть (12%) – высокоэффективные методы, что в более чем в два раза меньше по сравнению с женщинами, не инфицированными ВИЧ [6], и в 1,5–6 раз выше по сравнению с показателями у ВИЧ-инфицированных женщин в других исследованиях [20]. В исследовании, проведенном ранее в Санкт-Петербурге, было показано, что после качественного консультирования по планированию семьи 60% ВИЧ-инфицированных женщин выбрали высокоэффективные методы контрацепции (табл. 1) и в дальнейшем успешно их применяли [17, 21].
Таким образом, можно сделать вывод, что консультирование по выбору метода контрацепции является ключевым фактором использования эффективной контрацепции, в том числе у женщин с хроническими вирусными инфекциями. Имплантаты в группе исследования с целью контрацепции никто из женщин ранее не использовал. Основной причиной этого явился недостаток информации о гормональных методах планирования семьи (процедуры введения/удаления имплантата, возможные побочные эффекты), возможности их применения у женщин, живущих с ВИЧ (влияние на течение ВИЧ-инфекции, эффективность), и/или высокая стоимость контрацептива. Одной из причин, по которой женщины отдавали предпочтение имплантату, была информация о высокой контрацептивной эффективности метода, которая не зависит от строгого соблюдения женщиной ежедневного режима приема в отличие, например, от оральных гормональных средств. Женщины, живущие с ВИЧ, вынуждены пожизненно получать антиретровирусные препараты для лечения ВИЧ-инфекции, которые в большинстве случаев принимаются дважды в сутки в одно и то же время. В этом случае использование эффективного метода контрацепции, не требующего в течение трех лет никаких дополнительных действий, является очень важным преимуществом перед другими обратимыми методами планирования семьи. Высокая коморбидность у ВИЧ-инфицированных пациенток часто предполагает прием различных лекарственных средств помимо АРТ [25, 29, 32, 33], поэтому методы пролонгированной контрацепции должны стать методами выбора для женщин с ВИЧ и коинфекцией хронического гепатита С и В. Каждая вторая женщина, включенная в исследование, была коинфицирована хроническим гепатитом С (56%, табл. 3). В настоящее время для излечения хронического гепатита С используются препараты прямого противовирусного действия, на фоне приема которых не рекомендовано наступление беременности. Следовательно, в течение курса лечения этими препаратами для женщины крайне важна максимально эффективная защита от беременности, которую также могут обеспечить имплантаты.
В группе исследования отмечена высокая частота гинекологической патологии, которая в основном была представлена нарушениями менструального цикла в анамнезе (14,6%), эктопией шейки матки (9,8%), миомой матки (9,8%) и хроническими воспалительными заболеваниями органов малого таза (17,1%) (табл. 4). Известно, что нарушения менструального цикла по типу вторичной аменореи у женщин, живущих с ВИЧ, встречаются чаще, чем в популяции, что чаще связано не с самой ВИЧ-инфекцией, а с потреблением психоактивных веществ в анамнезе или в настоящее время, включая внутривенные наркотические средства [35]. В нашем исследовании 4,9% женщин были активными потребителями психоактивных веществ. Нередко у ВИЧ-инфицированных женщин, имеющих нарушения менструального цикла по типу вторичной аменореи и не использующих эффективную контрацепцию, незапланированная и, как правило, нежеланная беременность диагностируется во II или III триместрах беременности, когда ее прерывание возможно только по медицинским или социальным показаниям. При этом доля женщин, начавших профилактику перинатальной передачи ВИЧ в регламентированные сроки в этой группе, ниже, чем у пациенток с желанной и своевременно диагностированной беременностью, а частота отказов от детей выше. Согласно данным Центра СПИД, прекращение обеспечения ВИЧ-инфицированных женщин бесплатными, преимущественно гормональными контрацептивами (КОК, имплантаты, инъекционные контрацептивы) с 2021 г. явилось одной из причин увеличения числа отказов от новорожденных с 3–6 случаев в предыдущие годы до 25 в 2022 г. При этом наибольшее число отказов от детей в родильных домах отмечено у женщин – потребительниц психоактивных веществ. Данный факт подтверждает важность и необходимость решения вопроса обеспечения в первую очередь таких пациенток эффективными контрацептивами как компонента профилактики социального сиротства и снижения частоты перинатальной передачи ВИЧ. Каждая пятая пациентка имела хронические воспалительные заболевания органов малого таза, каждая десятая – эктопию шейки матки.
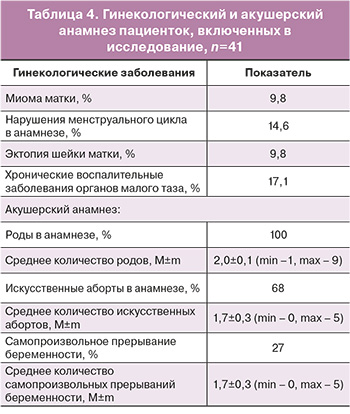
Все женщины, включенные в исследование, имели роды (табл. 4), две трети (68%) – искусственные аборты (2,0±0,1), у каждой третьей (27%) были самопроизвольные выкидыши (1,7±0,3), что подтверждает низкую частоту применения эффективной контрацепции в анамнезе.
Введение и удаление подкожного контрацептивного имплантата с ЭТГ прошло согласно стандартной процедуре без сложностей и осложнений у всех пациенток. Восемь из 10 женщин не имели побочных эффектов и не предъявляли жалоб на фоне использования данного метода контрацепции. Побочные эффекты на фоне использования имплантата с ЭТГ отмечались у 11 женщин (26,8%): увеличение массы тела (5–13 кг) у 5 пациенток (12,1%), дисменорея – у 4 (9,8%), в 2 случаях – депрессия (2,4%) и аллергическая реакция (2,4%), выражавшаяся в зуде кожных покровов. Важно отметить, что при введении имплантата с ЭТГ 35 пациенток (85%) уже получали АРТ, поэтому сложно связать увеличение массы тела только с применением имплантата с ЭТГ. Согласно данным клинических исследований, при применении нерентгеноконтрастного имплантата с ЭТГ частота дисменореи варьирует от 7,2 до 48%, увеличение массы тела встречается в 13,4% случаев, депрессия – у 5,5% [36, 37]. Согласно данным других авторов, на фоне применения имплантата с ЭТГ 77% участниц отмечали разрешение симптомов дисменореи и 6% – уменьшение их тяжести; дисменорея развилась или усугубилась у 5,5% женщин [37]. Таким образом, частота побочных эффектов на фоне использования имплантата с ЭТГ сопоставима с таковыми у женщин без ВИЧ-инфекции, за исключением дисменореи и депрессии, которые встречаются значительно реже. У 4 пациенток в связи с побочными эффектами, которые не купировались (длительные мажущие кровянистые выделения, прибавка массы тела 13 кг, аллергическая реакция и депрессия), имплантат с ЭТГ был удален до окончания срока его действия в течение первого года использования по согласованию с женщинами. Еще у 2 пациенток, которые хорошо переносили данный метод контрацепции, подкожный контрацептивный имплантат с ЭТГ был удален ранее предусмотренного срока в связи с отсутствием половой жизни по просьбе пациенток. В двух случаях причиной удаления имплантата с ЭТГ послужила беременность, наступившая на фоне его применения (третий год после введения). Установлено, что снижение контрацептивной эффективности метода связано с неучтенными межлекарственными взаимодействиями между ЭТГ и антиретровирусным препаратом из группы ННИОТ, который был назначен пациенткам после начала применения имплантата с ЭТГ. В обоих случаях беременность была диагностирована на раннем сроке: женщин беспокоил ранний токсикоз беременных, в связи с чем они обратились к гинекологу для консультации и проведения обследования. В обоих случаях имплантат с ЭТГ был извлечен сразу после диагностирования беременности, так как обе женщины выразили желание ее пролонгировать. Беременности протекали физиологически, родились доношенные дети без видимых пороков развития и других отклонений в состоянии здоровья.
В настоящее время 9 пациенток из группы исследования продолжают пользоваться данным методом контрацепции, у остальных женщин имплантат с ЭТГ извлечен в связи с истечением срока действия. Восемь женщин (25%) приняли решение о повторном введении имплантата с ЭТГ в день извлечения предыдущего.
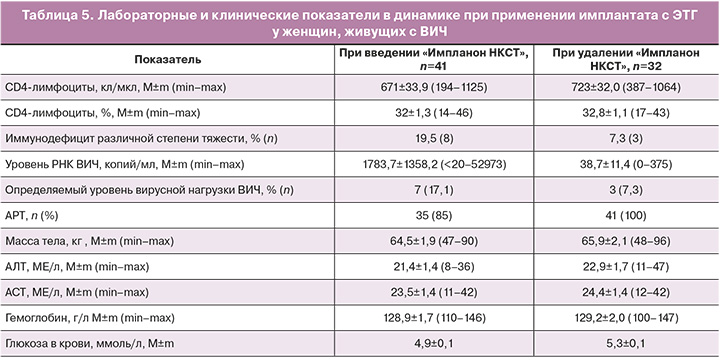
За время применения подкожного контрацептивного имплантата с ЭТГ у пациенток не отмечено значительных изменений количества CD4-лимфоцитов, уровня гемоглобина, АЛТ и АСТ, массы тела, что не противоречит данным других исследований [6, 7] (табл. 5). Отмечено уменьшение среднего уровня РНК ВИЧ в динамике, что можно связать с увеличением числа пациенток, получающих АРТ, с 85 до 100%. С применением АРТ можно связать снижение доли женщин с иммунодефицитом с 19,5 до 7,3% и числа пациенток с определяемой вирусной нагрузкой ВИЧ с 17,1 до 7,3%.
Заключение
ВИЧ-инфицированные женщины, включая пациенток с коинфекцией ВИЧ/хронический гепатит С, не имеют абсолютных противопоказаний для применения имплантата с ЭТГ. Имплантат с ЭТГ является методом выбора для пациенток, живущих с ВИЧ, и коинфекцией ВИЧ/хронический гепатит С, так как не влияет на прогрессирование ВИЧ-инфекции, высокоэффективен, не имеет значимых межлекарственных взаимодействий с большинством современных антиретровирусных препаратов. Высокая долгосрочная эффективность «Импланон НКСТ» при отсутствии необходимости в регулярном приеме важна для женщин, получающих лечение ВИЧ-инфекции, сопутствующих хронических заболеваний, потребляющих психоактивные вещества. Применение высокоэффективной контрацепции у женщин с хроническими вирусными инфекциями позволяет нормализовать иммунный статус и снизить вирусную нагрузку ВИЧ на фоне АРТ. Перед применением метода гормональной контрацепции или при старте АРТ/смене схемы АРТ у пациенток, живущих с ВИЧ, необходимо оценивать возможные межлекарственные взаимодействия. Важно интегрировать услуги по планированию семьи в оказание медицинской помощи женщинам с хроническими вирусными инфекциями с обеспечением их контрацептивами за счет региональных программ по профилактике ВИЧ-инфекции. Данная мера оправдана экономически и позволяет использовать безопасные и эффективные методы контрацепции женщинам с ограниченными финансовыми ресурсами.