PATIENTS WITH PELVIC FLOOR DYSFUNCTION IN THE POSTPARTUM PERIOD
Dobrokhotova Yu.E., Nagieva T.S., Il’ina I.Yu.
Definition: Pelvic floor dysfunction (PFD) is understood to mean a complex of disorders in the function of the ligamentous apparatus and the muscles of the pelvic floor that hold the pelvic organs in a normal position and ensure the retention of urine and feces [1].
ICD-10 code: O34.8
Relevance of the research problem
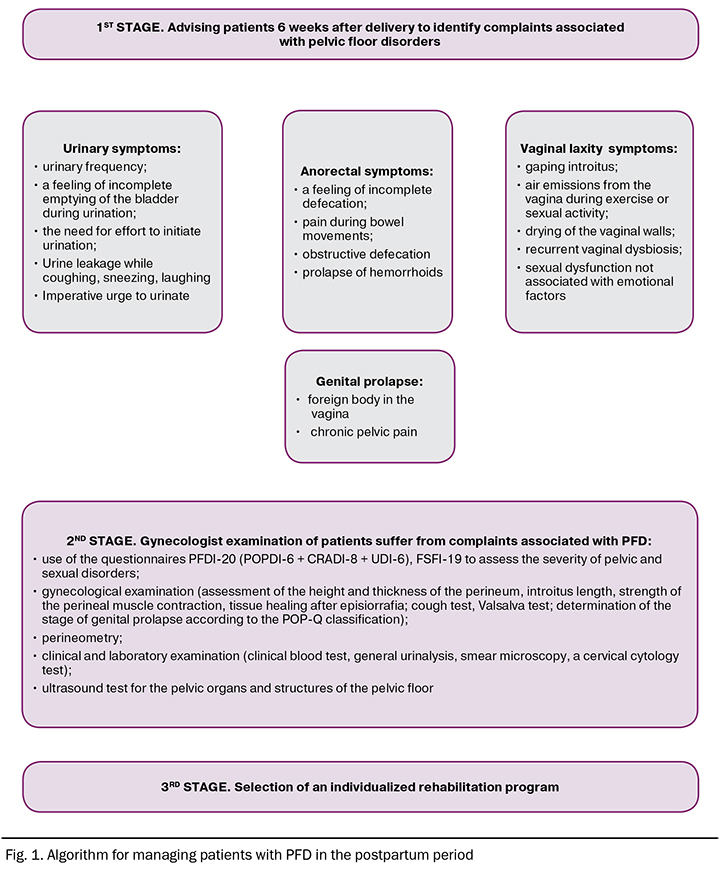
The first 6 weeks after birth is the most vulnerable period in a woman’s life in terms of the formation and / or progression of pelvic floor dysfunction [2]. Overstretching of the ligaments, defects of the pelvic fascia, including those not diagnosed, perineal injuries contribute to the development of impaired functioning of the pelvic organs. Genital prolapse, urinary incontinence, anal incontinence, pelvic pain, sexual dysfunction – these are the main clinical manifestations of pelvic floor dysfunction that need timely prevention and correction [3]. Currently, there is no universally accepted standardized approach to the management of patients with pelvic floor failure in the postpartum period. We made an attempt to generalize the experience of examination and treatment of such patients existing in scientific practice (Fig. 1).
Individual rehabilitation plan
Pelvic floor dysfunction (PFD) symptoms require a comprehensive and individual approach. Urinary incontinence is a serious problem due to the differential diagnosis of various types of urinary incontinence, and requires an interdisciplinary approach involving both gynecologists and urologists. A professional tandem is also justified if patients have phenomena of anal incontinence, requiring the involvement of a proctologist's patient in the examination and treatment of this cohort.
Research methods for patients in the postpartum period should include a thorough medical history taking, analysis of complaints associated with insufficiency of the pelvic floor and supporting structures of the pelvic organs. Gynecological examination involves an assessment of the thickness, extensibility and height of the perineum; the presence of cicatricial changes, gaping of the genital fissure and / or genital prolapse. Staging of genital prolapse relies on the POP-Q (Pelvic Organ Prolapse Quantification) system that based on an assessment of the location of the vaginal walls and cervix in relation to the hymenal ring [4]. Distance measurement is carried out by means of a uterine probe with a centimeter graduation and a ruler.
It is advisable to evaluate the results of specialized questionnaires to determine the effect of PFD symptoms on the quality of life in patients with genital prolapse [5]. An example of such a questionnaire is the PFDI-20 questionnaire, which includes 20 questions distributed in 3 blocks: POPDI-6 (Pelvic Organ Prolapse Distress Inventory) – for analyzing complaints associated directly with genital prolapse, CRADI-8 (Colorectal-Anal Distress Inventory) – to assess anorectal symptoms and UDI-6 (Urinary Distress Inventory) – to detect urinary disorders. Measuring sexual quality of life, taking into account parameters such as desire, arousal, lubrication, orgasm, satisfaction, and pain, is possible using the FSFI-19 questionnaire. The scatter of points is 0–36 [6].
In the arsenal of the obstetrician-gynecologist, a wide range of methods for the correction and prevention of pelvic dysfunction with an extensive evidence base. Thus, the effectiveness of the gynecological pessary in correcting genital prolapse and urinary disorders is widely reported in the scientific literature [7]. In our opinion, the use of this technique is effective and justified in patients in the postpartum period with stage II and higher genital prolapse and / or in the presence of symptomatic stage I genital prolapse in patients with unrealized reproductive plans. Sexual dysfunction caused by increased dryness of the vagina, cicatricial changes in the tissues of the urogenital tract can be eliminated by the local use of various types of energy, or estrogen-containing agents. But the use of ablative effects and / or hormonal agents in patients in the postpartum period is sharply limited. Hardware methods of exposure should be used no earlier than 2 months after delivery, giving preference to non-ablative methods of exposure, in particular, radio wave (RF) therapy [9]. The non-ablative radio wave effect on the tissues of the vulva and vagina consists in stimulating collagenogenesis, intensifying tissue regeneration, and improving microcirculation under the influence of high-frequency electric current [10].
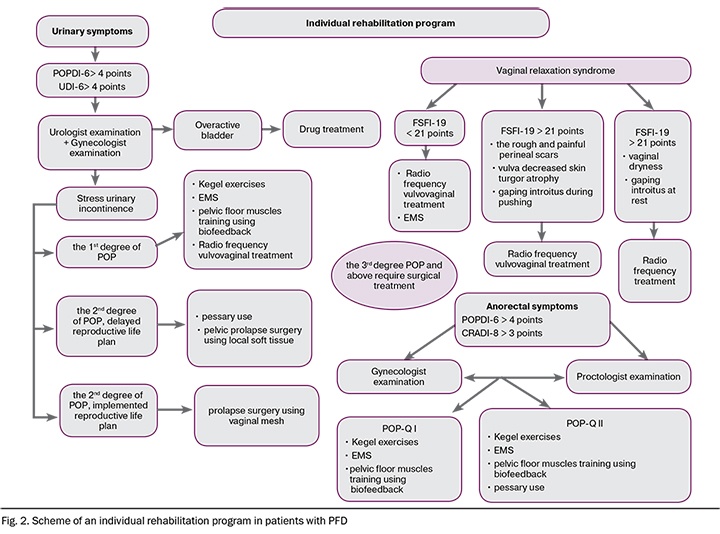
To summarize the foregoing, we offer the personified approach to the rehabilitation in the postpartum patients with PFD (Fig. 2)
References
1. Apolikhina I.A., Dodova E.G., Borodina E.A. et al. Pelvic floor dysfunction: modern principles of diagnostics and treatment. Effective pharmacotherapy. 2016; 22:16–23. (In Russ.).
2. Dobrokhotova Yu.E., Nagieva T.S. Pelvic floor dysfunction in women of the reproductive period, relaxed vaginal syndrome – the need for rehabilitation in the postpartum period. Russian Medical Journal. Mother and child. 2017; 5:1121-1124. (In Russ.).
3. Krasnopolskaya I.V. Pelvic floor dysfunction in women: clinical presentation, diagnosis, and principles of treatment. J. Obstetrics and gynecology. 2018; 2: 82–6. (In Russ.). doi: 10.18565/aig.2018.2.82-86.
4. Haylen B.T., Maher C.F., Barber M.D., Camargo S., Dandolu V., Digesu A., Goldman H.B., Huser M., Milani A.L., Moran P.A., Schaer G.N., Withagen M.I.J. An International Urogynecological Association (IUGA) / International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourology and Urodynamics 35:137–168 (2016).
5. Zuchelo LTS, Bezerra IMP, Da Silva ATM, Gomes JM, Soares Júnior JM, Chada Baracat E, de Abreu LC, Sorpreso ICE. Questionnaires to evaluate pelvic floor dysfunction in the postpartum period: a systematic review. Int J Womens Health. 2018 Aug 8; 10: 409-424. doi: 10.2147/IJWH.S164266.
6. Neijenhuijs K.I., Hooghiemstra N., Holtmaat K., Aaronson N.K., Groenvold M., Holzner B., Terwee C.B., Cuijpers P., Verdonck-de Leeuw I.M. The Female Sexual Function Index (FSFI)-A Systematic Review of Measurement Properties. J Sex Med. 2019 May; 16(5): 640-660. doi: 10.1016/j.jsxm.2019.03.001.
7. Rantell A. Vaginal Pessaries for Pelvic Organ Prolapse and Their Impact on Sexual Function. Sexual Medicine Reviews. 2019. doi:10.1016/j.sxmr.2019.06.002.
8. Hadizadeh-Talasaz Z., Sadeghi R., Khadivzadeh T. Effect of pelvic floor muscle training on postpartum sexual function and quality of life: A systematic review and meta-analysis of clinical trials. J Obstet Gynecol. 2019 Nov; 58(6): 737-747. doi: 10.1016/j.tjog.2019.09.003.
9. Dobrokhotova Yu.E., Nagieva T.S., Ilyina I.Yu., Kareva E.N., Kochina N.A., Zragus E.V., Dobrova A.B., Shakhmaratova I.A., Krasnoshchok E.V. Radiofrequency non-ablative effects on the expression of the connective tissue proteins of the urogenital tract in patients with relaxed vaginal syndrome in the postpartum period. J. Obstetrics and gynecology. 2019; 8:119-25. (In Russ.). doi: 10.18565/aig.2019.8.119-125.
10. Digesu G.A., Tailor V., Preti M., Vieira-Baptista P., Tarcan T., Stockdale C., Mourad S. The energy based devices for vaginal "rejuvenation," urinary incontinence, vaginal cosmetic procedures, and other vulvo-vaginal disorders: An international multidisciplinary expert panel opinion. Neurourol. Urodyn. 2019 Mar; 38(3): 1005-1008. doi: 10.1002/nau.23927.