В последние десятилетия частота многоплодных беременностей непрерывно растет в связи с широким внедрением вспомогательных репродуктивных технологий (ВРТ), поздним репродуктивным возрастом первородящих, наступлением беременности после отмены оральных контрацептивов [1]. Многоплодная беременность ассоциирована с высоким риском развития осложнений как со стороны матери, так и со стороны плодов. Замедление роста одного или обоих плодов при двойне является одной из главных причин перинатальных потерь [2]. Частота встречаемости данного патологического состояния при монохориальной двойне составляет 15–25%, при дихориальной – 5–10% [3].
Изучить особенности роста плодов при многоплодной беременности можно двумя способами: оценить соответствие веса каждого плода нормативным значениям и определить разницу, или дискордантность, их предполагаемой массы. Важно отметить, что, даже если вес близнецов соответствует норме, но имеет место разница в весе между ними, риск неблагоприятных исходов повышается [2].
Обычно дискордантность в весе плодов при отсутствии других патологических состояний позволяет предположить, что у одного из них имеется замедление роста. Согласно рекомендациям Национального института здоровья и медицинской помощи Соединенного Королевства, разница в весе плодов из двойни более 25% является важным клиническим признаком замедления роста плода [4]. Аналогично, Американским колледжем акушеров и гинекологов для диагностики значимого дискордантного роста близнецов принята разница в предполагаемой массе 25% [5]. Разница в весе плодов рассчитывается по следующей формуле: ((А – В)×100)/А, где А – вес большего плода; В – меньшего.
Известно несколько факторов, приводящих к дискордантности роста плодов при многоплодной беременности. Эти факторы, в зависимости от этиологии, можно разделить на три группы – материнские, плодовые и плацентарные [6]. К материнским факторам обычно относят возраст беременной, антропометрические характеристики, паритет, использование вспомогательных репродуктивных технологий, соматическую и гинекологическую патологию. Плодовые факторы риска развития дискордантного роста включают монохориальный тип плацентации, внутриутробное инфицирование цитомегаловирусом, генетическую аномалию одного из плодов. К плацентарным факторам можно отнести предлежание, отслойку плаценты, аномальное (оболочечное или краевое) отхождение пуповины, неравномерное разделение плацентарной территории при монохориальной двойне, тип, размер и количество сосудистых анастомозов монохориальной плаценты.
Крайне важно установить связь между дискордантным ростом плодов и перинатальными осложнениями, так как это влияет на тактику ведения беременности. При этом определение влияния дискордантного роста плодов на перинатальные исходы представляет определенные сложности [7]. В большинстве опубликованных по данной теме работ встречаются такие ограничения, как исследование небольшой выборки, отсутствие точного датирования срока беременности, наличие акушерских и соматических осложнений, хромосомных аномалий и пороков развития плодов, отсутствие данных о показаниях к родоразрешению и его методе, о госпитализации в отделение реанимации и интенсивной терапии новорожденных (ОРИТН) [8, 9].
Наличие этих ограничений не позволяет сделать вывод об истинном влиянии дискордантности на перинатальные исходы.
В связи с вышесказанным, целью данного исследования явилась оценка перинатальных исходов при дискордантности веса новорожденных из двойни более 25%.
Материалы и методы
Проведено ретроспективное исследование 485 беременных и их 959 новорожденных, которые находились под наблюдением и были родоразрешены на базе ФГБУ «НМИЦ АГП им. В.И. Кулакова» Минздрава России в 2014–2019 гг.
Критерии включения: беременность двойней вне зависимости от типа хориальности.
Критерии исключения: многоплодная беременность высшего порядка (тройни, четверни), хромосомные аномалии у одного или обоих плодов, фето-фетальный трансфузионный синдром и синдром обратной артериальной перфузии при монохориальной двойне.
Срок беременности рассчитывался на основании первого дня последней менструации или копчико-теменного размера большего плода, измеренного в 10–14 недель беременности.
Для расчета дискордантности веса новорожденных применялась следующая формула: ((А–В)×100)/А, где А – вес большего плода; В – меньшего. Критерием значимой дискордантности считалась разница в весе более 25%. На основании этого были сформированы: группа новорожденных с дискордантностью (разница 25% и более) и группа с симметричным весом (разница менее 25%).
Характеристика групп беременных включала возраст, индекс массы тела, паритет, тип наступления беременности. Оценка антенатального течения беременности проводилась на основании данных о внутриутробной гибели плода, методе родоразрешения (кесарево сечение, естественные роды), показаниях к родоразрешению (плодовые, материнские), а также наличии гестационного диабета и преэклампсии.
Оценка неонатальных исходов включала: гестационный возраст и массу тела новорожденных, оценку по шкале Апгар к концу 1-й и 5-й минут жизни, потребность в проведении лечения и выхаживания в условиях ОРИТН, продолжительность пребывания в ОРИТН, частоту развития внутрижелудочковых кровоизлияний как внутриутробно, так и в неонатальном периоде, развитие бронхолегочной дисплазии и ретинопатии недоношенных. Неонатальная смертность регистрировалась до момента выписки из стационара. Долгосрочные исходы у выписанных из стационара пациентов в ходе данного исследования не оценивались.
Статистический анализ
Для статистической обработки данных и построения графиков использовали электронные таблицы Microsoft Excel и пакет программ GraphPad Prism 8 (GraphPad Software, USA). Для определения нормальности распределения использовали обобщенный тест Д᾽Агостино–Пирсона. Данные с нормальным распределением представлены как среднее значение (стандартное отклонение), для их сравнения использовали t-test. Данные с распределением, отличным от нормального, представлены как медиана (интерквартильный размах), для их сравнения использовали критерий Манна–Уитни. Качественные данные представлены как абсолютное значение (n) и %, для их сравнения использовали точный тест Фишера. Различия считали статистически значимыми при p<0,05. Исследование было одобрено комиссией по этике ФГБУ «НМИЦ АГП им. В.И. Кулакова» Минздрава России.
Результаты
В ходе исследования установлено, что выраженная, более 25%, дискордантность веса новорожденных была у 18,8% (n=91) двоен, у 81,2% (n=394) пациенток на протяжении беременности отмечался симметричный рост плодов.
В исследуемых группах статистически различался возраст беременных – дискордантность веса новорожденных встречалась чаще у беременных более молодого возраста – 32,9 года, в то время как при симметричном весе возраст беременных составлял 34,3 года, р=0,02.
Значимые различия исследуемых групп по таким характеристикам, как индекс массы тела (ИМТ) беременных, паритет, тип наступления беременности, а также осложнения беременности (гестационный диабет и преэклампсия) выявлены не были.
Частота антенатальной смертности в исследуемой когорте составила 2,3% (n=11). Сравнение данного показателя в группах показало значительное его увеличение при наличии дискордантности – 6,6% (n=6); при симметричном весе внутриутробная гибель встречалась в 1,3% случаев (n=5), р=0,008, отношение шансов 5,5 (95% доверительный интервал (ДИ) 1,6–16,1).
Самым распространенным способом родоразрешения в изучаемой когорте было кесарево сечение. При этом его частота в группе с дискордантным весом была выше, чем с симметричным – 95,6% и 83,2% соответственно, р=0,002.
Также в исследуемых группах были выявлены статистически значимые различия показаний к родоразрешению. Беременные с дискордантным весом новорожденных значительно чаще родоразрешались по показаниям со стороны плодов – в 53,8%, при симметричном – только в 11,7% случаев, р<0,001. У пациенток из группы с симметричным весом новорожденных первое место среди показаний к родоразрешению занимали материнские – 36,3%, в то время как при дискордантном – в 20,9%, р<0,001.
Большинство беременных – 362 (74,6%) пациентки были родоразрешены преждевременно, до 37 недель. Сравнение частоты преждевременных родов в исследуемых группах показало значимое различие – 94,5% (n=86) при дискордантном весе и 70,1% (n=276) – при симметричном, р<0,001.
Клинические характеристики беременных и антенатального периода исследуемых групп представлены в таблице 1.
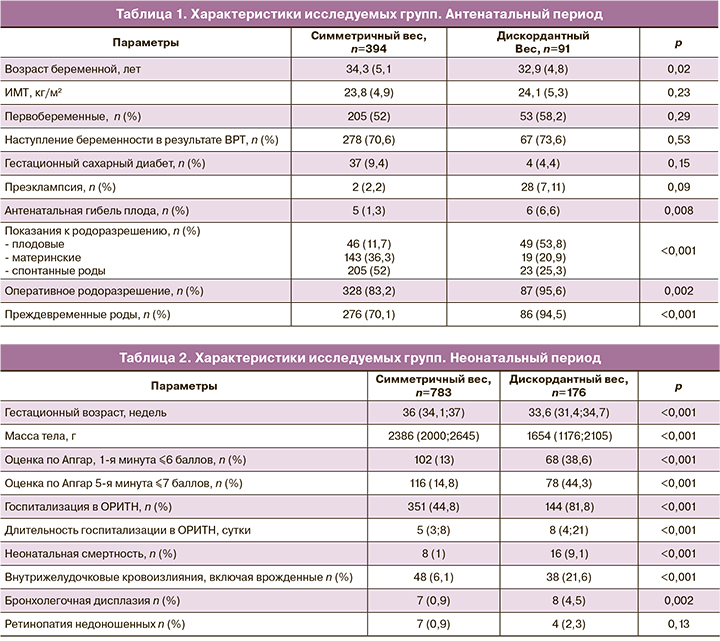
Гестационный возраст новорожденных отличался в исследуемых группах – медиана в группе с дискордантным весом составила 33,6 недель, в то время как при симметричном – 36 недель, р<0,001.
Анализ массы тела новорожденных показал значительно меньшие медианные значения при наличии дискордантности по сравнению с группой с симметричным весом – 1654 и 2386 г соответственно, р<0,001.
Оценка состояния новорожденных проводилась на основании шкалы Апгар. В каждой из групп рассчитывалось количество детей, у которых к концу первой минуты жизни оценка составляла 6 баллов и менее, к концу пятой минуты – 7 баллов и менее. В группе с дискордантным весом количество детей с низкой оценкой по шкале Апгар было значительно больше, чем с симметричным – на 1-й минуте 38,6% и 13%, на 5-й – 44,3% и 14,8% соответственно (р<0,001).
Анализ ранней неонатальной смертности выявил значительное увеличение этого показателя в группе с дискордантным весом новорожденных. Так, при симметричном весе неонатальная смертность составила 1% (8 детей), а при дискордантном – 9,1% (16 детей), р<0,001, отношение шансов 9,7 (95% ДИ 4,3–21,7). При этом обращает на себя внимание отсутствие статистической значимости в частоте данного показателя между новорожденными с отставанием веса и с нормальным весом – 1,2% (11 из 959) и 0,5% (5 из 959) соответственно, р=0,21. Дополнительно хочется отметить, что все случаи неонатальной смертности отмечались только среди детей, родоразрешенных оперативно.
Сравнение частоты осложнений неонатального периода показало их преобладание в группе с дискордантным весом. Так, частота госпитализаций в ОРИТН при дискордантном весе составляла 81,8% (n=144), при симметричном – 44,8% (n=351), р<0,001. Длительность пребывания в ОРИТН также была больше при дискордантном весе – 8 дней против 5, р<0,001. В ходе анализа неонатальной заболеваемости установлено повышение частоты внутрижелудочковых кровоизлияний, включая врожденные, и развитие бронхолегочной дисплазии у новорожденных с дискордантным весом по сравнению с детьми, вес которых был симметричным – 21,6% против 4,5% (р<0,001) и 6,1% против 0,9% (р=0,002).
Клинические характеристики новорожденных и неонатального периода исследуемых групп представлены в таблице 2.
Обсуждение
Замедление роста одного или обоих плодов при многоплодной беременности является одной из главных причин перинатальной заболеваемости и смертности [2]. Диагностика данного патологического состояния возможна с помощью оценки соответствия веса каждого плода нормативным значениям или определения разницы или дискордантности их предполагаемой массы. Важно отметить, что, даже если вес близнецов соответствует норме, но имеет место разница в весе между ними, риск неблагоприятных исходов повышается [2]. Обычно дискордантность в весе плодов при отсутствии других патологических состояний позволяет предположить, что у одного из них имеется замедление роста. Согласно рекомендациям Национального института здоровья и медицинской помощи Соединенного Королевства и Американского колледжа акушеров и гинекологов, наличие разницы между предполагаемыми массами плодов более 25% является признаком замедления роста [4, 5]. В то же время существует дискуссия относительно определения значимой дискордантности веса новорожденных, влияющей на перинатальные исходы. В данном исследовании использовался уровень отсечки в 25%. Miller et al. установили, что разница в весе на 20% может быть обнаружена приблизительно у 16% двоен [10]. В недавнем систематическом обзоре и метаанализе, посвященном перинатальной летальности при беременности двойней, установлено, что границей отсечки дискордантности веса, влияющей на данный показатель для дихориальной двойни, является 15%, а для монохориальной – 25% [9]. Частота новорожденных с дискордантностью веса более 25% в настоящем исследовании составила 18,8%, что сопоставимо с приведенными выше данными.
В нашем исследовании оценка антенатального периода не выявила статистически значимого различия между группами по частоте таких акушерских осложнений, как гестационный диабет и преэклампсия. По данным Machado et al., проанализировавших течение 1051 беременности двойней, влияния типа хориальности и дискордантного роста плодов на развитие преэклампсии также выявлено не было [11].
Частота антенатальной смертности в данном исследовании составила 2,3%. В ходе анализа данного показателя в группах было подтверждено предположение влияния на него дискордантного роста – риск антенатальной гибели повышен в 5,5 раза (ОШ 5,492; 95% ДИ 1,571–16,11) по сравнению с группой с симметричным весом.
В большом проспективном исследовании, которое включало 3005 беременностей двойней, частота антенатальной гибели плодов варьировала от 6,5 до 19,1 на 1000 плодов, что в целом сопоставимо с полученными нами данными [12].
Большинство (95,6%) беременных с дискордантным весом новорожденных были родоразрешены оперативно, путем операции кесарева сечения. Схожий процент оперативного родоразрешения двойни был продемонстрирован Carter et al. – частота кесарева сечения превышала 94% [13]. Аналогичные данные были получены в исследованиях Al Riyami и Fumagalli - процент кесаревых сечений составил 94% и 97% соответственно [14, 15].
Интересные данные представили Lee et al., которые показали зависимость частоты кесарева сечения при двойне от гестационного возраста [16]. В их исследовании 98% беременностей на 35-й неделе заканчивались кесаревым сечением, но процент постепенно уменьшался с увеличением срока, и на 38-й неделе только 52% родов были оперативными. Также высокую частоту операции кесарева сечения при дискордантности веса можно объяснить необходимостью экстренного родоразрешения при ухудшении состояния плода с замедлением роста.
Определение оптимального срока родоразрешения при многоплодной беременности является непростой задачей, решение которой зависит от многих факторов. В данном исследовании 74,6% беременностей закончились преждевременно, до 37 недель беременности. В ряде опубликованных исследований частота преждевременных родов при двойне варьирует от 54,4% до 87% [17, 18]. Беременные с выраженной дискордантностью веса плодов, как правило, родоразрешаются преждевременно из-за риска внутриутробной гибели плода с отставанием, что было подтверждено в ходе данного исследования. Средний гестационный возраст новорожденных с дискордантным весом составил 33,6 недели, частота преждевременных родов – 94,5%. Это также сопровождалось превалированием показаний к родоразрешению со стороны плодов в данной группе. При этом известно, что гестационный возраст при рождении является основной детерминантой перинатального исхода как при одноплодной, так и многоплодной беременности [19, 20]. Вполне возможно, что наблюдаемая более высокая частота ранней неонатальной заболеваемости и смертности у новорожденных с дискордантностью может быть результатом ятрогенных преждевременных родов, предпринятых для снижения частоты антенатальной смертности, а не следствием несоответствия веса. Однако, по данным Di Mascio et al., которые проанализировали исходы детей из двойни, рожденных после 34 недели, повышенный риск неонатальной заболеваемости был характерен для новорожденных с дискордантным весом [21]. Это позволило авторам предположить, что дискордантность веса новорожденных является независимым фактором, негативно влияющим на перинатальный исход, даже в более позднем гестационном возрасте.
Сравнение неонатальных исходов, представленных в нашем исследовании, показало влияние дискордантности веса новорожденных на частоту заболеваемости и смертности. Кроме того, масса тела новорожденных с дискордантностью была закономерно меньше, чем у детей с симметричным ростом. На этот факт могло повлиять не только замедление роста одного из плодов, но и более раннее родоразрешение в этой группе.
Оценка состояния новорожденных проводилась на основании шкалы Апгар на 1-й и 5-й минутах. В группе с дискордантным весом количество детей с оценкой по шкале Апгар 6 баллов и менее на 1-й минуте составило 38,6% и 7 баллов и менее на 5-й – 44,3%, что значительно превосходило частоту низких оценок при симметричном весе новорожденных. Timur et al. также обнаружили, что неблагоприятные перинатальные исходы, в том числе очень низкая масса тела при рождении и низкие баллы по шкале Апгар, чаще встречались у новорожденных из двойни, чем при одноплодной беременности [22].
Новорожденные с дискордантным весом значительно чаще госпитализировались в ОРИТН, что также сопровождалось более длительным пребыванием в стационаре по сравнению с группой детей с симметричным весом. Закономерно, что неонатальная заболеваемость у новорожденных с дискордантностью веса была выше. Так, частота внутрижелудочковых кровоизлияний, включая врожденные, при наличии дискордантности повышалась в 3,6 раза, что подтверждается опубликованными работами. Hack et al. выявили более высокую частоту неврологической патологии у новорожденных с дискордантным весом [3]. По данным D’Antonio et al., риск неврологической патологии увеличивался с увеличением процента дискордантности [9].
В ходе данного исследования установлено, что частота ранней неонатальной смертности была в 9,7 раза выше при наличии дискордантного веса новорожденных (ОШ 9,688; 95% ДИ 4,298–21,71). При этом статистически значимая разница неонатальной смертности между меньшим и большим новорожденными в дискордантной паре выявлена не была. Возможно, отсутствие данной взаимосвязи может быть объяснено большим влиянием недоношенности.
Результаты нашего исследования показали, что дискордантный вес связан как с антенатальной летальностью, так и с неонатальной заболеваемостью и смертностью. В связи с чем многоплодная беременность с дискордантным ростом плодов должна рассматриваться как беременность высокого риска. Несмотря на представленные результаты, несоответствие в весе само по себе не должно использоваться в качестве основного показания для досрочного родоразрешения с целью снижения антенатальной смертности, так как ятрогенные преждевременные роды могут увеличивать риск неблагоприятных исходов.
Основными ограничениями данного исследования являются ретроспективный и нерандомизированный дизайн, количественные различия между группами, а также отсутствие стратификации исходов в зависимости от типа хориальности. Известно, что причины дискордантного роста плодов при дихориальной и монохориальной беременностях различны, а наличие специфических осложнений монохориальной беременности может значительно влиять на перинатальные исходы. Несмотря на отсутствие стратификации групп по типу хориальности, в настоящем исследовании для устранения потенциальных факторов, влияющих на перинатальные исходы, были исключены случаи фето-фетального трансфузионного синдрома, синдрома обратной артериальной перфузии, хромосомные нарушения и врожденные пороки развития плодов. Сильной стороной исследования является достаточная выборка из 485 беременных женщин и их 959 новорожденных, а также обработка данных, полученных в одном учреждении.
Данное исследование позволило оценить влияние дискордантности веса новорожденных из двойни на перинатальные исходы. Однако требуются дальнейшие исследования влияния недоношенности и типа хориальности на частоту неблагоприятных исходов у новорожденных с дискордантным весом. Необходимо проведение проспективного рандомизированного исследования, чтобы доказать истинное влияние дискордантного роста плодов на перинатальные исходы.
Заключение
Дискордантный рост плодов из двойни является фактором риска преждевременных родов и оперативного родоразрешения. Дискордантность оказывает влияние как на частоту антенатальной летальности, так и неонатальной заболеваемости и смертности. При этом возможно, что ряд осложнений неонатального периода у новорожденных с дискордантным весом можно связать с влиянием недоношенности.