New classification of hypospadias in girls according to modern concepts of disorders of sexual development and surgical management strategy
Objective: To optimize the classification of hypospadias in girls based on a review of the literature and experience with this pathology.Anikiev A.V., Okulov A.B., Volodko E.A., Brovin D.N., Andreeva E.N., Mokrysheva N.G.
Materials and methods: The study included follow-up data from 114 female hypospadias patients aged from 6 months to 42 years. All patients were diagnosed with different variants of disorders of sexual development (DSD) including salt-wasting congenital adrenal hyperplasia (CAH) (n=79), virile form of CAH (n=17), idiopathic virilization (n=3), mixed dysgenesis of gonads (n=2), partial dysgenesis of gonads (n=3), and hypospadias due to urethral malformation (n=10). All patients with urogenital sinus underwent surgery. Urethral transposition was performed in three patients with vestibular and vestibulovaginal forms of hypospadias complicated by recurrent urinary tract infection. Two girls with total hypospadias underwent surgery for upper urinary tract malformations and urinary incontinence.
Results: Based on the observations presented, we proposed a new classification of hypospadias in girls:
1. Hypospadias due to urethral malformations
a) Vestibular;
b) Vestibulovaginal;
c) Total.
2. Hypospadias due to virilization of the external genitalia
a) Urogenital sinus
1) Mild form;
2) Medium form;
3) Severe form.
b) Low-vaginal ectopia of the external urethral opening
c) High-vaginal ectopia of the external urethral opening.
Conclusion: The new classification will help to determine the rational surgical management strategy for hypospadias in girls and facilitate the interaction of physicians of different specialties.
Keywords
Female hypospadias is one of the clinical manifestations of female disorders of sexual development (DSD) and is characterized by urethral shortening and ectopy of the external urethral opening [1, 2]. Current classifications of female hypospadias do not take into account the full range of its forms and have a number of contradictions associated with the changed concepts of disorders of sexual development and optimal surgical management strategy.
This study aimed to optimize the classification of hypospadias in girls based on a review of the literature and experience with this pathology.
Materials and methods
The study included follow-up data of 114 female hypospadias patients aged 6 months to 42 years. All patients were examined to verify the DSD variant and choose the treatment strategy. A multidisciplinary team of specialists including pediatric endocrinologists, surgeons, urologists, andrologists, gynecologists, geneticists, radiation diagnosticians, laboratory technicians, pathomorphologists, psychologists, and pubertal sexologists participated in the diagnosis, decision-making regarding treatment of the patients. Patients with urogenital sinus (UGS) or suspected UGS when the external orifice of the urethra was not defined in the vaginal vestibule area underwent karyotyping and testing for major sex hormones (testosterone, Estradiol), gonadotropins (luteinizing and follicle-stimulating hormones), adrenal function (adrenocorticotropic hormone, renin, cortisol, aldosterone, 17-hydroxyprogesterone, 21-deoxycortisol, DHEA-C).
In patients with male 46.XU and 45.X/46.XU mosaic karyotypes, the pelvic organs were examined by open revision and/or diagnostic laparoscopy [3] along with medical genetic counseling and examination of sexual function followed by histological examination of the removed gonads and Mullerian structures to specify the diagnosis. At the late diagnosis of the disease in three prepubertal female patients with partial dysgenesis of the gonads, a psychologist was consulted to clarify the mental gender identity.
Genitourinary organs were examined in several stages. All patients underwent an echographic examination of the kidneys, bladder, and pelvis to visualize their anatomy and detect malformations. X-ray contrast, including urography, cystourethrography, and cystourethrovaginography, was performed in 12 girls to diagnose upper urinary tract abnormalities suspected echographically and in cases of previous pyelonephritis. The combined pelvic examination (8 patients) by echography and sinusocystourethroovaginoscopy was the most informative and, at a certain stage, allowed the abandonment of cystourethroovaginography. If the echographic data did not allow an adequate assessment of the pelvic structure, we performed magnetic resonance imaging (21 patients). In patients with UGS, the level of urethrovaginal fusion in relation to the pelvic diaphragm was determined during sinusocystourethroovaginoscopy or intraoperatively during introitoplasty. Forms of UGS were classified as mild, moderate, and severe. As a result of the study, all patients with UGS were diagnosed with different variants of DSD corresponding to the current classification [4] (Table 1).
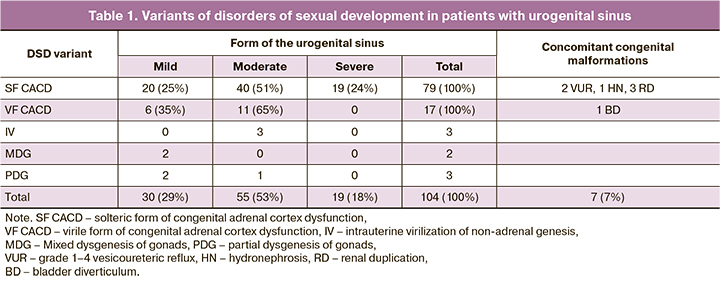
Patients with hypospadias due to urethral malformation (n=10) urinary tract were evaluated using renal function tests, microbiological, endoscopic examination of the urogenital tract, contrast studies with cystourethrography and urography and/or nephroscintigraphy, echography and MRI of the urinary tract and pelvic organs. Hypospadias were classified as vestibular, vestibulovaginal, and total (Table 2).
Patients with vestibular (n=2) and vestibulovaginal (n=1) hypospadias due to urethral malformation underwent urethral transposition [5] because of recurrent urinary tract infection. The girls with total hypospadias (n=2) underwent surgery for upper urinary tract malformations in infancy. Comprehensive treatment including injection of bulking agent into the bladder neck and pharmacotherapy aimed at urine retention was carried out at early and school age. Urinary and genital tract separation interventions were planned.
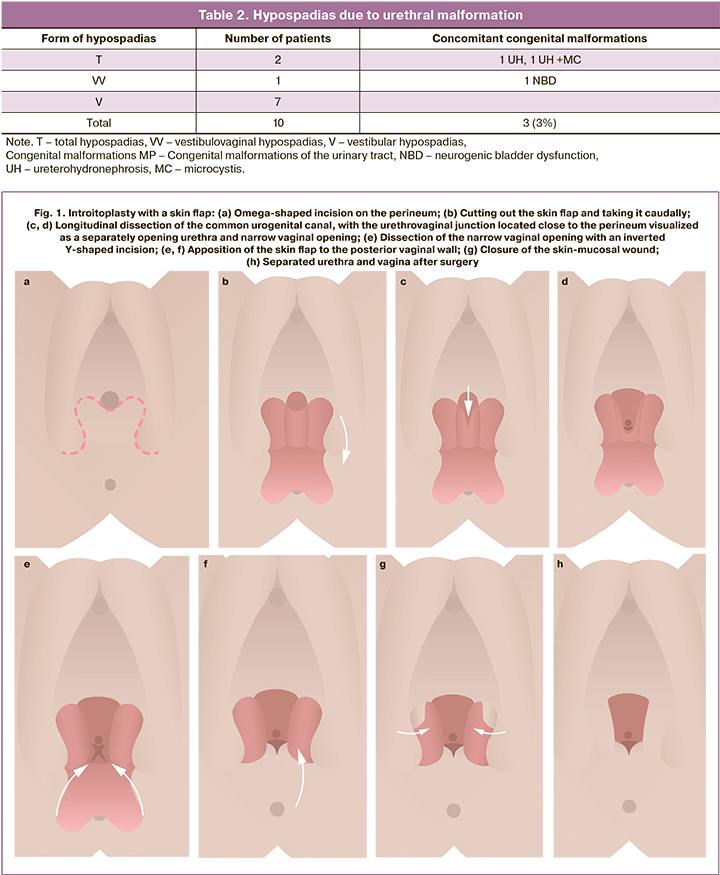
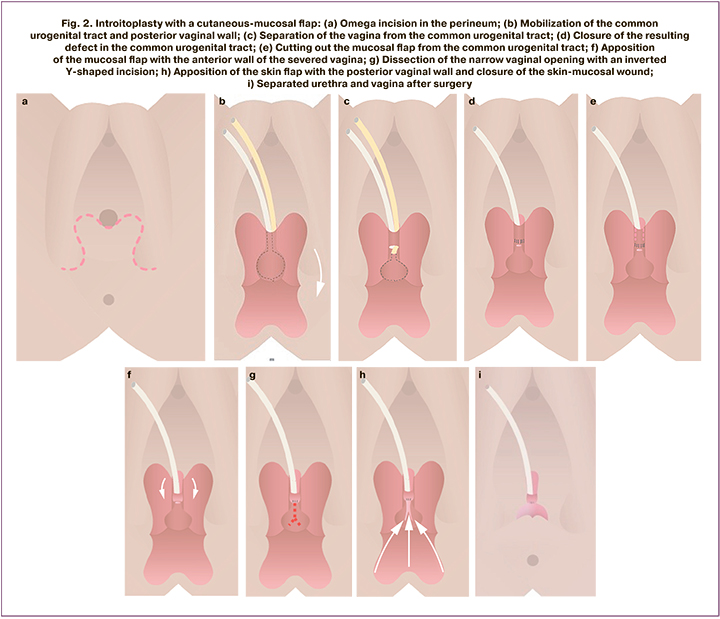
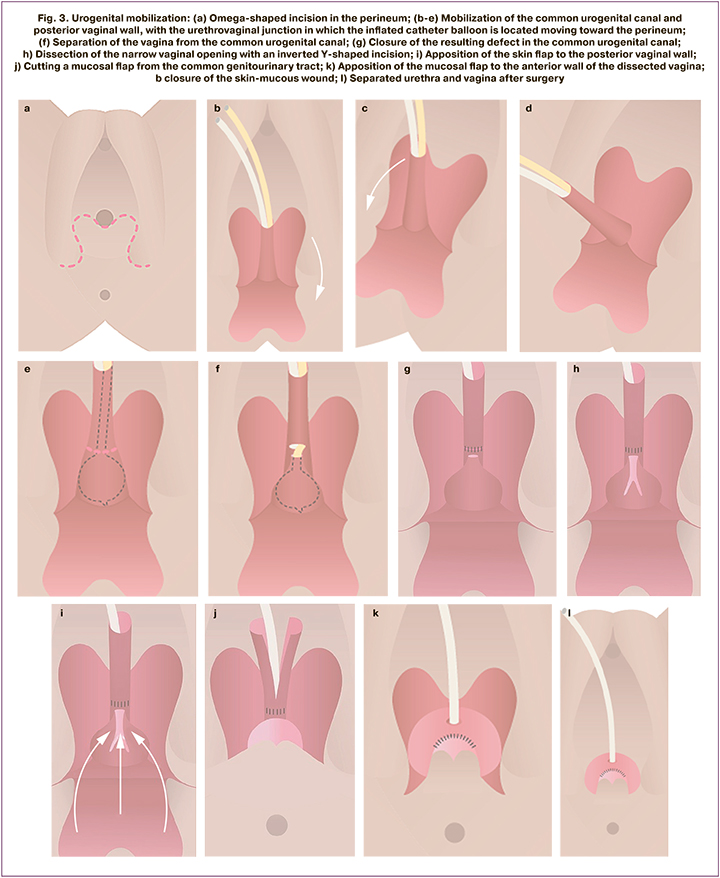
All patients with UGS underwent surgery, including introitoplasty in 104 patients; 15 of them were infants with congenital adrenal cortical dysfunction (CAH) and 89 were pubertal patients with various variants of DSD. Four types of interventions depending on the severity of UGS were used. Sinusotomy was performed in patients with mild UGS combined with a wide vaginal orifice. Dermal flap introitoplasty was performed for mild UGS combined with a narrow vaginal orifice (Fig. 1). Introitoplasty with a dermal mucosal flap was performed for the moderate form of UGS (Fig. 2). Urogenital mobilization was performed for severe UGS (Fig. 3). Patients with CAH of breastfeeding age underwent simultaneous repair of the hypertrophic clitoris and the labia minora.
Part of the patients who underwent skin flap introitoplasty without regard for the severity of UGS at pubertal age were observed for hypospadias in the form of low (n=17) and high (n=4) ectopy of the external urethral opening into the vagina.
Results
Based on the observations presented, we proposed a new classification of hypospadias in girls. The classification included two groups with different etiologies and surgical treatment approaches. Urogenital sinus is subject to obligatory surgical correction in all cases. Among the forms of hypospadias due to urethral malformation, obligatory surgical treatment is indicated in the total form. Vestibular and vestibulovaginal forms are subject to correction when urinary tract infection cannot be conservatively controlled. The newly proposed classification of hypospadias in girls is based on the current concepts of sex formation disorder and surgical management strategy:
1. Hypospadias due to urethral malformations
a) Vestibular;
b) Vestibulovaginal;
c) Total.
2. Hypospadias due to virilization of the external genitalia
a) Urogenital sinus
1) Mild form;
2) Medium form;
3) Severe form.
b) Low-vaginal ectopia of the external urethral opening
c) High-vaginal ectopia of the external urethral opening.
Discussion
The classification of female hypospadias, proposed by gynecologists in 2004, represents the most fully the spectrum of this malformation [1]. This classification of anatomic variants of female hypospadias includes low vaginal ectopia of the external urethral opening; high vaginal ectopia of the external opening of the urethra; urovaginal (vesicovaginal) fusion of the neck of the urinary bladder by the vagina accompanied with enuresis. The classification also contains forms of hypospadias, which are formulated as urogenital sinus in women and a combination of ectopy of the external urethra in women with impaired sex formation (in the original "in women with hermaphroditism"). The last two items of the classification do not correspond to the currently accepted terminology and current understanding of DSD. In accordance with the international consensus on the revision of terminology and classification of hermaphroditism, the use of the generalized term "hermaphroditism" to describe all conditions of sex development disorders is now unacceptable. It has been suggested that both the term "hermaphroditism" itself, which sounds offensive to patients, and the indication in the diagnosis of gender, ie male or female hermaphroditism, should be replaced. The term "disorders of sex development" (DSD) is recommended (4). [4].
The inclusion of UGS in the classification of female hypospadias is rational because it can identify the presence of two features characteristic of female hypospadias - ectopia of the external urethral opening and urethral shortening. A distinctive feature of the pathological structure of the external genitalia in patients with UGS is the inability to visualize the external urethral opening on the perineum during clinical examination, since it is located deep in the pelvis at the junction of the urethra and vagina. Urethral shortening also occurs in patients with UGS. The available literature reports reference values for urethral length in healthy female patients between 6 and 36 months of age. A study of 91 women with cystourethrography determined the minimum urethral length sufficient to provide a retention mechanism for urinary tract reconstruction in girls with UGS and cloaca. The mean urethral length for patients aged 6–12 months 12–24 months, and 24–36 months was 2.50, 2.31, and 2.59 cm, respectively [6]. The structure of the urethral tract in 30 girls with UGS due to CAH was reported in a study in Egypt [7]. The mean urethral length between 6 and 42 months of age, comparable to the previous study, was 2.2 cm. Urethral length was inversely correlated with the severity of UGS. Patients with a shorter urethral length of 1.0-1.5 cm required a more complex intervention. Conversely, patients with larger urethral lengths of 1.5–2.5 cm underwent a simple flap graft. A meta-analysis of these studies reported urethral shortening in girls with UGS due to CAH. Based on this and taking into account the nature of virilization of the external genitalia as a result of intrauterine exposure to androgens on the fetal urogenital sinus, we can assume that impaired involution of the fetal urogenital sinus causes not only abnormal vaginal development, but also urethral shortening characteristic of hypospadias.
The classification of hypospadias in women considers UGS without classifying them into its forms. The justification for this formulation was the management strategy adopted by the authors for the surgical correction of UGS [1]. Regardless of the form, the UGS correction was performed in two stages. The first stage was introitoplasty with a skin flap without separation of the urinary and genital tracts. A wide vaginal opening was formed with preservation of hypospadias. At the second stage, hypospadias was eliminated by urethral transposition. At the current stage of development of surgery for virilized external genitalia, UGS is corrected in the first stage [8]. At the same time, the form of malformation is an important criterion in the choice of feminizing plastic surgery strategy. Patients with the mild form undergo perineal skin flap repair, patients with the moderate form undergo skin-mucosal flap repair, and patients with the severe form undergo urogenital mobilization [9]. Therefore, we consider it important to include the three listed forms of UGS in the classification of hypospadias. It may seem irrational to separate the forms of external urethral ectopy due to virilization of the external genitalia into a separate group. Because these forms are the result of iatrogenesis, that is, the use of introitoplasty without separation of the urinary and genital tracts, adopted in the previous stage of pediatric surgery and inappropriate for the correction of virilized external genitalia. However, because its use is still widespread in many domestic clinics, we should expect hypospadias with low and high ectopy of the external urethral opening due to virilized external genitalia to be encountered in the practice of pediatric surgeons and gynecologists in the foreseeable future.
Other congenital diseases of the urogenital organs, such as bicornuate uterus, vaginal atresia, and vaginal septum may be concurrent with female hypospadias [10]. The abnormal structure of the urogenital tract as a consequence of CAH during puberty can be accompanied by abnormal outflow of menstrual secretions in the form of hematocolpos and hematometra [8]. The incidence of urinary abnormalities in girls with CAH is significantly higher (21.2%) than in the general population (2-4%). They include vesicoureteric reflux grades 1 to 3, hydronephrosis, and renal duplication [11]. In our study, the percentage of concomitant malformations of MPP is significantly lower compared with the literature data (7%), which is due to the inclusion in the study of a limited number of patients with CAH (only those who had UGS).
Shortening of the urethra, an increase in urethral diameter, the urethra running directly into the vagina, or the close proximity of the external opening to the vagina and anal opening are factors that reduce the barrier function of the urethra and lead to urinary tract infection (UTI) [1, 5]. The most severe course of UTI in the form of pyelonephritis in the first months of life is observed in total hypospadias combined with congenital malformations of the upper urinary tract, the need for surgical correction of which arises. In our group, patients with total hypospadias in infancy were diagnosed and surgically treated for ureterohydronephrosis. The asymptomatic course of UTI in patients with vestibular and vestibulovaginal forms of hypospadias due to urethral malformation determines their late diagnosis. The manifestation of chronic recurrent cystitis occurs in young women and is due to the beginning of sexual activity [12]. In our study, all patients with these forms of hypospadias had manifestations of urinary tract infection. The indication for urethral transposition in our study was recurrent UTI in one case in a girl with vestibulovaginal form concurrent with neurogenic bladder dysfunction, and due to postcoital cystitis in two patients with vestibular form of hypospadias who had experienced sexual intercourse.
Conclusion
The classification of hypospadias proposed in 2004 is acceptable for use in pediatric surgery because it encompasses the widest range of malformations. However, it is inconsistent with the current understanding of DSD, currently accepted terminology, and current surgical management strategy for UGS. The strategy adopted at the current stage of pediatric surgery suggests a single-stage correction of UGS, which significantly improves the quality of treatment of this complex malformation. We proposed modern formulations to describe the forms of hypospadias, and one of them in the form of UGS is supplemented with three forms. The new classification will help determine the rational surgical management strategy for hypospadias in girls and will facilitate the interaction of physicians of different specialties.
References
- Деревянко И.М., Рыжков Т.И., Елисеева В.В. Влагалищная эктопия уретры и мочеполовой синус у женщин. Ставрополь; 2004. 195c. [Derevyanko I.M., Ryzhkov T.I., Eliseeva V.V. Vaginal ectopia of the urethra and genitourinary sinus in women. Stavropol; 2004. 195 p. (in Russian)].
- Соловьев А.Е. Диагностика и лечение гипоспадии у девочек. Урология и нефрология. 1993; 6: 11-3. [Solovyev A.E. Diagnosis and treatment of hypospadias in girls. Urology and nephrology. 1993; 6: 11-3. (in Russian)].
- Мираков К.К., Володько Е.А., Окулов А.Б., Годлевский Д.Н., Аникиев А.В., Поварнин О.Я. Лапароскопия в диагностике и лечении нарушений формирования пола у детей. Medicus. 2016; 2: 122-4. [Mirakov K.K., Volodko E.A, Okulov A.B., Godlevskiy D.N., Anikiev A.V., Povarnin O.Ya. Laparoscopic surgery in diagnostics and treatment of sexual development disorders in children. Medicus. 2016; 2(8): 122-4. (in Russian)].
- Lee P.A., Houk C.P.б Ahmed S.F., Hughes I.A. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. Pediatrics. 2006; 118(2): e488-500. https://dx.doi.org/10.1542/peds.2006-0738.
- Комяков Б.К., Тарасов В.А. Способ хирургического лечения гипермобильности и влагалищной эктопии уретры. Патент на изобретениеRU 2686948 C1, Бюллетень Роспатента № 13, 06.05.2019. [Komyakov B.K., Tarasov V.A. Method of surgical treatment of hypermobility and vaginal ectopia of the urethra. Patent for invention RU 2686948 C1, Bulletin of RospatentNo. 13, 06.05.2019. (in Russian)].
- Halleran D.R., Thompson B., Fuchs M., Vilanova-Sanchez A., Rentea R.M., Bates D.G. et al. Urethral length in female infants and its relevance in the repair of cloaca. J. Pediatr. Surg. 2019; 54(2): 303-6. https://dx.doi.org/10.1016/j.jpedsurg.2018.10.094.
- Marei M.M., Fares A.E., Abdelsattar A.H., Abdullateef K.S., Seif H., Hassan M.M. et al. Anatomical measurements of the urogenital sinus in virilized female children due to congenital adrenal hyperplasia. J. Pediatr. Urol. 2016; 12(5): 282.e1-282.e8. https://dx.doi.org/10.1016/j.jpurol.2016.02.008.
- Адамян Л.В., Курило Л.Ф., Макиян З.Н., Поддубный И.В., Окулов А.Б., Глыбина Т.М., Глыбина Т.М., Файзуллин А.К. Тактика реконструктивно-пластических операций у пациенток с нарушениями формирования пола (disorders of sex development), отнесенных к женскому полу. Андрология и генитальная хирургия. 2010; 3: 56-62. [Adamyan L.V., Kurilo L.F.,Makiyan Z.N., Poddubniy B.V., Okulov A.B., Glybina T.M., Fayzullin A.K.The feminization surgical correction of patient with disorders of sexdevelopment. Andrology and genital surgery. 2010; 3: 56-62. (in Russian)].
- Аникиев А.В., Володько Е.А., Бровин Д.Н., Калинченко Н.Ю., Туманян Г.Т., Окулов А.Б. Дифференцированный подход к лечению гипоспадии у девочек. Вопросы гинекологии, акушерства и перинатологии. 2019; 18(4): 5-11. [Anikiev A.V., Volodko E.A., Brovin D.N., Kalinchenko N.Yu., Tumanyan G.T., Okulov A.B. Differentiated approach to the treatment of hypospadias in girls. Issues of gynecology, obstetrics and perinatology. 2019; 18(4): 5-11. (in Russian)].https://dx.doi.org/10.20953/1726-1678-2019-4-5-11.
- Knight H.M., Philip N.J., Mouriquand P.D. Female hypospadias: a case report. J. Pediat. Surg.1995; 30(12): 1738-40.
- Nabhan Z.M., Eugster E.A. Upper-tract genitourinary malformations in girls with congenital adrenal hyperplasia. Pediatrics. 2007; 120(2): e304-7.https://dx.doi.org/10.1542/peds.2006-2993.
- Рудин Ю.Э., Марухненко Д.В., Гарманова Т.Н. Гипоспадия у женщин и девочек: обзор литературы и клинический случай. Экспериментальная и клиническая урология. 2015; 4: 110-4. [Rudin Yu. E., Marukhnenko D.V., Garmanova T.N. Hypospadias in women and girls: a literature review and clinical case. Experimental and clinical urology. 2015; 4: 110-4. (in Russian)].
Received 19.04.2022
Accepted 05.07.2022
About the Authors
Alexander V. Anikiev, PhD, Surgeon at the Pediatric Surgery Department, National Medical Research Center for Endocrinology, Ministry of Health of Russia,+7(916)510-16-43, anikieal70@gmail.com, https://orcid.org/0000-0002-6448-6842, 117036, Russia, Moscow, Dmitry Ulyanov str., 11.
Dmitriy N. Brovin, PhD, Head of the Pediatric Surgeon Department, National Medical Research Center for Endocrinology, Ministry of Health of Russia, brovin-dn@yandex.ru,
https://orcid.org/0000-0002-3734-6510, 117036, Russia, Moscow, Dmitry Ulyanov str., 11.
Alexey B. Okulov, Dr. Med. Sci., Professor at the Pediatric Surgery Department, Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, okulov20@yandex.ru, https://orcid.org/0000-0002-8921-2856, 125993, Russia, Moscow, Barrikadnaya str., 2/1 b.1.
Elena A. Volodko, Dr. Med. Sci., Professor at the Pediatric Surgery Department, Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, okulov20@yandex.ru, https://orcid.org/0000-0002-4667-214X, 125993, Russia, Moscow, Barrikadnaya str., 2/1 b.1.
Elena N. Andreeva, Dr. Med. Sci., Professor at the Reproductive Medicine and Surgery Department, A.I. Yevdokimov Moscow State University of Medicine and Dentistry,
Ministry of Health of Russia, endogin@mail.ru, https://orcid.org/0000-0002-5949-1815, 127473, Russia, Moscow, Delegatskaya str., 20 b. 1.
Natalya G. Mokrysheva, Corresponding Member of the RAS, Dr. Med. Sci., Professor, Director of the National Medical Research Center for Endocrinology,
Ministry of Health of Russia, nm70@mail.ru, https://orcid.org/0000-0002-9717-9742, SPIN: 5624-3875, 117036, Russia, Moscow, Dmitry Ulyanov str., 11.
Corresponding author: Alexander V. Anikiev, anikieal70@gmail.com
Authors' contributions: Andreeva E.N., Anikiev A.V., Mokrysheva N.G. – conception and design of the study; Anikiev A.V. – data collection and analysis; Anikiev A.V., Volodko E.N., Brovin D.N. – manuscript drafting; Andreeva E.N., Brovin D.N., Mokrysheva N.G. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Acknowledgements: The authors express their gratitude to Valentina A. Peterkova, Academician of the RAS, Dr. Med. Sci., Professor, Scientific Director of the Institute of Pediatric Endocrinology, for her attention to the work and to the management of the "Alpha Endo" program, the Philanthropic Development Fund "KAF" for the financial support in creating the operation schemes.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Anikiev A.V., Okulov A.B., Volodko E.A., Brovin D.N., Andreeva E.N.,
Mokrysheva N.G. New classification of hypospadias in girls
according to modern concepts of disorders of sexual development
and surgical management strategy.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 7: 88-95 (in Russian)
https://dx.doi.org/10.18565/aig.2022.7.88-95