Adaptive capacities of full-term babies of breastfeeding age born in different cities of the Russian Federation
Aim. To investigate adaptive capacities of full-term babies of breastfeeding age born in different cities of the Russian Federation.Derevtsov V.V., Ivanov D.O., Kozlova L.V., Antonova L.K., Bekezin V.V., Neudakhin E.V.
Materials and methods. This was a cross-sectional (transverse) study involving 244 infants born at 37–42 weeks of gestation. Of them, 219 babies were from mothers with past extragenital diseases and a complicated obstetric and gynecological history. These infants were from St. Petersburg (group 1, n=110) and Smolensk (group 2, n=109). Twenty-five healthy children were from Tver (group 3). Children underwent serial examinations including cardiointervalography at the age of 1 (n=229), 3 (n=217), 6 (n=200), 12 (n=203) months. Statistical analysis was performed using nonparametric methods.
Results. On days 2–3, 75% and 68% of babies in groups 1 and 2, respectively, needed personalized recommendations. Children in group 1 were more likely to require non-drug and drug therapy than infants in group 2. At one month, 68% and 75% of children in groups 1 and 2, at three months 64% and 74% of children in groups 1 and 2, at six months 50% and 56% of children in groups 1 and 2, and at 12 months 54% and 60% of children in groups 1 and 2 needed such interventions. The majority of children in group 1 did not require personalized correction.
Conclusion. Children born in different cities of the Russian Federation had statistically significant differences in functional adaptation reserves. These differences were associated with maternal past extragenital diseases and a complicated obstetric and gynecological history regardless of the babies’ city of birth. Subsequently, they affect the health status of the children.
Keywords
The relevance of investigating the functional state of compensatory resources and body adaptation to detect early stages of the pathological process is beyond doubt [1–8]. Nevertheless, there is limited evidence about full-term infants born in different cities of Russia.
This study aimed to investigate adaptive capacities of full-term babies of breastfeeding age born in different cities of the Russian Federation.
Materials and methods
This was a cross-sectional (transverse) study (transverse) conducted at regular intervals [4] at the Saint-Petersburg State Pediatric Medical University (St.-Petersburg), Smolensk State Medical University (Smolensk), and Tver State Medical University (Tver). A limitation of the study is a small sample size.
The study groups included full-term neonates (at 37–42 week gestation) from neonatal care departments born by women with a complicated history, pregnancies, and childbirth. They were divided into those born in St. Petersburg (group 1) and Smolensk (group 2). Group 3 from Tver included infants from healthy women who had a healthy pregnancy and uncomplicated delivery at 38–40 weeks.
The study initially included 650 children on days 2–3 of life. Of these, 250 were not evaluated according to the inclusion criteria, 100 mothers refused to participate because they lived in rural areas, 30 refused for other reasons, and 270 children were assessed according to the inclusion criteria. From those evaluated according to the inclusion criteria, 15 were excluded, 11 refused to participate, and 244 children were included in the study. The data of 244 cardiointervalograms of children were available for analysis, including 110 in group 1, 109 in group 2, and 25 in group 3. At one month of age, data of 229 cardiointervalograms were available for analysis, including 101 in group 1 (9 dropped out at the request of legal representatives), 103 in group 2 (7 dropped out at the request of legal representatives), and 25 in group 3. In children at the age of 3 months, data of 217 cardiointervalograms were available for analysis, including 91 in group 1(10 dropped out at the request of legal representatives), 101 in group 2 (2 dropped out at the request of 2 legal representatives), and 25 in group 3. In children aged six months, data of 200 cardiointervalograms were available for analysis, including 85 (6 did not turn up due to acute respiratory infection), 90 in group 2(7 dropped out at the request of legal representatives, four did not turn up due to acute respiratory infection), and 25 in group 3. For children at the age of 12 months, the data of 203 cardiointervalograms were available for analysis. Eighty-six, 92, and 25 children in groups 1, 2, and 3 completed the study.
A total of 1093 cardiointervalograms performed according to the method [7] were analyzed. Babies’ adaptive capacities to environmental conditions were analyzed [4].
The study was approved by the Research Ethics Committees of the V. A. Almazov National Medical Research Center (extract from minutes No. 59 of 03.17.2014) and St. Petersburg State Pediatric Medical University (extract from minutes No. 12/3 dated 04.12.2017).
Statistical analysis
In addition to the statistical analysis [4], a 95% confidence interval (CI) for the relative rate (RR) was calculated using the EpiTools Web-Based Calculator https://epitools.ausvet.com.au/ztesttwo.
Results
Analysis of the data presented in Figure 1 showed statistically significant differences (Kolmogorov–Smirnov test, p <0.05). Thus, on days 2–3 of life, median Me SI1 (SI1 – index calculated as a result of analysis of cardiointervalograms, removal of which occurred at the child's resting point, prior to application of tilt-test) in the sample of children in group 1 was statistically significantly lower by 73 than among children in group 2 and by 170 than among children in group 3. Consequently, children in groups 1 and 2 had depleted compensatory resources, especially children in group 1. At one month of life, Me SI1 in children of group 1 was statistically significantly higher by 298 than in children of group 2, and by 144 than in children in group 3, that is, children in group 1 had strained compensatory resources, and children group 2 they were reduced. At three months of life, in children of group 1, Me SI1 was statistically significantly higher by 84 and 30 compared with children in groups 2 and 3, respectively. That is, children in group 1had stressed compensatory resources. At the same time, Me SI1 in children of group 2 was statistically significantly lower by 54 than in group 3. Therefore, in children of group 2, compensatory resources were reduced. At six months of age, Me SI1 in children of group 1 was statistically significantly higher by 85 than in children of group 2, less by 43 than in group 3. Therefore, group 1 had more stressed compensatory resources than children in group 2 and were reduced compared with group 3. At this age, the lowest compensatory resources were recorded in children of group 2. At 12 months of age, Me SI1 in children of groups 1 and 2 was statistically significantly lower than in group 3. At the same time, Me SI1 in children of group 2 was lower than in group 1. Thus, children in groups 1 and 2 had weakened compensatory resources, especially children in group 2.
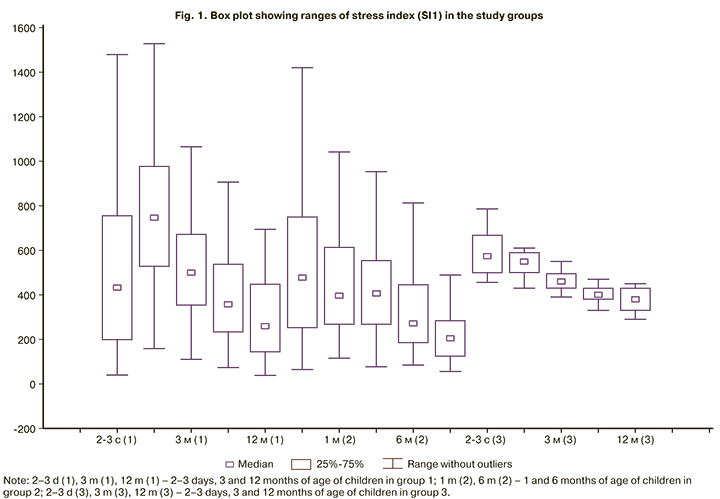
An analysis of the data presented in Figure 1 showed statistically significant differences between the study groups (Wilcoxon test). From days 2–3 to one month of life, Me SI1 in children of group1 increased statistically significantly by 290, p <0.01; that is, there was a tension of compensatory resources. From 1 to 3 months of life, Me SI1 in children of groups 1 and 3 decreased statistically significantly by 204 (p <0.01) and by 90 (p <0.01), respectively. Consequently, the stress of compensatory resources decreased. It should be emphasized that among children of group 1, the greatest (2 fold) decrease in the tension of compensatory resources was noted. From 3 to 6 months of life, Me SI1 in children of groups 1, 2, and 3 decreased statistically significantly by 133 (p <0.02), 134 (p <0.01), and 60 (p <0.01), respectively. Consequently, the stress of compensatory resources also decreased. Comparable changes occurred in children of groups 1 and 2, which were more pronounced than in group 3. In children of groups 1 and 2, compensatory resources during the 1st year of life decreased, especially in the 2nd half of the year, especially in children group 1.
As a result of the data analysis presented in Figure 2, statistically significant differences were found. At 2–3 days of life, children in group 1 had satisfactory adaptation 3.5 times less often, unsatisfactory – in 39% compared with group 3. At the age of 1 month, satisfactory adaptation was determined three times less often, unsatisfactory – in 24%. At three months, satisfactory adaptation was recorded two times less often, unsatisfactory – in 20%. At the age of 6 months, satisfactory adaptation was observed two times less often, unsatisfactory – in 13%. At 12 months, satisfactory adaptation was noted two times less often, unsatisfactory – in 26%.
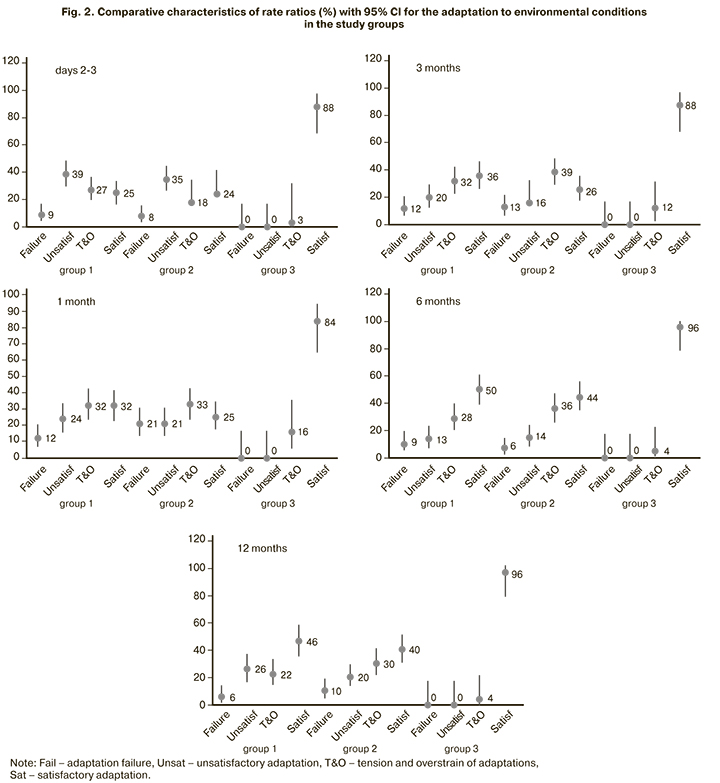
At 2–3 days of life, children in group 2 were three times less likely to have satisfactory adaptation than babies in group 3, and 35% had unsatisfactory adaptation. At the age of 1 month, satisfactory adaptation was also determined 3 times less often and was unsatisfactory in 21%. At the age of 3 months, satisfactory adaptation was also recorded three times less often and was unsatisfactory in 22%. At the age of 6 months, satisfactory adaptation is recorded two times less often and was unsatisfactory in 14%. At the age of 12 months, satisfactory adaptation is noted 2.5 times less often and was unsatisfactory in 30% (Fig. 2).
At 2–3 days of life, in children of groups 1 and 2, the frequency of satisfactory adaptation to environmental conditions was statistically significantly higher than the adaptation failure by 3 and 4 times, respectively. The stress and overstrain of adaptation was more significant than the adaptation failure, by 3 and 3 times, the frequency of unsatisfactory adaptation was greater than that of adaptation failure, by 4 and 4 times. At the age of 1 month, in group 1, the frequency of a satisfactory adaptation to environmental conditions was statistically significantly higher than that of adaptation failure by three times. The frequency of tension and overstrain was three times higher than that of adaptation failure. The same was observed at the age of 3 months. In children of group 2, the frequency of tension and overstrain adaptation was three times higher than adaptation failure. At the age of 6 months, in children of groups 1 and 2, the frequency of a satisfactory adaptation to environmental conditions was statistically significantly higher than unsatisfactory, 4 and 3 times, and adaptation failure by 5 and 8 times. The frequency of tension and overstrain was 3 and 6 times higher than that of adaptation failure. At the age of 12 months, in group 1, the frequency of satisfactory adaptation to environmental conditions was statistically significantly twice higher than that of tension and overstrain and was unsatisfactory by two times, adaptation failure by eight times. The frequency of tension and overstrain was four times greater than that of adaptation failure; the frequency of unsatisfactory adaptation was four times higher than failure. Simultaneously, in children of group 2, the frequency of satisfactory adaptation to environmental conditions was statistically significantly twice higher than that of unsatisfactory and adaptation failure by four times. Tension and overstrain were observed three times more often than adaptation failure. The changes revealed in groups 1 and 2 differed from that in children of group 3 (Fig. 2).
Discussion
Therefore, at 2–3 days of life, many children in groups 1 and 2 had unsatisfactory adaptation. As a result, 75% and 68% of children group 1 and 2, respectively, needed personalized recommendations. The type of measures, which depended on the degree of adaptation environmental conditions, we described in our earlier study [4]. At the age of 1 month, children in group 1 with the tension of compensatory resources had a high rate of unsatisfactory adaptation with a decrease in satisfactory one. In the structure of the group, stress and overstrain were more common than adaptation failure. Children in group 2 had a high rate of reduced compensatory resources. As a result, 68% and 75% of children group 1 and 2, respectively, needed personalized recommendations. At the age of 3 months, children in group 1, against the background of the stress of compensatory resources, the frequency of satisfactory adaptation was found less often. In this group, stress and overstrain were observed less frequently than adaptation failure. In group 2, most children with reduced compensatory resources had unsatisfactory adaptation. As a result, 64% and 74% of children in groups 1 and 2 needed personalized recommendations. At the age of 6 months, children in group 1 against the background of reduced compensatory resources, satisfactory adaptation was observed less often. In children of group 2, something different was observed. As a result, 50% and 56% of children in groups 1and 2 needed personalized recommendations. At the age of 12 months, children in group 1, against the background of reduced compensatory resources, often had unsatisfactory adaptation.
In this group, tension and overstrain prevailed, unsatisfactory adaptation dominated over its failure. Simultaneously, in children of group 2, against the background of reduced compensatory resources, the frequency of stress and overstrain prevailed with a decrease in satisfactory adaptation. In the structure of the sample, the frequency of tension and overstrain prevailed over adaptation failure. As a result, 54% and 60% of children in groups 1 and 2 needed personalized recommendations. In children of group 3 who were born healthy after uneventful pregnancies and childbirth, adaptation to environmental conditions was characterized by the prevalence of satisfactory adaptation. By contrast, children in groups 1 and 2 had reduced adaptation to environmental conditions. Undoubtedly, this fact indicates a decrease in the functional reserve of adaptation in such children, which was contributed by complicated maternal somatic and obstetric-gynecological anamnesis, regardless of the city of birth of full-term babies, and subsequently also by the health features of the children themselves. However, the cost of this restructuring remains unknown.
Since the study included practically healthy children from neonatal care departments, subsequently observed according to the outpatient-polyclinic principle of providing medical care, the results of this study should be helpful for healthcare organizers and doctors working in maternity wards, polyclinics, and hospitals.
Conclusion
Statistically significant differences found in compensatory resources and the adaptation to environmental conditions justify a personalized approach (high-risk strategy), including cardiointervalography with the consultation of a pediatric cardiologist and neurologist in the management of term infants on days 2–3, 1, 3, 6, 12 months of life. Such children need preventive measures (including courses of metabolic (adaptation enhancing) drugs). For any acute infectious and somatic diseases, hospitalization is recommended. Cardiointrevalography should be used to assess the results of preventive measures aimed to compensate for adaptive processes after diseases.
References
- Близнецова Е.А., Антонова Л.К., Малинин А.Н. Вегетативная регуляция в первые три месяца жизни у недоношенных детей, родившихся с задержкой внутриутробного развития. Педиатр. 2018; 9(4): 36-43. [Bliznetsova E.A., Antonova L.K., Malinin A.N. Vegetative regulation in the first three months of life in premature children born with intrauterine development delay. Pediatrician. 2018; 9(4): 36-43. (in Russian)]. https://dx.doi.org/10.17816/PED9436-43.
- Деревцов В.В., Козлова Л.В. Функциональное состояние вегетативной нервной системы и адаптация в раннем неонатальном периоде у детей от матерей с анемиями. Российский вестник перинатологии и педиатрии. 2010; 55(3): 14-9. [Derevtsov V.V., Kozlova L.V. Functional state of the autonomic nervous system and adaptation in the early neonatal period in children from mothers with anemia. Russian Bulletin of Perinatology and Pediatrics. 2010; 55(3): 14-9. (in Russian)].
- Дука Ю.М., Нагорнюк В.Т., Хало М.В. Характеристика течения адаптационного периода у новорожденных, рожденных от женщин с избыточной массой тела. Таврический медико-биологический вестник. 2015: 18(1): 30-6. [Duka Yu.M., Nagornyuk V.T., Khalo M.V. Characteristics of the course of the adaptation period in newborns born to overweight women. Tavrichesky medical and biological bulletin. 2015: 18(1): 30-6. (in Russian)].
- Иванов Д.О., Деревцов В.В., Серова Н.П. Оценка адаптации организма младенцев, рожденных с разными типами легкой степени тяжести замедления внутриутробного роста. Педиатр. 2019: 10(3): 5-16. [Ivanov D.O. Derevtsov V.V., Serova N.P. Assessment of adaptation of the organism of infants born with different types of light severity of intrauterine growth retardation. Pediatrician. 2019: 10(3): 5-16. (in Russian)]. https://dx.doi.org/10.17816/PED1035-16.
- Тумаева Т.С., Целкович Л.С., Науменко Е.И., Самошкина Е.С., Гарина С.В., Верещагина В.С., Широкова А.А. Особенности вегетативной регуляции у детей, перенесших внутриутробную гипоксию при различных способах родоразрешения, на первом году жизни. Вестник Уральской медицинской академической науки. 2018: 15(6): 814-23. [Tumaeva T.S., Tselkovich L.S., Naumenko E.I., Samoshkina E.S. at al. Especially vegetative regulation in children who have undergone intrauterine hypoxia, with different methods of delivery in the first year of life. Bulletin of the Ural medical Academy. 2018: 15(6): 814-23. (in Russian)]. https://dx.doi.org/10.22138/2500-0918-2018-15-6-814-823.
- Холодова И.Н., Зайденварг Г.Е., Горяйнова А.Н. Дети после кесарева сечения: как улучшить их адаптацию и уменьшить риск развития патологических состояний. Медицинский совет. 2019; 11: 16-22. [Kholodova I.N., Zaydenvarg G.E., Goryainova A.N. Children after cesarean section: how to improve their adaptation and reduce the risk of developing pathological conditions. Medical Council. 2019: 11: 16-22. (in Russian)]. https://dx.doi.org/10.21518/2079-701X-2019-11-16-22.
- Шиляев Р.Р., Неудахин Е.В. Детская вегетология. М.: Медпрактика-М; 2008; 408 c. [Shilyaev R.R., Neudakhin E.V. Children's vegetology. Moscow: Medpraktika-M, 2008; 408 p. (in Russian)].
- Неудахин Е.В. Теоретическое и практическое значение новых представлений о хронической стрессовой реакции у детей. Quantum Satis. 2019; 1(1): 10-9. [Neudakhin E.V. Theoretical and practical significance of new ideas about chronic stress reaction in children. Quantum Satis. 2019; 1(1): 10-9. (in Russian)].
Received 02.06.2020
Accepted 29.12.2020
About the Authors
Vitaly V. Derevtsov, Dr. Med. Sci., Consultant at the Department of Child’s Health Care, Directorate of Hospital Care of the Ministry of Health of Moscow region.Tel.: +7(498)602-29-71. E-mail: Vitaly21081981@yandex.ru. ORCID: 0000-0002-8819-7033. 1 Stroiteley b-r, Krasnogorsk, Moscow region, Russia, 143407.
Dmitry O. Ivanov, Dr. Med. Sci., Professor, Rector of the Saint-Petersburg State Pediatric Medical University, Chief Neonatologist of Minzdrav of Russia.
Tel.: +7(812)416-54-04. E-mail: doivanov@yandex.ru. ORCID: 0000-0002-0060-4168. 2 Litovskaya str., St. Petersburg, Russia, 194100.
Lyudmila V. Kozlova, Dr. Med. Sci., Professor at the Smolensk State Medical University of Minzdrav of Russia. Tel.: +7(4812)55-02-75.
E-mail: milkozlova@yandex.ru. 28 Krupskaya str., Smolensk, Russia, 214019.
Lyudmila K. Antonova, Dr. Med. Sci., Professor at the Departments of Polyclinic Pediatrics and Neonatology, Tver State Medical University of Minzdrav of Russia.
Tel.: +7(4822)32-17-79. E-mail: antonova.lk@yandex.ru. ORCID: 0000-0002-5587-5969. 4 Sovetskaya str., Tver, Russia, 170100.
Vladimir V. Вekezin, Dr. Med. Sci., Professor, Vice-Rector for Research, Head of the Department of Children's Diseases, Smolensk State Medical University of Minzdrav of Russia. Tel.: +7(4812)55-02-75. E-mail: smolenskbvv@yandex.ru. ORCID: 0000-0001-9141-5348. 28 Krupskaya str., Smolensk, Russia, 214019.
Yevgeny V. Neudakhin, Dr. Med. Sci., Professor, Merited Doctor of the Russian Federation, Chief Researcher, St. Lukaʼs Clinical Research Center for Children.
Tel.: +7(499)638-35-01. Е-mail: pediatr_ev@mail.ru. ORCID: 0000-0002-9124-1306. 38 Aviatorov str., Moscow, Russia, 119620.
For citation: Derevtsov V.V., Ivanov D.O., Kozlova L.V., Antonova L.K., Bekezin V.V., Neudakhin E.V. Adaptive capacities of full-term babies
of breastfeeding age born in different cities of the Russian Federation.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 4: 128-133 (in Russian)
https://dx.doi.org/10.18565/aig.2021.4.128-133



