В последние годы неуклонно увеличивается количество малоинвазивных хирургических вмешательств, кажущаяся простота которых повышает требовательность пациентов к качеству анестезиологического пособия. Поэтому является актуальным вопрос выбора методик, не только обеспечивающих безопасность и эффективность, но и позволяющих осуществлять адекватное обезболивание и комфортность периоперационного периода.
Эффективная антиноцицептивная защита должна строиться на принципах мультимодальной периоперационной анальгезии и многоуровневого подавления ноцицептивной импульсации. Включение в протокол обезболивания регионарных блокад позволяет воздействовать на уровне начальных этапов зарождения болевого синдрома – процессов трансдукции и трансмиссии, с одновременной блокадой вегетативных эфферентных волокон, что ведет к уменьшению симпатических влияний и обеспечивает стресс-лимитирующий эффект.
Как в общехирургической практике, так и при акушерско-гинекологических вмешательствах ведутся активные исследования по применению в рамках мультимодальной анестезии новых методов регионарного обезболивания на основе миофасциальных блоков, способных стать альтернативой центральным нейроаксиальным блокадам. К таким методам относятся блоки поперечного пространства живота (Transversus abdominis plane block, TAP-блок), блок квадратной поясничной мышцы (Quadratus Lumborum Block, QLB), блокада фасциального влагалища разгибателя спины (m. еrector spinae) (Erector Spinae Plane Block, ESP-блок), ретроламинарный блок (Retrolaminar Block, RLB), выполняемые с применением ультразвуковой навигации. Привлекательность миофасциальных блоков связана с низким риском нейрососудистых осложнений и относительной технической простотой выполнения по сравнению с эпидуральной или паравертебральной блокадой. Появившись сравнительно недавно, данные блоки все чаще рекомендуются исследователями в качестве компонента Enhanced Recovery After Surgery (ERAS), обеспечивающего раннюю активизацию пациента в условиях качественного мультимодального обезболивания.
Блокада поперечного пространства живота (ТАР-блок)
Согласно клиническим рекомендациям по анестезии, интенсивной терапии и реанимации в акушерстве и гинекологии от 2017 г., альтернативой эпидуральной анальгезии для послеоперационного обезболивания при кесаревом сечении могут служить билатеральный TAP-блок и субфасциальная инфузия местного анестетика (МА) в области операционной раны [1].
При ТАР-блоке МА воздействует на передние ветви грудных спинномозговых нервов ТhVII–ТhXII, а также подвздошно-подчревный и подвздошно-паховый нервы, берущие свое начало от корешка LI, обеспечивая анестезию передней и латеральной брюшной стенки [2–4].
В зависимости от точки доступа выделяют подреберный, латеральный и задний TAP-блоки и их сочетание; МА при этом вводится между прямой и поперечными мышцами живота и/или между внутренней косой и поперечной мышцами живота. Ни один из вариантов TAP-блока не обеспечивает блокады висцеральных ноцицептивных импульсов, но значительно уменьшает выраженность соматического компонента боли; возможно, именно с этим фактом связаны противоречивые данные о его эффективности в гинекологической практике [4–7].
Блокада квадратной поясничной мышцы (QLB)
В 2007 г. Рафаэлем Бланко был впервые предложен в качестве метода послеоперационной анальгезии QLB, который первоначально был назван им как задний TAP-блок [8]. Детальное описание техники выполнения данного блока было опубликовано в 2013 г., учитывая существенную разницу в глубине выполнения, анатомических и ультразвуковых ориентирах и в механизме действия, блок получил самостоятельное название Quadratus Lumborum Block (QLB) [9]. В отличие от TAP-блока QLB эффективно блокирует соматическую и интенсивную висцеральную боль и в настоящее время широко используется для лечения острой послеоперационной боли во многих областях хирургии, включая урологию, абдоминальную хирургию, гинекологию и ортопедию [10–14].
Квадратная мышца поясницы (m. quadratus lumborum) – это плоская парная четырехугольная мышца, точками прикрепления которой являются: гребень подвздошной кости, подвздошно-поясничная связка, поперечные отростки поясничных позвонков LI–LIV и нижний край XII ребра. Дополнительными анатомическими ориентирами для выполнения QLB служат: большая поясничная мышца (m. psoas major) и мышца, выпрямляющая позвоночник (m. erector spinae). Характерную картину, получаемую при ультразвуковой визуализации данных мышц, J. Borglum [15] описал как «знак трилистника». QLB выполняется исключительно под контролем ультразвука, а прохождение иглы и место применения МА находятся далеко от органов брюшной полости, магистральных сосудов и брюшной полости.
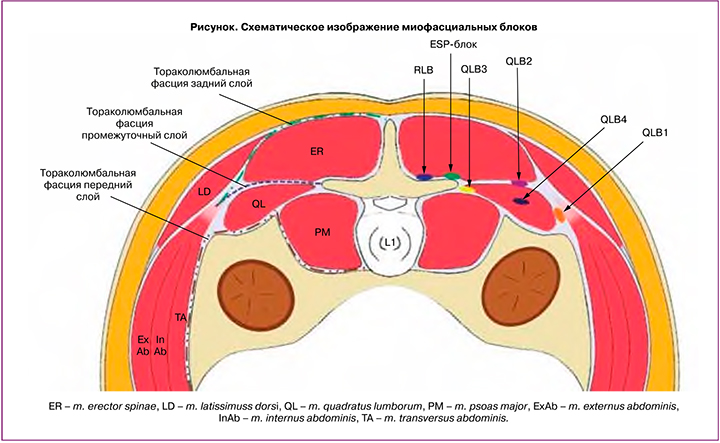
До настоящего времени при описании блоков сохранялась некоторая номенклатурная и методологическая путаница. H. Ueshima [13] была предложена классификация QLB в зависимости от окончательного положения иглы по отношению к m. quadratus lumborum и зоны введения раствора МА (рисунок):
- QLB1 (латеральный) – МА вводится в зоне прилегания латерального края m. quadratus lumborum к поперечной фасции;
- QLB2 (задний) – МА вводится между медиальным листком пояснично-грудной фасции и задней частью m. quadratus lumborum;
- QLB3 (передний) – МА вводится перед m. quadratus lumborum в зоне ее прилегания к поперечному отростку поясничного позвонка;
- QLB4 (интрамускулярный) – МА вводится непосредственно в толщу m. quadratus lumborum.
Кроме того, указанные выше блоки могут быть выполнены от субкостального уровня до уровня LIV, что, безусловно, в совокупности с объемом вводимого препарата не может не влиять на уровень распространения сенсорной блокады [13, 16, 17].
Во всех случаях предполагается, что введенный МА будет в той или иной мере распространяться под медиальной и латеральной дугообразными связками диафрагмы в грудное паравертебральное пространство, а также проходить вдоль m. рsoas major, воздействуя на ветви поясничного сплетения. На сегодняшний день недостаточно данных о преобладающих паттернах распространения МА и преимуществах в клинической эффективности того или иного вида QLB. Согласно последним клиническим исследованиям, уровень сенсорной блокады при QLB распространяется от ThVI–ThVII до LI–LII, обеспечивая эффективную анальгезию на уровне ThVI–VII–LI–IV дерматомов, а также блокаду n. iliohypogastricus и n. ilioinguinalis [13, 14, 16–18].
Однозначных данных о механизме анальгетического действия QLB пока не получено. J. Carney et al. [19] с помощью магнитно-резонансной томографии было выявлено паравертебральное распространение контраста при QLB1 краниально – до уровня ThV, каудально – до уровня LI, в то время как при TAP-блоке распространение контраста было ограничено областью поперечной плоскости живота и обеспечивало сенсорный блок только в рамках иннервации ThIX–LI. Распространение в грудное паравертебральное пространство подтверждено также исследованием на трупах, проведенным M. Dam et al. [20] при QLB4. В данной работе также выявлено распространение красителя в межреберные промежутки с прокрашиванием соматических нервов, торакального симпатического ствола, n. iliohypogastricus и n. ilioinguinalis. Аналогичные данные получены Н. Elsharkawy [14] при выполнении QLB3. Однако в исследовании S. Adhikary et al. [21] при QLB4 было продемонстрировано распространение раствора в поясничное паравертебральное пространство, но не подтверждено распространение в грудное паравертебральное пространство. Об отсутствии паравертебрального распространения свидетельствует и исследование A. Kumar et al. [22], результаты которого показывают, что контраст, введенный в область m. quadratus lumborum, не распространяется в паравертебральное пространство, а контраст, введенный в паравертебральное пространство, не перетекает в область m. quadratus lumborum. Из возможных точек приложения, обеспечивающих висцеральную блокаду, обсуждается действие МА на чревный ганглий и /или на симпатические ветви спланхнических нервов [11, 13, 14].
Учитывая противоречивые данные, касающиеся паравертебрального распространения МА, анальгетическое действие QLB может быть связано с анатомо-гистологическими характеристиками торако-люмбальной фасции (fasciae thoracolumbalis, TLF) [11, 13, 14].
TLF представляет собой сложную трубчатую структуру соединительной ткани, образованную связующими апоневрозами и слоями фасции, которая охватывает мышцы спины. При описании TLF используется двух- либо трехкомпонентная модель ее строения [11, 14]. Согласно трехкомпонентной модели, различают три листка TLF: задний, средний и передний. Задний и средний листки покрывают соответственно дорсальную и вентральную поверхность m. еrector spinae, срастаясь по латеральному краю данной мышцы. Передний листок покрывает вентральную поверхность m. quadratus lumborum и латерально переходит в поясничную фасцию. В двухслойной модели TLF выделяют поверхностный (задний) и глубокий (передний) слои, идентичные соответственно заднему и среднему листкам трехслойной модели, а слой фасции, покрывающий переднюю поверхность m. quadratus lumborum, считают продолжением трансверсальной фасции. TLF тесно связана с эндоторакальной фасцией, что обеспечивает потенциальный путь распространения МА в грудную полость и паравертебральное пространство. Кроме того, TLF соединяет поясничную паравертебральную область с переднелатеральной брюшной стенкой.
Последние данные свидетельствуют о том, что фасциальная ткань, вместо того, чтобы быть «пассивным» каркасом, является более сложной структурой с богатой сосудистой и сенсорной иннервацией. В поверхностном слое TLF имеются густая сеть симпатических нейронов, высокопороговые и низкопороговые механорецепторы, болевые рецепторы, играющие роль в развитии как острой, так и хронической боли. Анальгезия при QLB может быть, по крайней мере частично, объяснена блокадой этих рецепторов [11, 14].
Блокада m. quadratus lumborum в последние годы активно используется для послеоперационной анальгезии в акушерстве и гинекологии. Согласно данным рандомизированных клинических исследований (РКИ), применение QLB2 [10, 23, 24] QLB4 [25, 26] и QLB1 [27] для послеоперационного обезболивания при кесаревом сечении обеспечивает опиоидсберегающий эффект и значительно уменьшает показатели боли в покое и во время движения. W. Kang [28] в своем исследовании приводит данные о том, что сочетанное использование QLB2 и QLB3 в послеоперационном периоде при кесаревом сечении может стать альтернативой интратекальному введению морфина.
Результаты проведенного Xu M. et al. [29] метаанализа 12 РКИ c участием 904 пациенток с применением QLB для послеоперационной анальгезии при кесаревом сечении подтверждают его эффективное анальгетическое действие – уменьшение 12-часовой оценки боли в покое и во время движения, а также значительное снижение послеоперационного потребления опиоидов. Результаты метаанализа 16 РКИ с применением QLB для послеоперационной анальгезии в хирургической практике, проведенного Jin Z. et al. [30], подтверждают опиоидсберегающий эффект QLB при кесаревом сечении, но авторы констатируют недостаточность и неоднородность данных для проведения оценки QLB при других типах операций.
По данным Fujimoto H. et al. [31], QLB2 не улучшал качество послеоперационной анальгезии и качество восстановления, оцениваемого по шкале Quality of Recovery 40 (QoR-40) после гинекологических лапароскопических вмешательств. Ishio J. et al. [12] показано, что QLB2 в течение 24 часов значительно уменьшает послеоперационную боль при движении и в покое после лапароскопических гинекологических операций. По данным Yousef et al. [32], двусторонний QLB1 обеспечивает лучшую интраоперационную и послеоперационную анальгезию с меньшим потреблением опиоидов по сравнению с двусторонним TAP-блоком у пациенток, перенесших абдоминальную гистерэктомию.
Аналогичные данные получены при сравнении QLB1 с латеральным TAP-блоком при лапароскопических операциях на яичниках в работе Murouchi et al. [18], где показано, что QLB обеспечивал более длительный и распространенный анальгетический эффект. Кроме того, обнаружено, что при введении одинаковых суммарных доз при TAP-блоке пиковый уровень концентрации МА в крови были выше, чем при QLB. Это, возможно, объясняется следующим: во время QLB часть вводимого препарата перемещается из межмышечного пространства в паравертебральное, которое заполнено жировой тканью, где локальная тканевая перфузия низкая, следовательно, и низкая скорость абсорбции МА в кровь [32]. Данные исследования Blanco et al. [23] подтверждают преимущество QLB2 в сравнении с TAP-блоком в послеоперационном периоде при кесаревом сечении. Эти данные согласуются с данными трех метаанализов [33–35], в которых показано, что QLB обеспечивал более эффективную периоперационную анальгезию с меньшим потреблением опиоидов и более низкими баллами по визуальной аналоговой шкале в течение 24 часов после операции по сравнению с TAP-блоком.
Описано эффективное применение QLB1 для купирования выраженного болевого синдрома при эмболизации маточных артерий [36].
Однако объективную оценку эффективности QLB затрудняют: недостаточность накопленного клинического материала, его гетерогенность, отсутствие единой терминологии и методологических подходов, низкая частота использования исследователями стандартизированных конечных точек оценки периоперационного периода.
Блокада фасциального пространства m. еrector spinae (ESP-блок) и ретроламинарный блок (RLB)
В 2016 г. Forero М. et al. описан и введен в клиническую практику ESP-блок [37]. Инъекция МА при данном виде блока производится между фасцией, покрывающей m. erector spinae, и задней поверхностью поперечного отростка целевого позвонка на уровнях от ТhIII до LIV в зависимости от вида хирургического вмешательства [37, 38]. ESP-блок технически проще в исполнении, чем QLB, имеет четкие анатомические ориентиры – остистый отросток целевого позвонка и легко идентифицируемую m. erector spinae. Простота использования блока в сочетании с его теоретическим профилем безопасности, вероятно, ответственна за расширение его использования [38].
ESP-блок, первоначально применявшийся в торакальной хирургии, «спустившись» на уровень ниже ThVII, в настоящее время применяется для купирования послеоперационного болевого синдрома в абдоминальной хирургии и ортопедии [39–42]. Аналогично QLB, ESP-блок воздействует как на висцеральные, так и на соматические компоненты болевого синдрома, однако точный механизм развития данного блока пока не установлен. Предполагаются два пути распространения МА: во-первых, паравертебральный, с блокадой вентральных и дорсальных ветвей спинномозговых нервов и спинальных ганглиев; во-вторых, латеральный путь с вовлечением латеральной кожной ветви и мелких ветвей межреберных нервов [43, 44].
В 2006 г. Pfeiffer G. et al. [45] был описан RLB или, как еще его называют, паравертебральный преламинарный блок, выполняемый более медиально по отношению к целевому остистому отростку, чем ESP-блок (1,0–1,5 см от надостистой линии при RLB и 2–3 см – при ESP-блоке). В отличие от классической паравертебральной блокады при RLB раствор МА вводится дорсально по отношению к пластинке дуги целевого позвонка. RLB выполняется как «вслепую» [45], так и под ультразвуковым контролем [46, 47]. Механизм действия данного блока близок к механизму действия ESP-блока [47]; кроме того, при использовании обеих техник при магнитно-резонансной томографии было отмечено распространение местного анестетика через межпозвоночные отверстия в паравертебральное и эпидуральное пространство на уровне 2–5 позвонков от уровня инъекции [40, 47].
В последние два года отмечается увеличение количества статей, содержащих как описания клинических случаев, так и результаты РКИ применения ESP-блока для послеоперационного обезболивания в гинекологической практике. Описано применение ESP-блока для послеоперационного обезболивания при открытой миомэктомии и гистерэктомии [48, 49], кесаревом сечении [50]. Выводы, содержащиеся в данных публикациях, свидетельствуют о том, что ESP-блок обеспечивает эффективную анальгезию и снижение послеоперационного использования опиоидов и согласуются с результатами метаанализа, проведенного Kendall M.C. et al. [39].
Противопоказания к проведению миофасциальных блоков
Абсолютными противопоказаниями к проведению миофасциальных блоков являются: отказ пациента, местная инфекция в области проведения процедуры, аллергические реакции на МА. Относительные противопоказания включают: анатомические особенности пациента, нестабильность гемодинамики, неврологические нарушения. Некоторые исследователи предполагают, что их применение достаточно безопасно у пациентов с коагулопатиями и при приеме антикоагулянтов; однако в рекомендациях Американского общества региональной анестезии от 2017 г. указано на высокий риск осложнений при проведении глубоких региональных анестезирующих процедур у данной категории пациентов.
Препараты, применяемые для миофасциальных блоков
Для миофасциальных блокад в подавляющем большинстве случаев используют ропивакаин, бупивакаин, левобупивакаин. Однако нет единого мнения об оптимальном объеме и концентрации вводимого препарата. Как правило, используется от 10 до 30 мл раствора МА, вводимого билатерально, в концентрации 0,125–0,375%. Следует помнить, что максимальная доза ропивакаина не должна превышать 3 мг/кг, бупивакаина – 2,5 мг/кг. Описано как однократное, так и продленное применение МА с использованием катетера [11, 38].
Из адъювантов большинство авторов указывают на использование адреналина, уменьшающего абсорбцию МА и являющегося индикатором в случае непреднамеренного внутрисосудистого введения раствора. Проводятся исследования целесообразности добавления к раствору МА 4–8 мг дексаметазона, позволяющего увеличить продолжительность блока и его анальгетический и опиоидсберегающий эффект. Перспективным считается использование липосомальных форм бупивакаина [4, 11].
Осложнения миофасциальных блоков
Считается, что миофасциальные блоки более безопасны, чем нейроаксиальные блокады. Риск инфекционных осложнений не превышает таковой при внутримышечных инъекциях. Выполнение блока под ультразвуковой навигацией, с обязательным контролем положения кончика иглы перед инъекцией препарата, значительно повышает уровень безопасности и эффективности. Удаленность места пункции и введения местного анестетика при QLB, ESP и RLB от брюшной полости, внутренних органов и крупных кровеносных сосудов минимизирует возможность их механической травмы. Отсутствие необходимости проведения манипуляций вблизи крупных нервных стволов сводит к минимуму риск неврологических осложнений.
При всех типах QLB и при ESP-блоке [11, 14, 42] описаны случаи длительной моторной блокады четырехглавой мышцы бедра, что связано либо с паравертебральным распространением раствора МА, либо с вовлечением в блокаду поясничного сплетения и бедренного нерва. Описаны случаи транзиторной гипотонии при QLB2 [14], которые авторы объясняют паравертебральным распространением МА и развитием симпатической блокады.
Билатеральное введение требует относительно высоких объемов МА, что ведет к увеличению риска развития LAST (local anaesthetic system toxicity). Зарегистрированы случаи развития LAST при TAP-блоке, потребовавшие проведения реанимационных мероприятий [4]. Развитие LAST при QLB, ESP-блоке и RLB в литературе не описано. Однако необходимо учитывать, что связывание МА с белками плазмы максимально снижено на поздних сроках беременности, что ведет к увеличению концентрации свободного МА в плазме. Более того, биохимические и гормональные изменения во время беременности повышают чувствительность нейронов к МА, а также могут снижать порог судорог и развитие LAST. Поэтому целесообразно ограничить дозировку МА для периферических и центральных нейроаксиальных блокад у данной категории пациенток.
Заключение
Постепенно накапливаются данные, свидетельствующие об эффективности и безопасности вышеуказанных блоков. Более того, при увеличении количества малоинвазивных хирургических вмешательств миофасциальные блоки занимают прочные позиции в схемах мультимодальной анестезии. С учетом минимального количества осложнений, возможности ранней активизации и быстрой реабилитации пациентов, в некоторых случаях их использование предпочтительнее применения центральных нейроаксиальных блокад.
Возможность воздействия на висцеральный компонент боли при QLB, ESP-блоке и RLB является многообещающим фактором в плане их применения для послеоперационного обезболивания, что детерминирует необходимость более пристального изучения анатомических субстратов точек приложения, механизмов действия и клинических аспектов применения данных блоков.