INDIVIDUAL APPROACH TO MICTONUTRIENT SUPPORT DURING PREGNANCY
Baranov I.I.
A woman’s body need for micronutrients during pregnancy naturally increase within the trimesters I to III. Since a woman must has to provide vitamins not only herself, but for the baby’s body, too, the women’s need for vitamins in the second half of pregnancy period increases by 10–50 %, and for some minerals — by 1.5–1.8 times [1].
Deficiency of vitamins and essential minerals during different periods of pregnancy affects organisms of a mother and her unborn baby variously. Vitamin and mineral deficiency during the first trimester of pregnancy may lead to abnormal development of a fetus and even to its death. Deficiency vitamins in the II and III trimesters can lead to intrauterine growth restriction and negatively influence the gestation course and pregnancy outcomes [2, 3].
Randomized studies showed that the use of folic acid 400–800 µg/day at least 4 weeks before conception and during the first 12 weeks of pregnancy reduces the neural tube defects risk. Administration of folic acid as part of multivitamin drugs enhanced this effect [4].
Simultaneously, according to numerous studies and the Cochrane meta-analysis, the use of vitamin mineral complexes during pregnancy contributes to normal gestation course and reduces the risks of some pregnancy complications, such as intrauterine development restriction syndrome and extremely premature birth (22–27 weeks of gestation) [2, 3, 5].
Vitamins deficiency, detected by their blood level, is observed in a significant part of the pregnant women surveyed, regardless of a season of the year and place of residence. According to modern studies, about 70–80% of women suffer from a combined deficiency of at once several micronutrients [6, 7].
At the same time, real clinical practice provides no method to diagnose deficiency of each separate vitamin. For this reason it is proposed to identify poly-/hypovitaminosis risk groups based on the history and routine laboratory tests (body mass index (BMI), hemoglobin level, age, and concomitant diseases). This approach allows to identify women that need therapeutic dosages of multivitamins to treat hypovitaminosis, as well as women with a low hypovitaminosis risk, for which it would be enough to use supplements to supply increased needs for vitamins and minerals.
Proceeding from the factors influencing the risk of hypovitaminosis, congenital malformations (СМ) and the complicated gestation course, it is reasonable to perform individual risk stratification and choose the method of micronutrient preventive treatment during planning, gestation and the puerperal period. The simplest indicators, such as age, BMI value, hemoglobin level, available within the routine practice of an obstetrician-gynecologist, allow distinguish high and low risk hypovitaminosis groups.
I. CM and hypovitaminosis low risk group. The group includes women not having a personal or family history of birth defects risks, without medical conditions and a burdened obstetric-gynecological history [8], who underwent preconceptional training and with normal study indicators: hemoglobin level 120 g/l, BMI within 18,5–30 kg/m2, with favourable living conditions and a versatile dietary intake.
To cover increased micronutrient needs, these women can use multivitamin complexes adapted for pregnant women, that will provide additional fortification with folic acid, calcium, iodine and vitamin D.
II. CM and hypovitaminosis low risk group.
The group includes women aged 35 years and over, with hemoglobin level under 120 g/l, BMI of over 30 kg/m2 or + less than 18.5 kg/m2, with clinical and historical risk factors for hypovitaminosis and/or congenital malformations + [8, 9]: +
- burdened obstetric-gynecological history: history of CM, recurrent miscarriage, impaired coagulation; +
- concurrent diseases impairing the metabolism of vitamins and minerals (gastrointestinal diseases, diabetes + mellitus type 1 and 2); +
- medications disrupting folate metabolism (carbamazepine, valproic acid, phenytoin, phenobarbital, methotrexate, triamteren, trimethoprim, colestyramine, etc.);
- poor lifestyle, dysnutrition: vegetarianism and other types of restrictive diets, bad health habits (smoking, alcohol ingestion), a sedentary lifestyle and insufficient exposure to sunlight.
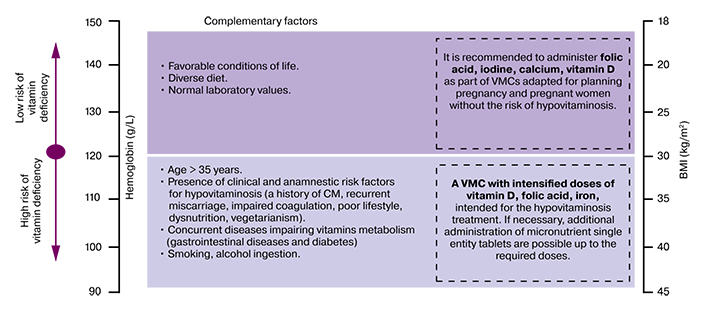
To reduce the perinatal risks associated with hypovitaminosis, it is recommended for these women to use multivitamin complexes adapted for the pregnant to treat hypovitaminosis, that will provide intensified dosages of folic acid, vitamin D, iron, and other micronutrients.
Comments
Age. Age 35 years and older is associated with an increase in the extragenital pathology amount, leading to higher complications incidence. Pregnant women over 35 years or older are susceptible an obstetric risk: significant increase of the rate of miscarriage and premature birth [10], birth of a low weight infant, arterial hypertension, gestational diabetes, presentation and placental abruption. Women over 35 years are also susceptible to an increased risk of congenital malformations and chromosomal abnormalities of a fetus. The risk of death due to pregnancy and childbirth is 2.5 times higher in 35–39 years old women, and 5.3 times higher after 40 years old ones compared to the 20–30 years of age category [11].
Hemoglobin. Measuring of hemoglobin level is a simple, widespread and recommended method to diagnose iron-deficient anemia. To confirm latent iron deficiency, serum ferritin measuring can be used as the most sensitive iron level indicator. Correlation between hemoglobin/iron levels and polyhypovitaminosis as well as the risk of complications during pregnancy and childbirth has been proven by plenty of studies [12–14].
BMI. Both excessive and insufficient BMI before and during pregnancy are associated with polyhypovitaminosis (of the liposoluble vitamins: D, A, E and other vitamins and minerals) [14–17], obstetric and perinatal complications. Pregnant patients with obesity (BMI ≥ 30 kg/m2) constitute a perinatal complications high risk group: spontaneous miscarriage, gestational diabetes mellitus, preeclampsia and hypertension disorders, premature birth, operative delivery, intrauterine and intranatal fetal death. The pregnant with a ≤ 185 kg/m2 BMI constitute a fetal growth retardation high risk group [17].
References
1. Guidelines MR 2.3.1.2432-08. Norms of Physiological Needs for Energy and Nutrients in Various Groups of Population of the Russian Federation. M., 2008.
2. Gromova O., Serov V., Torshin I., Kerimkulova N., Limanova O. Role of Vitamin-mineral Complexes Containing Folic Acid in Prevention of Congenital Heart Diseases and Neural Tube Defects. Efficient Pharmacotherapy. 2015; 4: 4–15.
3. Schaefer E. Micronutrient Deficiency in Women Living in Industrialized Countries During the Reproductive Years: Is there a Basis for Supplementation with Multiple Micronutrients? J Nutr Disorders Ther. 2016; 06. https://doi.org/10.4172/2161-0509.1000199.
4. Czeizel A.E. Primary Prevention of Neural-Tube Defects and Some Other Major Congenital Abnormalities: Recommendations for the Appropriate Use of Folic Acid During Pregnancy. Paediatric Drugs. 2000; 2: 437–49. https://doi.org/10.2165/00128072-200002060-00003.
5. Keats E.C., Haider B.A., Tam E., Bhutta Z.A. Multiple-micronutrient Supplementation for Women During Pregnancy. Cochrane Database of Systematic Reviews. 2019. https://doi.org/10.1002/14651858.CD004905.pub6.
6. Kodentsova V., Gmoshinskaya M., Vrzhesinskaya O. Vitamin and Mineral Complexes for Pregnant and Breastfeeding Women: Justification of Composition and Doses. Reproductive Health of Children and Teenagers. 2015; 62: 73–96.
7. Limanova O.A., Torshin I.Yu., Sardaryan I.S., Kalacheva A.G., Yudina N.V., Egorova E.Yu. Micronutrient Supply and Women's Health: Mining of Clinical and Epidemiological data. Issues of Gynecology, Obstetrics and Perinatology. 2014; 13: 5–15.
8. Wilson R.D., Genetics Committee, Wilson R.D., Audibert F., Brock J-A., Carroll J., et al. Pre-conception Folic Acid and Multivitamin Supplementation for the Primary and Secondary Prevention of Neural Tube Defects and Other Folic Acid-Sensitive Congenital Anomalies. J Obstet Gynaecol Can. 2015; 37: 534–52. https:// doi. org/10.1016/s1701-2163(15)30230-9.
9. FIGO Working Group on Best Practice in Maternal-Fetal Medicine, International Federation of Gynecology and Obstetrics. Best practice in maternal-fetal medicine. Int J Gynaecol Obstet. 2015; 128: 80–2. https://doi.org/10.1016/j.ijgo.2014.10.011.
10. Ciancimino L., Lagana A.S., Chiofalo B., Granese R., Grasso R., Triolo O. Would It Be Too Late? A Retrospective Case-control Analysis to Evaluate Maternal-fetal Outcomes in Advanced Maternal Age. Arch Gynecol Obstet. 2014; 290: 1109–14. https://doi.org/10.1007/s00404-014-3367-5.
11. Geller S.E., Cox S.M., Callaghan W.M., Berg C.J. Morbidity and Mortality in Pregnancy: Laying the Groundwork for Safe Motherhood. Womens Health Issues. 2006; 16: 176–88. https://doi.org/10.1016/j.whi.2006.06.003.
12. Smith E.M., Alvarez J.A., Martin G.S., Zughaier S.M., Ziegler T.R., Tangpricha V. Vitamin D Deficiency Is Associated with Anaemia Among African Americans in a US Cohort. Br J Nutr. 2015; 113: 1732–40. https://doi.org/10.1017/S0007114515000999.
13. Khurshid M., Molla A. M., Badruddin S. H., Snyder J. D., Hendricks K., Molla A. Is Anemia an Accurate Predictor of Vitamin A Status in Pakistani Children? The American Journal of Tropical Medicine and Hygiene. 1993; 49: 276–9. https://doi.org/10.4269/ajtmh.1993.49.276.
14. Goetz L.G., Valeggia C. The Ecology of Anemia: Anemia Prevalence and Correlated Factors in Adult Indigenous Women in Argentina: GOETZ and VALEGGIA. Am J Hum Biol. 2017; 29. e22947. https://doi.org/10.1002/ajhb.22947.
15. Thomas-Valdés S., Tostes M. das G.V., Anunciação P.C., da Silva B.P., Sant’Ana H.M.P. Association Between Vitamin Deficiency and Metabolic Disorders Related to Obesity. Critical Reviews in Food Science and Nutrition. 2017; 57: 3332–43. https://doi.org/10.1080/10408398.2015.1117413.
16. Xanthakos S.A. Nutritional Deficiencies in Obesity and After Bariatric Surgery. Pediatric Clinics of North America. 2009; 56: 1105–21. https://doi.org/10.1016/j. pcl.2009.07.002.
17. “Physiological Pregnancy” Clinical Practice Guidelines, 2019.