Assessment of quality of life, psycho-emotional state, eating behavior, obstetric and perinatal outcomes in pregnant women with early and late gestational diabetes mellitus
Objective: To evaluate anamnestic data, quality of life, psycho-emotional state, eating behavior, obstetric and perinatal outcomes in women with early and late gestational diabetes mellitus (GDM). Materials and methods: We conducted a study that included 144 women with GDM. 86 out of these women were included in group 1 with early GDM that was detected before 24 weeks of pregnancy, and group 2 comprised 68 women with late GDM detected after 24 weeks. The questionnaires Short Form 36 (SF-36), Well-being-Activity-Mood (WAM), Hospital Anxiety and Depression Scale (HADS) and the Dutch eating behavior questionnaire (DEBQ) were used. The course of pregnancy and perinatal outcomes were evaluated. Results: Women with GDM that was detected in early pregnancy were characterized by decreased indicators of vital activity, social functioning, mental and psychological health, well-being and mood, high indicators of subclinical anxiety and subclinical depression. Women with GDM that was detected in early pregnancy were characterized by frequent mental distress (RR 3.36; 95% CI 1.67–6.78; p<0.001), miscarriages inherited from their mothers (RR 9.49; 95% CI 1.26–71.18; p=0.03), arterial hypertension during previous pregnancy (RR 5.14; 95% CI 1.20–22.01; p=0.03), recurrent miscarriage in medical history (RR 8.69; 95% CI 1.15–65.72; p=0.04), intake of methylprednisolone (RR 9.49; 95% CI 1.26–71.18; p=0.03), tranexamic acid (RR 9.49; 95% CI 2.32–38.75; p=0.002), sodium ethamsylate (RR 5.53; 95% 1.30–23.53; p=0.02), threatened early miscarriage (RR 13.84; 95% CI 3.45–55.50; p<0.001), threatened late miscarriage (RR 4.47; 95% CI 1.02–15.70; p=0.04), placental insufficiency (RR 4.47; 95% CI 1.61–12.44; p=0.004), premature birth (RR 3.89; 95% CI 1.37–11.03; p=0.01). The patients with GDM that was detected in later terms of pregnancy were characterized by more frequent presence of type 1 diabetes mellitus in first-degree relatives (RR 0.05; 95% CI 0.003–0.79; p=0.03), and in second-degree relatives (RR 0.13; 95% CI 0.03–0.56; p=0.01), late menarche (12.6 (1.3) and 13.4 (1.3); p=0.01), frequent dysmenorrhea (RR 0.47; 95% CI 0.36–0.62; p<0.001). Conclusion: Women with early GDM were characterized by frequent mental distress, miscarriages inherited from their mothers, arterial hypertension during previous pregnancy, recurrent miscarriage in medical history, intake of methylprednisolone, tranexamic acid and ethamsylate, threatened early and late miscarriages, placental insufficiency, premature birth. Women with late GDM were characterized by the frequent presence of type 1 diabetes mellitus in first-degree and second-degree relatives, late menarche, dysmenorrhea in anamnesis. Authors’ contributions: Batrak N.V., Malyshkina A.I., Tkachenko A.S. – material collection, design of the study, review of publications on the topic of the article, statistical analysis of the obtained data, writing the text of the manuscript. Conflicts of interest: The authors declare that they have no conflicts of interest. Funding: The study was conducted without any sponsorship. Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Ivanovo Research Institute of Maternity and Childhood named after V.N. Gorodkov, Ministry of Health of Russia. Patient Consent for Publication: All patients provided informed consent for the publication of their data. Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator. For citation: Batrak N.V., Malyshkina A.I., Tkachenko A.S. Assessment of quality of life, psycho-emotional state, eating behavior, obstetric and perinatal outcomes in pregnant women with early and late gestational diabetes mellitus. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (2): 64-70 (in Russian) https://dx.doi.org/10.18565/aig.2022.230Batrak N.V., Malyshkina A.I., Tkachenko A.S.
Keywords
Gestational diabetes mellitus (GDM) is the most frequent metabolic disorder in pregnant women. The prevalence of GDM throughout the world is steadily increasing and varies from 1 to 14%, and reaches 7% on average in the total population of different countries [1, 2]. One in seven infants is born to a mother with a certain type of hyperglycemia during pregnancy. In addition, 84% of cases of first diagnosed diabetes during pregnancy are associated with GDM [3].
GDM is a serious medical and social problem due to increasing frequency of complications and adverse pregnancy outcomes, and their rate depends on the gestational age, when the disease is diagnosed [4–6]. Moreover, in women affected by GDM, the risk of developing type 2 diabetes mellitus in the subsequent 10–20 years increases by 3–6 times [7].
The increasing prevalence of GDM and complications associated with GDM leads to the necessity of identifying risk factors for the development of this disease [8]. The best-studied risk factors of GDM are maternal age, family history of diabetes mellitus, previous history of fetal macrosomia, ethnicity, overweight or obesity, cigarette smoking, genetic factors, harmful effects of environmental pollution [9, 10].
In addition to these risk factors, the data accumulated in epidemiological studies show that dietary and lifestyle factors, psychosocial status both before and during pregnancy are associated with the risk of developing GDM [9, 11].
Throughout many years it has been discovered that a number of dietary factors before pregnancy are significantly associated with the risk of developing GDM. Among them, potentially harmful factors include sugar-sweetened beverages, consumption of heme iron, fried foods, animal fats and animal proteins, a low-carbohydrate diet, as well as high consumption of red meat and prefabricated meat, refined grains, sweets, fried potatoes and pizza [9, 12]. It has been discovered that the Mediterranean Diet (MedDiet), Dietary Approaches to Stop Hypertension (DASH) and the Alternative Healthy Eating Index (AHEI) were associated with reduction of relative risk of GDM by 15–38% [12].
Research on physical activity using International Physical Activity Questionnaire (IPAQ) showed that lack of physical activity before and during pregnancy was associated with increased risk for developing GDM in later terms of pregnancy [13]. Physical activity before pregnancy or in early terms was associated with reduction of occurrence of GDM by 30% and 21%, respectively. In addition, any form of physical activity for more than 90 minutes per week before pregnancy was associated with reduction of probability of GDM by 46% [13].
Due to this, timely and adequate detection, correction of modifiable risk factors for maternal hyperglycemia, eating behavior and psycho-emotional state will improve the women’s and children’s quality of life [14–21].
The objective of this study was to evaluate anamnestic data, quality of life, psycho-emotional state, eating behavior in women with early and late GDM, as well as to study the impact of early and late GDM on obstetric and perinatal outcomes.
Material and methods
A prospective study was carried out. It included pregnant women with GDM that was diagnosed according to the Russian national consensus Gestational diabetes mellitus: the diagnosis, treatment and postpartum follow-up” (No. 15-4/10/2-9478, 2013). All women have signed informed consent for participation in the study and examination of their newborns. Exclusion criteria were type 1 and type 2 diabetes mellitus that was diagnosed before and during pregnancy, multiple pregnancy. The clinical examination of patients was performed in women’s clinics in Ivanovo. The study included 144 pregnant women, who were divided into 2 groups depending on the gestational age, when GDM was detected. Group 1 included 86 pregnant women with GDM that was diagnosed before 24 weeks of pregnancy (early GDM). Group 2 comprised 68 women with GDM that was diagnosed at 24 weeks of pregnancy and later (late GDM).
The Short Form 36 (SF-36) questionnaire was used to assess quality of life. Psycho-emotional state of women was assessed using the Well-being-Activity-Mood (WAM) questionnaire. Anxiety and depression was assessed using Hospital Anxiety and Depression Scale (HADS). Eating behavior was assessed using the Dutch Eating Behavior Questionnaire (DEBQ). Assessment of occupational factors, heredity, obstetric, gynecologic and somatic anamnesis and infections in medical history, the course of the current pregnancy and perinatal outcomes was performed by collection of anamnestic data, the studies of outpatient cards and birth histories.
Statistical analysis
The Shapiro–Wilk test was used to check normality of distribution and Levene’s test was used to check equality of variances. Quantitative description of the values with a normal distribution was performed by calculating the arithmetic mean (M) and standard deviation (SD). The parametric Student's t-test was used for definition of statistical significance of differences. The values characterizing qualitative parameters were displayed as absolute numbers, and relative values were displayed as percentage. Pearson's chi-square test (χ²) was used to assess the significance of qualitative variables between the groups. Relative risk (RR) was calculated with 95% confidence interval (95% CI). For statistical hypothesis testing, the critical level of significance was considered at p=0.05. Statistical data processing was performed using Statistica for Windows 10.0, MedCalc.
Results
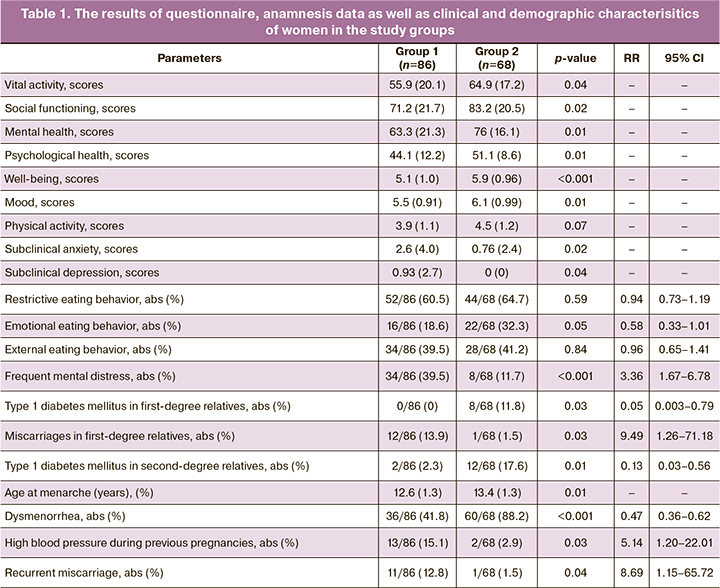
According to the Short Form 36 (SF-36) questionnaire, it was found that women with early GSD had low scores of vital activity (55.9 (20.1) and 64.9 (17.2) scores; р=0.04), social functioning (71.2 (21.7) and 83.2 (20.5)scores; р=0.02), mental health (63.3 (21.3) and 76 (16.1) scores; р=0.01) and psychological health (44.1 (12.2) and 51.1 (8.6) scores; р=0.01)
The results of the Well-being-Activity-Mood (WAM) questionnaire were also less satisfactory for well-being (5.1 (1.0) and 5.9 (0.96) scores; р<0.001) and mood (5.5 (0.91) and 6.1 (0.99) scores; р=0.01) in pregnant women with GDM that was diagnosed before 24 weeks than in women with late GDM.
Hospital Anxiety and Depression Scale (HADS) indicated that subclinical anxiety was statistically significant (2.6 (4.0) and 0.76 (2.4) scores; р=0.02) and prevailed in pregnant women with early GDM. Subclinical depression (0.93 (2.7) and 0 (0) scores; р=0.04) also prevailed in pregnant women with early GDM.
The results of the Dutch Eating Behavior Questionnaire did not find statistically significant difference in eating behavior between the women in the groups under study.
Women with GDM that was detected in early pregnancy were characterized by frequent mental distress (RR 3.36; 95% CI 1.67–6.78; p<0.001), miscarriages inherited from their mothers (RR 9.49; 95% CI 1.26–71.18; p=0.03), arterial hypertension during previous pregnancy (RR 5.14; 95% CI 1.20–22.01; p=0.03), recurrent miscarriage in medical history (RR 8.69; 95% CI 1.15–65.72; p=0.04.)
The patients with late GDM were characterized by more frequent presence of type 1 diabetes mellitus in first-degree relatives (RR 0.05; 95% CI 0.003–0.79; p=0.03), and hereditary type 1 diabetes mellitus in second-degree relatives (RR 0. type 1 diabetes mellitus in first-degree relatives 13; 95% CI 0.03–0.56; p=0.01), late menarche (12.6 (1.3) and 13.4 (1.3); p=0.01), frequent dysmenorrhea (RR 0.47; 95% CI 0.36–0.62; p<0.001).
The obtained results are shown in Table 1.
Medications used to treat endocrine, obstetric and gynecological disorders during the current pregnancy played an important role in the development of GDM. We found an association between early GDM and intake of methylprednisolone (RR 9.49; 95% CI 1.26–71.18; р=0.03), tranexamic acid (RR 9.49; 95% CI 2.32–38.75; р=0.002), sodium ethamsylate (RR 5.53; 95% 1.30–23.53; р=0.02). The obtained results are shown in Table 2.
Analysis of the course of the current pregnancy showed that most often the women with early GDM had early threatened miscarriages (RR 13.84; 95% CI 3.45–55.50; р<0.001), late threatened miscarriages (RR 4.47; 95% CI 1.02–15.70; р=0.04) placental insufficiency (RR 4.47; 95% CI 1.61–12.44; р=0.004), premature birth (RR 3.89; 95% CI 1.37–11.03; р=0.01).
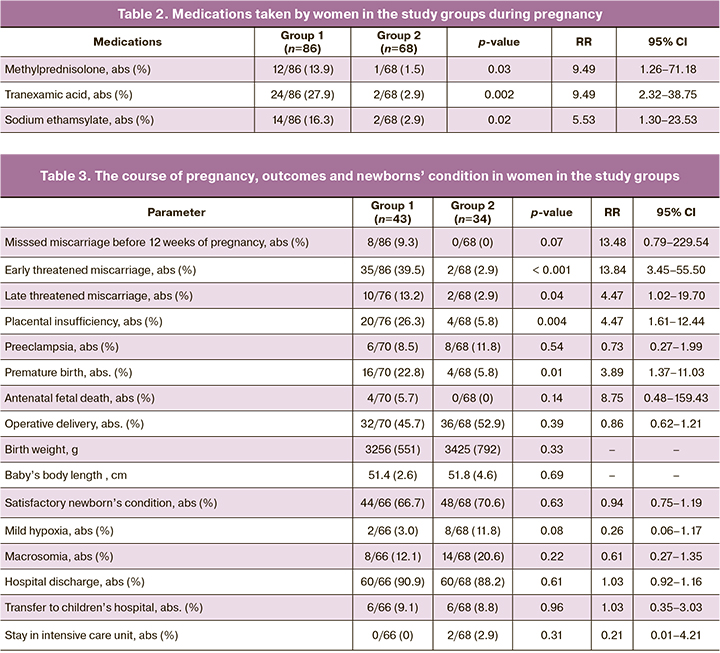
Analysis of the anthropometric data showed high birth weight (3256 (551) and 3425 (792) g; р=0.33) and infant’s body length (51.4 (2.6) and 51.8 (4.6) cm; р=0.69) born to women in group 2. However, these values were statistically non-significant.
The newborns of women in both groups equally needed treatment and transferring to other departments or hospitals. The obtained results are shown in Table 3.
Women in both groups equally rarely consulted endocrinologist after the completion of pregnancy (11/86 (12.8%) and 14/68 (20.6%); р=0.19). Due to this, the diagnosis of GSD was cancelled in a small number of women who sought help from the doctor (11/86 (12.8%) and 14/68 (20.6%); р=0.19).
Discussion
Taking into account the obtained results, to prevent the development of GDM in the preconception period and during pregnancy, it is necessary to correct the detected impairments: optimization of working conditions; psychologist’s consultation; balanced diet; timely prevention and treatment of complications that develop during pregnancy; prescription of drugs strictly according to indications; to raise awareness of doctors and women about the need for postpartum care after GDM, including prophylactic medical examination and regular invitation of women to see a doctor to reconsider the diagnosis.
In this regard, improvement in quality of life, physical and psychological health can be achieved by various intervention programs for behavior changes in management of diabetes. We recommend that implementation of integration programs, including telemedicine and educational courses that can improve quality of life in patients with GDM and provide support for healthy lifestyle in these category of women, serve as a ground for successful treatment of the disease.
Therefore, a rational solution of this issue is organization of schools for women with GDM for the purpose to improve quality of life, provide psycho-emotional support, correct eating behavior, help to control the disease. All these will contribute to reduction in the frequency of complications and adverse obstetric and perinatal outcomes in pregnant women, saving healthcare resources associated with negative impact of GDM.
It is advisable that training for women with GDM should be organized in women’s clinics according to the developed and structured program, including general information about the disease; eating behavior; physical activity; psychosocial support; quality of life; self-control of glycemia; insulin therapy; postpartum care; preconception preparation for the subsequent pregnancy.
Since GDM is an interdisciplinary issue, it is necessary to involve obstetricians and gynecologists, endocrinologists, nutritionists, psychologists, physiotherapists in the activity of these schools.
Organization of “Schools for pregnant women with GDM” will make it possible to eliminate the lack of knowledge of patients about the existing disease, to control their health, will contribute to the achievement of metabolic compensation, that will lead to reduction of pregnancy complications and improve pregnancy outcomes. Raising patient awareness as a result of training, will create the preconditions for their more active participation in treatment process, and implementation of training programs with involvement of obstetricians and gynecologists and related professionals will optimize the work of the Obstetric and Gynecological Service.
Conclusion
It was found that women with early GDM were characterized by decrease in the scores of vital activity, social functioning, mental and psychological health, well-being and mood, high scores of subclinical anxiety and subclinical depression, frequent mental distress, miscarriages inherited from their mothers, arterial hypertension during previous pregnancy, recurrent miscarriage in medical history, intake of methylprednisolone, tranexamic acid, ethamsylate during the current pregnancy, threatened early and late miscarriages, placental insufficiency, premature birth. Women with late GDM were characterized by the frequent presence of type 1 diabetes mellitus in first-degree and second-degree relatives, late menarche, dysmenorrhea in anamnesis. Timely correction of impairments defines obstetric and perinatal outcomes.
References
- Мирошник Е.В., Рюмина И.И., Зубков В.В. Влияние сахарного диабета матери на здоровье новорожденного. Акушерство и гинекология. 2016; 9: 45-9. [Miroshnik E.V., Ryumina I.I., Zubkov V.V. Impact of maternal diabetes mellitus on neonatal health. Obstetrics and Gynecology. 2016; (9): 45-9.(in Russian)]. https://dx.doi.org/10.18565/aig.2016.9.45-9.
- Радзинский В.Е., Папышева О.В., Есипова Л.Н., Старцева Н.М., Котайш Г.А. Особенности медицинской помощи при гестационном сахарном диабете (на примере специализированного акушерского стационара). Акушерство и гинекология. 2018; 2: 108-14. [Radzinsky V.E.,Papysheva O.V., Esipova L.N., Startseva N.M., Kotaish G.A. Features of medical care for gestational diabetes mellitus (in case of a specialized obstetric hospital). Obstetrics and Gynecology. 2018; (2): 108-14. (in Russian)].https://dx.doi.org/10.18565/aig.2018.2.108-114.
- Сухих Г.Т., Ход М. На пути к Европейскому консенсусу по гестационному сахарному диабету. Рациональное руководство по обследованию, лечению и уходу. Акушерство и гинекология. 2017; 4: 5-12. [Sukhikh G.T., Hod M. Towards a European сonsensus on пestational diabetes mellitus. A pragmatic guide for diagnosis, management, and care. Obstetrics and Gynecology. 2017; (4): 5-12. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.4.5-12.
- Аксенов А.Н., Бочарова И.И., Башакин Н.Ф., Троицкая М.В., Якубина А.А., Букина М.Ю., Бурумкулова Ф.Ф., Гурьева В.М. Особенности ранней постнатальной адаптации и ведения новорожденных, родившихся у матерей с гестационным сахарным диабетом. Российский вестник акушера-гинеколога. 2015; 15(4): 75-80. [Aksenov A.N., Bocharova I.I., Bashakin N.F., Troickaja M.V., Jakubina A.A., Bukina M.Ju., Burumkulova F.F., Gur'eva V.M. Features of early postnatal adaptation and management of newborns born to mothers with gestational diabetes mellitus. Russian Bulletin of 0bstetrician-Gynecologist. 2015; 15(4): 75-80. (in Russian)]. https://dx.doi.org/10.17116/rosakush201515475-80.
- Лысенко С.Н., Чечнева М.А., Петрухин В.А., Бурумкулова Ф.Ф., Ермакова Л.Б. Ультразвуковая диагностика диабетической фетопатии. Российский вестник акушера-гинеколога. 2016; 16(3): 23-30. [Lysenko S.N., Chechneva M.A., Petruhin V.A., Burumkulova F.F,Ermakova L.B. Ultrasound diagnosis of diabetic fetopathy. Russian Bulletin of Obstetrician-Gynecologist. 2016; 16(3): 23-30. (in Russian)].https://dx.doi.org/10.17116/rosakush201616323-30.
- Лысенко С.Н., Чечнева М.А., Петрухин В.А., Бурумкулова Ф.Ф. Оценка степени тяжести диабетической фетопатии. Российский вестник акушера-гинеколога. 2020; 20(1): 61-7. [Lysenko S.N., Chechneva M.A., Petruhin V.A., Burumkulova F.F. Assessment of the severity of diabetic fetopathy. Russian Bulletin of Obstetrician-Gynecologist. 2020; 20(1): 61-7.(in Russian)]. https://dx.doi.org/10.17116/rosakush20202001161.
- Chiefari E., Arcidiacono B., Foti D., Brunetti A. Gestational diabetes mellitus: an updated overview. J. Endocrinol. Invest. 2017; 40(9): 899-909.https://dx.doi.org/10.1007/s40618-016-0607-5.
- Плеханова М.А., Бурумкулова Ф.Ф., Петрухин В.А., Овчинникова В.В. Факторы риска развития впервые выявленной гипергликемии во время беременности. Российский вестник акушера-гинеколога. 2022; 22(1): 74-80. [Plehanova M.A., Burumkulova F.F., Petruhin V.A., Ovchinnikova V.V. Risk factors for the development of newly diagnosed hyperglycemia during pregnancy. Russian Bulletin of Obstetrician-Gynecologist. 2022; 22(1): 74-80. (in Russian)]. https://dx.doi.org/10.17116/rosakush20222201174.
- Zhang С., Rawal S., Chong Y.S. Risk factors for gestational diabetes: is prevention possible? Diabetologia. 2016; 59(7): 1385-90. https://dx.doi.org/10.1007/s00125-016-3979-3.
- Zhang C., Sundaram R., Maisog J., Calafat A.M., Barr D.B., Buck Louis G.M. A prospective study of prepregnancy serum concentrations of perfluorochemicals and the risk of gestational diabetes. Fertil. Steril. 2015; 103: 184-9.https://dx.doi.org/10.1016/j.fertnstert.2014.10.001.
- Garduño-Alanis A., Torres-Mejía G., Nava-Díaz P., Herrera-Villalobos J., Díaz-Arizmendi D., Mendieta-Zerón H. Association between a medical nutrition therapy program and eating behavior with gestational weight gain in women with diabetes. J. Matern. Fetal Neonatal Med. 2020; 33(24): 4049-54.https://dx.doi.org/10.1080/14767058.2019.1594764.
- Bao W., Tobias D.K., Hu F.B., Chavarro J.E., Zhang C. Pre-pregnancy potato consumption and risk of gestational diabetes mellitus: prospective cohort study. BMJ. 2016; 352: h6898. https://dx.doi.org/10.1136/bmj.h6898.
- Mijatovic-Vukas J., Capling L., Cheng S., Stamatakis E., Louie J., Cheung N.W. et al. Associations of diet and physical activity with risk for gestational diabetes mellitus: a systematic review and meta-analysis. Nutrients. 2018; 10(6): 698. https://dx.doi.org/10.3390/nu10060698.
- Marchetti D., Carrozzino D., Fraticelli F., Fulcheri M., Vitacolonna E. Quality of life in women with gestational diabetes mellitus: a systematic review. J. Diabetes Res. 2017; 2017: 7058082. https://dx.doi.org/10.1155/2017/7058082.
- Pantzartzis K.A., Manolopoulos P.P., Paschou S.A., Kazakos K., Kotsa K., Goulis D.G. Gestational diabetes mellitus and quality of life during the third trimester of pregnancy. Qual. Life Res. 2019; 28(5): 1349-54.https://dx.doi.org/10.1007/s11136-018-2090-2.
- Ghasemi F., Vakilian K., Khalajinia Z. Comparing the effect of individual counseling with counseling on social application on self-care and quality of life of women with gestational diabetes. Prim. Care Diabetes. 2021; 15(5): 842-7. https://dx.doi.org/10.1016/j.pcd.2021.05.009.
- Long Q., Guo J., Zhong Q., Jiang S., Wiley J., Chen J.L. General self-efficacy and social support as mediators of the association between perceived stress and quality of life among rural women with previous gestational diabetes mellitus. J. Clin. Nurs. 2021; 30(7-8): 1026-36. https://dx.doi.org/10.1111/jocn.15648.
- Ansarzadeh S., Salehi L., Mahmoodi Z., Mohammadbeigi A. Factors affecting the quality of life in women with gestational diabetes mellitus: a path analysis model. Health Qual. Life Outcomes. 2020; 18(1): 31. https://dx.doi.org/10.1186/s12955-020-01293-4.
- Ходжаева З.С., Снеткова Н.В., Клименченко Н.И., Абрамова М. Е., Дегтярева Е.И., Донников А.Е. Клинико-молекулярно-генетические детерминанты формирования гестационного сахарного диабета. Акушерство и гинекология. 2019; 4: 18-24. [Khodzhaeva Z.S., Snetkova N.V., Klimenchenko N.I., Abramova M.E., Degtyareva E.I., Donnikov A.E. Clinical and molecular genetic determinants of the development of gestational diabetes mellitus. Obstetrics and Gynecology. 2019; (4): 18-24. (in Russian)].https://dx.doi.org/10.18565/aig.2019.4.18-24.
- Абрамова М.Е., Ходжаева З.С., Горина К.А., Муминова К.Т., Горюнов К.В., Рагозин А.К., Силачев Д.Н. Гестационный сахарный диабет: скрининг и диагностические критерии в ранние сроки беременности. Акушерство и гинекология. 2021; 5: 25-32. [Abramova M.E., Khodzhaeva Z.S., Gorina K.A., Muminova K.T., Goryunov K.V., Ragozin A.K., Silachev D.N. Gestational diabetes mellitus: screening and diagnostic criteria in early pregnancy. Obstetrics and Gynecology. 2021; (5): 25-32. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.5.25-32.
- Ходжаева З.С., Абрамова М.Е., Муминова К.М., Горина К.А., Фролова Е.Р., Горюнов К.В., Силачев Д.Н., Шевцова Ю.А. Роль внеклеточных везикул плазмы как предикторов гестационного сахарного диабета в первом триместре беременности. Акушерство и гинекология. 2022; 4: 76-83. [Khodzhaeva Z.S., Abramova M.E., Muminova K.M., Gorina K.A., Frolova E.R., Goryunov K.V., Silachev D.N., Shevtsova Yu.A. The role of plasma extracellular vesicles as predictors of gestational diabetes mellitus in the first trimester of pregnancy. Obstetrics and Gynecology. 2022; (4): 76-83.(in Russian)]. https://dx.doi.org/10.18565/aig.2022.4.76-83.
Received 14.10.2022
Accepted 12.12.2022
About the Authors
Natalia V. Batrak, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Medical Genetics, Ivanovo State Medical Academy, Ministry of Health of the Russian Federation, 153012, Russia, Ivanovo, Sheremetevsky Ave., 8, +7(962)160-01-33, batrakn@inbox.ru, https://orcid.org/0000-0002-5230-9961Anna I. Malyshkina, Dr. Med. Sci., Professor, Director, Ivanovo Research Institute of Motherhood and Childhood named after V.N. Gorodkov, Ministry of Health of the Russian Federation, 153045, Russia, Ivanovo, Pobedy str., 20; Head of the Department of Obstetrics and Gynecology, Medical Genetics, Ivanovo State Medical Academy,
Ministry of Health of the Russian Federation, 153012, Russia, Ivanovo, Sheremetevsky Ave., 8, ivniimid@inbox.ru, https://orcid.org/0000-0002-1145-0563
Alina S. Tkachenko, 5th year student of the Faculty of Medicine, Ivanovo State Medical Academy, Ministry of Health of the Russian Federation,
153012, Russia, Ivanovo, Sheremetevsky Ave., +7(915)810-99-52, alina.tkachenkoisma@mail.ru, https://orcid.org/0000-0003-0550-6724
Corresponding author: Natalia V. Batrak, batrakn@inbox.ru