Pregnancy outcomes after maternal COVID-19 vaccination during pregnancy: preliminary data
Sukhikh G.T., Dolgushina N.V., Shmakov R.G., Klimov V.A., Yarotskaya E.L., Petrova U.L.
COVID-19 significantly raises risk during pregnancy. Currently, available evidence suggests that pregnant women are more susceptible to COVID-19 than the general population [1]. Pregnant women with COVID-19 are at increased risk of severe illness, death, and adverse pregnancy outcomes [2–4]. The most effective way to prevent the disease is vaccination. Current research evidence suggests that approved COVID-19 vaccines are safe, effective, and unlikely to pose any dangers to pregnant women or fetuses [5]. National and international associations issued guidelines supporting COVID-19 vaccination in pregnant and lactating women [6]. In the Russian Federation, vaccination of pregnant women with the Gam-COVID-Vac (Sputnik V) vaccine has been permitted since June 2021. Results of animal preclinical studies suggest no adverse impact of the Gam-COVID-Vac vaccine on the course of pregnancy and fetal, embryonic, and prenatal development of offspring [7].
Objective: This study aimed to analyze pregnancy complications after maternal COVID-19 vaccination with domestic vaccines during pregnancy.
Materials and methods
The study analyzed medical records on 773 women vaccinated against COVID-19 during pregnancy. The data were provided by 26 regions of the Russian Federation, including that on 3 women from the Republic of Buryatia, 4 from the Republic of Altai, 7 from the Kabardino-Balkar Republic, 8 from the Republic of Kalmykia, 10 from the Republic of Karelia, 11 from the Republic Komi, 16 from the Republic of Tatarstan, 18 from the Udmurt Republic, 22 from Altai Krai, 25 from Primorsky Krai, 31 from Belgorod Region, 36 from Voronezh Region, 37 from Ivanovo Region, 40 from Kaluga Region, 44 from Kostroma Region, 46 from Kursk Region, 48 from Lipetsk Region, 58 from Penza Region, 63 from Samara Region, 67 from Smolensk Region, 69 from Tver Region, 71 from Tula Region, 75 from Trans-Baikal Krai, 76 from Yaroslavl Region, 89 from Yamalo-Nenets Autonomous Okrug, and 92 from Sevastopol.
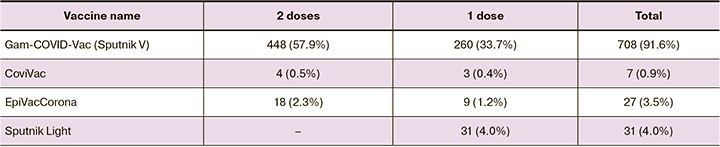
Most of the women were vaccinated with Gam-COVID-Vac (Sputnik V) vaccine (91.6%) and received two vaccine doses (57.9%).
Most of the patients were vaccinated in the first trimester of pregnancy, including 683 (88.4%), 51 (6.6%), and 39 (5%) before 12 weeks, from 12 to 22 weeks, and after 22 weeks of pregnancy, respectively.
Results
Pregnancy was completed in 157 (20.3%) of 773 women, and in 616 (79.7%), pregnancy continues to develop. Induced abortion before 12 weeks gestation at the woman's request was performed in 55 out of 773 women. In 24 women, pregnancy resulted in a full-term live birth. The term newborns were in satisfactory condition with a mean birth weight of 3300 g, Apgar score of 8–9, and were discharged home 4–5 days after delivery.
Ectopic pregnancy was diagnosed in 7 (0.9%) of 773 women. In 2020, the ectopic pregnancy rate in the Russian Federation was 2.6% of the total number of pregnancies [8, 9].
One woman gave birth to preterm twins. In 2020, the preterm birth rate in the Russian Federation was 5.9% of the total number of births [9]. During the COVID-19 pandemic, the preterm birth rate is 2–4 times higher and amounts to 14–25% [7].
Spontaneous miscarriage rate and fetal malformation rate were calculated for completed pregnancies above 22 weeks' gestation (n=488).
Spontaneous pregnancy loss before 22 weeks (spontaneous miscarriage or missed miscarriage) occurred in 65 women (13.3%), of whom 56 (86.2%) and 9 (13.8%) lost their pregnancies in the first and second trimester, respectively. In the population, 15–20% of all clinically diagnosed pregnancies end in miscarriage, 80% before 12 weeks of pregnancy [10]. During the COVID-19 pandemic, the incidence of spontaneous miscarriage was increased by 25% [11].
Fetal malformations were diagnosed in 5 women (1.1%). In 2020, in the Russian Federation induced abortion rate due to fetal malformations was 1.1% of the total number of pregnancies [9].
The incidence of COVID-19 in vaccinated patients was low. Sixteen women (2%) suffered COVID-19 during pregnancy, of whom in 15 (93.7%) and 1 (6.3%), the disease was mild and moderate, respectively.
Conclusion
The incidence of pregnancy complications after COVID-19 vaccination during pregnancy was no higher than in the population, and it was significantly lower than in women with COVID-19 during pregnancy. This observation emphasizes the need to vaccinate pregnant women to prevent adverse perinatal outcomes.
References
- Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I. Clinical course, maternal and perinatal outcomes of 2019 novel coronavirus infectious disease (COVID-19) in pregnant women in Siberia and Far East. Obstetrics and Gynecology. 2021; 2: 48-54. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.2.48-54.
- Jafari M., Pormohammad A., Sheikh Neshin S.A., Ghorbani S., Bose D., Alimohammadi S. et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021; 31(5): 1-16.e2208. https://dx.doi.org/10.1002/rmv.2208.
- Di Toro F., Gjoka M., Di Lorenzo G., De Santo D., De Seta F., Maso G. et al. Impact of COVID-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021; 27(1): 36-46. https://dx.doi.org/10.1016/j.cmi.2020.10.007.
- Liu H., Wang L.L., Zhao S.J., Kwak‐Kim J., Mor G., Liao A.H. Why are pregnant women susceptible to COVID‐19? An immunological viewpoint. J. Reprod. Immunol. 2020; 139: 103122. https://dx.doi.org/10.1016/j.jri.2020.103122.
- Shimabukuro T.T., Kim S.Y., Myers T.R., Moro P.L., Oduyebo T., Panagiotakopoulos L. et al. Preliminary findings of mRNA COVID-19 vaccine safety in pregnant persons. N. Engl. J. Med. 2021; 384(24): 2273-82. https://dx.doi.org/10.1056/NEJMoa2104983.
- https://www.rcog.org.uk/en/guidelines-research-services/coronavirus-covid-19-pregnancy-and-womens-health/covid-19-vaccines-and-pregnancy/
- Temporary methodological recommendations of the Ministry of Health of the Russian Federation "Organization of medical care for pregnant women, women in labor, maternity and newborns with a new coronavirus infection COVID-19". Version 4 (01.07.2021). (in Russian)].
- Statistical report form of the Ministry of Health of the Russian Federation No. 13 "Information on pregnancy with abortive outcome". (in Russian)].
- Statistical reporting form of the Ministry of Health of the Russian Federation No. 32 "Report on medical care for pregnant women, women in labor and maternity hospitals". (in Russian)].
- Russian Society of Obstetricians and Gynecologists (ROAG). Clinical recommendations "Miscarriage (spontaneous abortion)". 2021. (in Russian)].
- Sacinti K.G., Kalafat E., Sukur Y.E., Koc A. Increased incidence of first-trimester miscarriage during the COVID-19 pandemic. Ultrasound Obstet. Gynecol. 2021; 57(6): 1013-4. https://dx.doi.org/10.1002/uog.23655.
Received 17.11.2021
Accepted 19.11.2021
About the Authors
Gennady T. Sukhikh, MD, PhD, Professor, Academician of the Russian Academy of Sciences, Director of the V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-18-00, g_sukhikh@oparina4.ru, https://orcid.org/0000-0002-7712-1260, 117997, Russia, Moscow, Ac. Oparina str., 4.Nataliya V. Dolgushina, MD, PhD, Professor, Deputy Director – Head of the Department of Research and Development, V.I. Kulakov NMRC for OG&P,
Ministry of Health of Russia, +7(495)438-49-77, n_dolgushina@oparina4.ru, https://orcid.org/0000-0001-1116-138X, 117997, Russia, Moscow, Ac. Oparina str., 4.
Roman G. Shmakov, MD, PhD, Professor of the Russian Academy of Sciences, Head Specialist in Obstetrics of Ministry of Health of Russia, Director of the Institute
of Obstetrics, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-72-00, r_shmakov@oparina4.ru, https://orcid.org/0000-0002-2206-1002,
117997, Russia, Moscow, Ac. Oparina str., 4.
Vladimir A. Klimov, PhD, Head of the Medical care organization service, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(977)937-62-27,
Klimov12008@rambler.ru, https://orcid.org/0000-0002-4699-7614, 117997, Russia, Moscow, Ac. Oparina str., 4.
Ekaterina L. Yarotskaya, MD, PhD, Associate Professor, Head of the Department of International Cooperation, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-11-66, e_yarotskaya@oparina4.ru, https://orcid.org/0000-0003-0335-9660, 117997, Russia, Moscow, Ac. Oparina str., 4.
Uliana L. Petrova, PhD student, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(991)118-24-31, u_petrova@oparina4.ru,
https://orcid.org/0000-0003-0388-3104, 117997, Russia, Moscow, Ac. Oparina str., 4.
Aurthors' contributions: Shmakov R.G., Dolgushina N.V. – concept and design of the study, Dolgushina N.V., Klimov V.A. – collection and processing of the material, Dolgushina N.V. – writing the text, Yarotskaya E.L. – editing the text, Petrova U.L. – design of the article, Sukhoi G.T., Shmakov R.G. – final approval of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Acknowledgement: The authors express their gratitude to the chief non-staff specialists in obstetrics and gynecology and reproductive health of federal districts and subjects of the Russian Federation for their contribution to collecting data on vaccination of pregnant women.
For citation: Sukhikh G.T., Dolgushina N.V., Shmakov R.G.,Klimov V.A., Yarotskaya E.L., Petrova U.L. Pregnancy outcomes after maternal COVID-19 vaccination during pregnancy: preliminary data.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 11: 5-8 (in Russian)
https://dx.doi.org/10.18565/aig.2021.11.5-8